Navigating Complex Surgical Anatomy: A Case Report
Received: 28-Feb-2023, Manuscript No. ijav-23-6236; Editor assigned: 01-Mar-2023, Pre QC No. ijav-23-6236 (PQ); Accepted Date: Mar 21, 2023; Reviewed: 14-Mar-2023 QC No. ijav-23-6236; Revised: 21-Mar-2023, Manuscript No. ijav-23-6236 (R); Published: 28-Mar-2023, DOI: 10.37532/1308-4038.16(3).246
Citation: Hvizdosova N. Navigating Complex Surgical Anatomy: A Case Report. Int J Anat Var. 2023;16(3):265-266.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The success of surgical procedures depends on a comprehensive understanding of the anatomical structures involved. However, in some cases, the surgical anatomy can be complex, posing challenges for the surgical team. In this case report, we present a case of a 56-year-old male who underwent a surgical procedure for a tumor located in a challenging anatomical location. The surgery required an in-depth knowledge of the anatomy of the surrounding structures and a meticulous surgical approach to avoid damage to vital structures. This case report highlights the importance of a thorough understanding of surgical anatomy, careful preoperative planning, and a multidisciplinary team approach to achieve successful outcomes in complex surgical cases.
Keywords
Surgical Anatomy; Neuroanesthesiologist; Neurosurgeon; Motor evoked potentials
INTRODUCTION
Surgical procedures require an intricate knowledge of the anatomy of the structures involved. While modern imaging techniques have improved the accuracy of preoperative planning, complex surgical anatomy can still pose significant challenges to the surgical team. A detailed understanding of the anatomy of the structures involved is crucial to ensure a safe and successful surgical outcome. In this case report, we present a case of a challenging surgical anatomy and the surgical approach used to navigate it. Navigating complex surgical anatomy is an important skill for surgeons, as it involves the ability to understand and manipulate intricate structures within the human body. Surgical procedures often require the surgeon to navigate through complex anatomy in order to reach the target organ or tissue and perform the necessary procedure [1].
To navigate complex surgical anatomy, surgeons must have a strong understanding of the human anatomy, including the location, function, and relationship between different organs and tissues. They must also possess technical skills and dexterity, as well as the ability to think critically and make quick decisions in high-pressure situations [2-3]. In addition to traditional surgical techniques, new technologies such as computer-assisted navigation systems and virtual reality simulations are emerging as tools to aid surgeons in navigating complex anatomy. These technologies can provide enhanced visualization and precision, allowing for more accurate and less invasive procedures.
Overall, navigating complex surgical anatomy is a challenging but essential component of surgical practice, requiring a combination of anatomical knowledge, technical skills, and innovation.
CASE REPORT
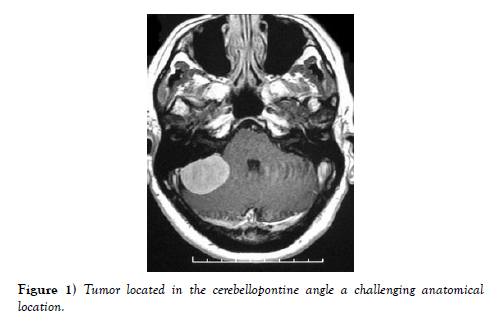
A 56-year-old male presented with a tumor located in the cerebellopontine angle, a challenging anatomical location due to the presence of critical structures such as the cranial nerves, blood vessels, and brainstem. The patient underwent preoperative imaging, which revealed the size and location of the tumor and the surrounding structures. The surgical team, consisting of a neurosurgeon, neuroanesthesiologist, and neurophysiologist, conducted a thorough preoperative planning session to discuss the surgical approach and the potential risks associated with the surgery [4-5] (Figure 1).
Figure 1: Tumor located in the cerebellopontine angle a challenging anatomical location.
During the surgery, the team used intraoperative monitoring techniques, including somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs), to ensure the safety of the surrounding structures. The neurosurgeon used a meticulous surgical approach to access the tumor, carefully dissecting the surrounding structures while avoiding damage to the cranial nerves and blood vessels. The surgery was successful, and the patient had no postoperative complications [6].
CONCLUSION
The success of surgical procedures depends on a comprehensive understanding of the anatomy of the structures involved. In complex surgical cases, preoperative planning and a multidisciplinary team approach are crucial to ensure a safe and successful outcome. This case report highlights the importance of a thorough understanding of surgical anatomy, careful preoperative planning, and a meticulous surgical approach in navigating complex surgical anatomy [7-9].
ACKNOWLEDGEMENT:
None
CONFLICTS OF INTEREST:
None.
References
- Kay LW. Some anthropologic investigations of interest to oral surgeons. Int J Oral Surg. 1974; 3(6):363-79.
- Agthong S, Huanmanop T, Chentanez V. Anatomical variation of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg. 2005; 63(6):800-804.
- Katakami K, Mishima A, Shiozaki K, Shimoda S, et al. Characteristics of accessory mental foramina observed on limited cone-beam computed tomography images. J Endod. 2008; 34(12):1441-1445.
- Sonick M, Abrahams J, Faiella RA. A comparison of the accuracy of periapical, panoramic, and computerized tomographic radiographs in locating the mandibular canal. Int J Oral Maxil-lofac Implants. 1994; 9:455-468.
- Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, et al. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107(2):289-294.
- Laurent de K, Stefano M. Variability of repairable bicuspid aortic valve phenotypes: towards an anatomical and repair-oriented classification. Eur J Cardiothorac Surg. 2019; 37(11):9-828.
- Jun S, Zhang-Y, Chuan C. Postoperative neovascularization, cerebral hemodynamics, and clinical prognosis between combined and indirect bypass revascularization procedures in hemorrhagic moyamoya disease. Clin Neurol Neurosurg. 2021 Sep; 208:106869.
- Qi L, Xiaojie T, Yafang D. Evaluation of Carotid Plaque Rupture and Neovascularization by Contrast-Enhanced Ultrasound Imaging: an Exploratory Study Based on Histopathology. Transl Stroke Res. 2021 Feb; 12(1):49-56.
- Kuo-Shyang J, Shu-Sheng L, Chiung-FC. The Role of Endoglin in Hepatocellular Carcinoma. Int J Mol Sci. 2021 Mar 22;22(6):3208
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref