Neuroanatomy in Clinical Practice: A Comprehensive Case Report of a Patient with Neuroanatomical Disorder
Received: 04-Jun-2023, Manuscript No. ijav-23-6530; Editor assigned: 05-Jun-2023, Pre QC No. ijav-23-6530 (PQ); Accepted Date: Jun 23, 2023; Reviewed: 19-Jun-2023 QC No. ijav-23-6530; Revised: 23-Jun-2023, Manuscript No. ijav-23-6530 (R); Published: 30-Jun-2023, DOI: 10.37532/1308-4038.16(6).272
Citation: Karl M. Neuroanatomy in Clinical Practice: A Comprehensive Case Report of a Patient with Neuroanatomical Disorder. Int J Anat Var. 2023;16(6):319-320.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Neuroanatomy is a fundamental field in neuroscience that focuses on the study of the structure and organization of the nervous system. This case report aims to provide a comprehensive analysis of a patient with a neuroanatomical disorder, highlighting the importance of understanding Neuroanatomy in clinical practice. The report presents a detailed examination of the patient’s clinical history, neurological examination, and neuroimaging findings. Additionally, it discusses the underlying neuroanatomical structures and pathways affected in the patient, emphasizing the correlation between structural abnormalities and clinical manifestations. The case report underscores the significance of neuroanatomical knowledge for accurate diagnosis, treatment planning, and patient management in neurology.
Keywords
Neuroanatomy, Nervous system; Clinical practice; Neuroimaging; Neurological examination; Diagnosis; Treatment planning; Patient management
INTRODUCTION
Neuroanatomy is a fundamental discipline within the field of neuroscience that provides a comprehensive understanding of the structure and organization of the nervous system [1]. The intricate anatomy of the brain and spinal cord forms the basis for neurologic functioning, and any disruption in these structures can lead to significant clinical manifestations [2]. The ability to accurately diagnose and manage neurologic disorders relies heavily on a thorough understanding of Neuroanatomy. This case report presents a detailed analysis of a patient with a neuroanatomical disorder, highlighting the importance of neuroanatomical knowledge in clinical practice [3-4].
CASE REPORT
Clinical History a 45-year-old male presented with a three-month history of progressive weakness and sensory loss in the right upper and lower limbs. The patient reported no significant medical history, previous trauma, or family history of neurological disorders. He also denied any recent infections or exposure to toxins.
Neurological Examination: On examination, the patient exhibited reduced muscle strength (4/5) in the right upper and lower limbs compared to the left side. Sensory examination revealed decreased light touch and proprioception in the right limbs. Deep tendon reflexes were diminished on the right side. Cranial nerve examination, coordination, and gait were normal.
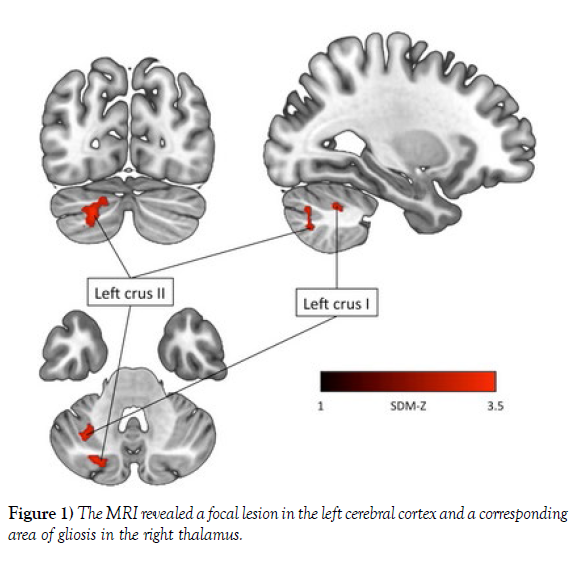
Neuroimaging Findings: Magnetic resonance imaging (MRI) of the brain and spine was performed to investigate the underlying cause of the patient’s symptoms. The MRI revealed a focal lesion in the left cerebral cortex and a corresponding area of gliosis in the right thalamus. Additionally, spinal cord imaging showed abnormal T2 hyper intensity involving the right dorsal columns at the cervical level (Figure 1).
DISCUSSION
Neuroanatomical Structures and Pathways: The patient’s clinical presentation, including weakness and sensory loss in the right limbs, suggests involvement of the corticospinal tract and the dorsal column-medial lemniscus pathway. The corticospinal tract, originating from the precentral gyrus, is responsible for the voluntary control of limb movements. Lesions affecting this pathway lead to contralateral weakness [5]. The dorsal column-medial lemniscus pathway carries fine touch, proprioceptive, and vibratory information from the periphery to the somatosensory cortex, damage to this pathway results in ipsilateral sensory deficits.
Correlation between Structural Abnormalities and Clinical Manifestations: The focal lesion in the left cerebral cortex observed on MRI explains the patient’s contralateral weakness [6]. The corticospinal tract fibers originating from the precentral gyrus cross in the medullary pyramids, resulting in contralateral motor deficits. The corresponding gliotic changes in the right thalamus suggest secondary degeneration due to trans-synaptic axonal injury.
The abnormal T2 hyper intensity in the right dorsal columns at the cervical level correlates with the patient’s ipsilateral sensory loss. This finding indicates disruption of the ascending fibers carrying sensory information from the limbs to the brain. The specific location of the lesion suggests involvement of the fasciculus gracilis and fasciculus cuneatus within the dorsal columnmedial lemniscus pathway [7].
Diagnosis and Treatment: Based on the clinical history, neurological examination, and neuroimaging findings, the patient was diagnosed with a neuroanatomical disorder affecting the left cerebral cortex, right thalamus, and right dorsal columns. Treatment options, including physical therapy and symptomatic management, were discussed with the patient. Regular followup visits were scheduled to monitor the patient’s progress and assess the effectiveness of the treatment plan [8-10].
CONCLUSION
This case report highlights the crucial role of Neuroanatomy in clinical practice, emphasizing the correlation between neuroanatomical structures and clinical manifestations. A comprehensive understanding of Neuroanatomy is essential for accurate diagnosis, treatment planning, and patient management in neurology. The integration of neuroimaging techniques with neuroanatomical knowledge provides valuable insights into the underlying pathophysiology of neurologic disorders, facilitating optimal patient care. Further research and advancements in Neuroanatomy will continue to enhance our understanding of the intricate workings of the nervous system and contribute to improved outcomes for patients with neuroanatomical disorders.
ACKNOWLEDGEMENT
None
REFERENCES
- Penprapa SK, Brianna KR. Duplication of the inferior vena cava: evidence of a novel type IV. Folia Med Cracov. 2020; 28; 60(2):5-13.
- Laurent de K, Stefano M. Variability of repairable bicuspid aortic valve phenotypes: towards an anatomical and repair-oriented classification. Eur J Cardiothorac Surg. 2019; 37(11):9-828.
- Jun S, Zhang-Y, Chuan C. Postoperative neovascularization, cerebral hemodynamics, and clinical prognosis between combined and indirect bypass revascularization procedures in hemorrhagic moyamoya disease. Clin Neurol Neurosurg. 2021; 208:106869.
- Qi L, Xiaojie T, Yafang D. Evaluation of Carotid Plaque Rupture and Neovascularization by Contrast-Enhanced Ultrasound Imaging: an Exploratory Study Based on Histopathology. Transl Stroke Res. 2021; 12(1):49-56.
- Kuo-Shyang J, Shu-Sheng L, Chiung-FC. The Role of Endoglin in Hepatocellular Carcinoma. Int J Mol Sci. 2021;22(6):3208.
- Anri S, Masayoshi O, Shigeru H. Glomerular Neovascularization in Nondiabetic Renal Allograft Is Associated with Calcineurin Inhibitor Toxicity. Nephron. 2020; 144 Suppl 1:37-42.
- Mamikonyan VR, Pivin EA, Krakhmaleva DA. Mechanisms of corneal neovascularization and modern options for its suppression. Vestn Oftalmo. 2016; 132(4):81-87.
- Brian M, Jared PB, Laura E. Thoracic surgery milestones 2.0: Rationale and revision. J Thorac Cardiovasc Surg. 2020 Nov; 160(5):1399-1404.
- Xin W, Bofu L. Aortic Dissection with Rare Anatomical Aortic Arch Variation Depicted by Computed Tomography Angiography. Heart Surg Forum. 2021; 24(2): E407-E408.
- Foivos I, Jonathon K, Daryll B. Aberrant right subclavian artery - a rare congenital anatomical variation causing dysphagia lusoria. Vasa. 2021; 504(5):394-397.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref