Neuroanatomical Correlates of Motor Deficits in a Patient with Traumatic Brain Injury
Received: 03-May-2023, Manuscript No. ijav-23-6431; Editor assigned: 04-May-2023, Pre QC No. ijav-23-6431 (PQ); Accepted Date: May 22, 2023; Reviewed: 18-May-2023 QC No. ijav-23-6431; Revised: 22-May-2023, Manuscript No. ijav-23-6431 (R); Published: 29-May-2023, DOI: 10.37532/1308-4038.16(5).266
Citation: Hvizdosova N. Neuroanatomical Correlates of Motor Deficits in a Patient with Traumatic Brain Injury. Int J Anat Var. 2023;16(5):308-309.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This case report examines the neuroanatomical correlates of motor deficits in a patient who sustained a traumatic brain injury (TBI). The patient presented with hemiparesis and impaired coordination following a motor vehicle accident. Neuroimaging studies, including computed tomography (CT) and magnetic resonance imaging (MRI), were performed to assess the extent of structural brain damage and identify the underlying neural substrates responsible for the motor deficits. The findings revealed lesions in the corticospinal tract, primary motor cortex, and basal ganglia, highlighting the importance of understanding the neuroanatomical basis of motor function in patients with TBI. The case report emphasizes the significance of accurate diagnosis and tailored rehabilitation strategies based on neuroanatomical principles for optimal patient outcomes.
Keywords
Traumatic brain injury, Motor deficits, Neuroanatomy, Corticospinal tract, Primary motor cortex, Basal ganglia, Neuroimaging
INTRODUCTION
Traumatic brain injury (TBI) is a significant public health concern worldwide, often leading to long-term disabilities, including motor deficits. The severity and localization of motor impairments in patients with TBI can vary depending on the nature and extent of brain damage. Understanding the neuroanatomical basis of motor function is crucial for accurate diagnosis and effective rehabilitation interventions. This case report aims to examine the neuroanatomical correlates of motor deficits in a patient with TBI, highlighting the importance of integrating neuroanatomical knowledge into clinical practice [1].
CASE REPORT
A 42-year-old male was admitted to the emergency department following a motor vehicle accident. Upon arrival, he presented with left-sided weakness, predominantly affecting the upper extremity, and impaired coordination. The patient had a Glasgow Coma Scale score of 14/15, indicating mild traumatic brain injury. Initial clinical assessment revealed signs of hemiparesis and mild spasticity in the affected limb [2].
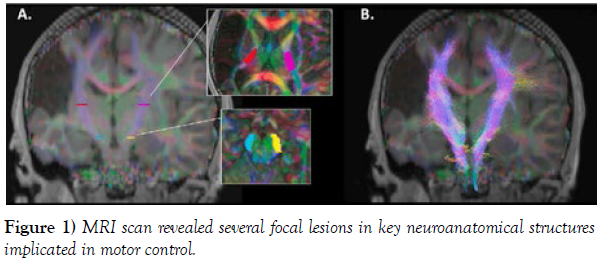
Neuroimaging Findings: The patient underwent CT and MRI scans to assess the structural brain damage associated with the motor deficits. The CT scan revealed no evidence of acute intracranial hemorrhage or skull fractures. However, the MRI scan revealed several focal lesions in key neuroanatomical structures implicated in motor control (Figure 1).
1. Corticospinal Tract (CST): A focal lesion was observed in the posterior limb of the internal capsule on the right side, consistent with damage to the descending motor pathway known as the corticospinal tract. This pathway carries motor signals from the primary motor cortex to the spinal cord and is crucial for voluntary motor control. Disruption of the CST can result in contralateral motor deficits, as observed in the patient’s leftsided weakness.
2. Primary Motor Cortex: Further examination of the MRI scans revealed a small area of cortical contusion in the right precentral gyrus, corresponding to the primary motor cortex (M1). The primary motor cortex plays a vital role in motor planning and execution, with specific areas corresponding to different body parts. Damage to the primary motor cortex can lead to motor deficits, including weakness, impaired coordination, and altered muscle tone. The contusion in the right precentral gyrus likely contributed to the patient’s left-sided hemiparesis.
3. Basal Ganglia: The MRI scans also revealed bilateral basal ganglia abnormalities. The basal ganglia are a group of subcortical structures involved in motor control and movement regulation. In this patient, there was evidence of hemorrhagic lesions in the right caudate nucleus and left putamen. Dysfunction or damage to the basal ganglia can lead to movement disorders and motor deficits. The observed lesions in the basal ganglia could contribute to the coordination difficulties and abnormal muscle tone observed in the patient.
Neuroanatomical Correlates of Motor Deficits: The neuroimaging findings in this case indicate that the patient’s motor deficits can be attributed to damage in multiple key neuroanatomical structures involved in motor control. The lesions in the corticospinal tract, primary motor cortex, and basal ganglia provide insights into the underlying pathophysiology of the observed motor impairments.
The disruption of the corticospinal tract, as evidenced by the lesion in the posterior limb of the internal capsule, explains the contralateral hemiparesis. The descending motor signals from the primary motor cortex are unable to reach the spinal cord, resulting in weakness and spasticity in the affected limb [3]. The contusion in the right precentral gyrus, corresponding to the primary motor cortex, further contributes to the patient’s motor deficits. Damage to this region disrupts the precise control of voluntary movements, leading to impaired coordination and difficulty executing motor tasks.
The presence of hemorrhagic lesions in the basal ganglia, particularly in the caudate nucleus and putamen, suggests dysfunction in these subcortical structures. The basal ganglia play a crucial role in the regulation of movement and coordination by modulating the activity of the motor cortex. Damage to the basal ganglia can result in movement disorders and abnormal muscle tone, which aligns with the patient’s observed coordination difficulties and spasticity.
Implications for Diagnosis and Rehabilitation: Understanding the neuroanatomical basis of motor deficits in patients with TBI is vital for accurate diagnosis and targeted rehabilitation interventions. In this case, the identification of specific lesions in the corticospinal tract, primary motor cortex, and basal ganglia provides valuable information for treatment planning [4-5].
DISCUSSION
Accurate diagnosis of the underlying neuroanatomical damage can guide the development of individualized rehabilitation strategies. For example, rehabilitation efforts should focus on promoting neural plasticity and facilitating compensatory mechanisms to bypass the disrupted corticospinal tract. Additionally, interventions targeting the primary motor cortex and basal ganglia can help improve motor coordination and normalize muscle tone.
Furthermore, knowledge of the neuroanatomical correlates of motor deficits can aid in prognostication and predicting the potential for functional recovery. It allows healthcare professionals to communicate realistic expectations to patients and their families, promoting informed decisionmaking and effective long-term care planning [6-7].
CONCLUSION
This case report highlights the importance of integrating neuroanatomical knowledge into the clinical assessment and management of patients with TBI and motor deficits. The neuroimaging findings demonstrate the involvement of specific neuroanatomical structures, including the corticospinal tract, primary motor cortex, and basal ganglia, in the observed motor impairments. Understanding the neuroanatomical basis of motor deficits enables accurate diagnosis, tailored rehabilitation strategies, and informed prognostication, ultimately leading to improved patient outcomes.
CONFLICTS OF INTEREST
None.
REFERENCES
- Veltman CE, van der Hoeven BL, Hoogslag GE, Boden H, Kharbanda RK, et al. Influence of coronary artery dominance on short- and log-term outcomes in patients after ST-segment elevation myocardial infarction. Eur Heart J. 2015; 36:1023-1030.
- Galiuto L. How to access functional significance of myocardial bridging in athletes: a personalized medicine approach. Biomed J Sci & Tech Res. 2020; 26(2): 004-313.
- Navarro A, Sladden D, Casha A, Manche A. The difficulty in identifying and grafting an intramuscular coronary artery. Malta Med J. 2019; 3(1):14-16.
- Ibarrola M. Myocardial bridge a forgotten condition: A review. Clin Med Img Lib. 2021; 7:182.
- Jiang L, Zhang M, Zhang H, Shen L, Shao L, et al. A potential protective element of myocardial bridge against severe obstructive atherosclerosis in the whole coronary system. BMC Cardiovasc Disord. 2018; 18(1):105.
- Aricatt DP, Prabhu A, Avadhani R, Subramanyam K, Ezhilan J, et al. A study of coronary artery dominance and its clinical significance. Folia Morphol. 2023; 82(1): 102-107.
- Abu-Assi E, Castineira-Busto M, Gonzalez-Salvado V, Raposeiras-Roubin S, Abumuaileq RR-Y, et al. Coronary artery dominance and long-term prognosis in patients with ST-segment elevation myocardial infarction treated with primary angioplasty. Rev Esp Cardiol. 2016; 69(1):19-27.
Indexed at , Indexed at , Crossref
Indexed at, Indexed at , Crossref
Indexed at , Indexed at , Crossref
Indexed at , Indexed at , Crossref
Indexed at , Indexed at , Crossref