Nonrotation of the intestine: embryological and clinical correlation
Velavan SS* Castellanos B, Gulfam N and Rich S
Touro College of Osteopathic Medicine, New York, NY-10027, USA
- *Corresponding Author:
- Dr. Sumathilatha Sakthi Velavan
Touro College of Osteopathic Medicine
230 W 125th Street, New York
NY-10027, USA
Tel: +646 981-4629
E-mail: sumathilathads@yahoo.co.in
Citation: Velavan SS, Castellanos B, Gulfam N, Rich S. Nonrotation of the intestine: embryological and clinical correlation. Int J Anat Var. 2017;10(3):53-4.
Copyright: This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
[ft_below_content] =>Keywords
Malrotation; Nonrotation; Embryology; Midgut; Ladd’s band
Introduction
The Embryology of the gastrointestinal tract is complex and involves a particularly well-orchestrated rotation of midgut. The complex steps result in assembly of the parts of the gut in the normal anatomical location. Error at the stage of midgut rotation may result in an array of variations in the abdominal organs. The extreme form of malrotation of the midgut is non-rotation and is a very rarely reported variation with the incidence of less than 1:500 [1]. The completely altered architecture of the organs in the peritoneal cavity poses a surgical risk and deserves embryological reasoning. The aim of this study is to report an extremely rare anatomical variant. The altered arrangement of viscera is combined peritoneal relations also and hence may lead to complications such as intestinal obstruction, volvulus, and misdiagnosis. For the benefit associated with its clinical implications. This report might aid in the understanding of this anatomical variant and optimize patient management.
Case Report
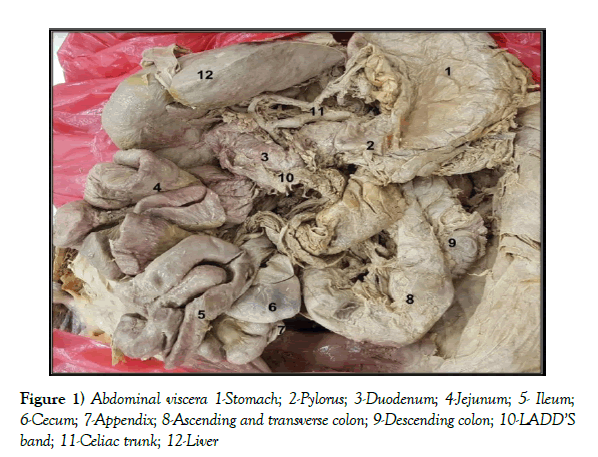
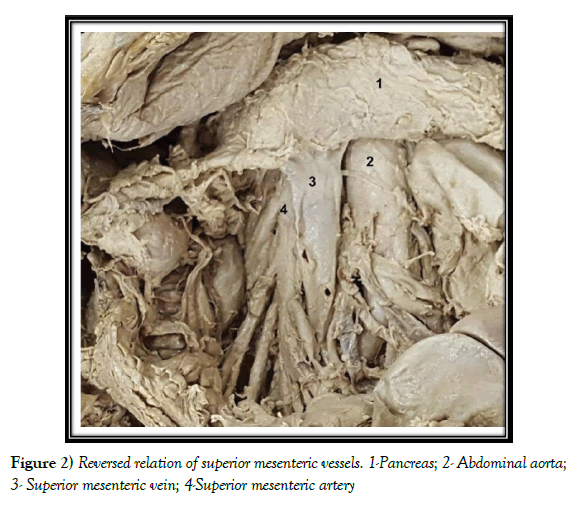
During routine dissection of the abdomen in a 93-Year old, Caucasian female cadaver, abnormal location of the small intestine was noted. The cadaver was donated and embalmed with formalin based on appropriate ethical principles. A detailed analysis of the intestines was done by tracing from pyloric end of the stomach to the rectum. The vasculature of the abdominal organs was dissected. The liver, pancreas, spleen and the genitourinary tract were dissected to note any variation. The Stomach was normal in a location with the pyloric end just to the right of the midline. The duodenum was oriented vertically, coiled, lacked its usual ‘C’ loop and to the right of the vertebral column. The entire small intestine was found to lie on the right side of the abdominal cavity. The duodenum was located to the right of the superior mesenteric artery and was not crossed by the artery. The superior mesenteric vein was found on the left side of the artery. Mesenteric root was short and was in the prevertebral region. The ileocecal junction was traced to the hypogastrium where cecum and appendix were situated. The ascending, transverse and descending colon formed a‘s’ shaped loop while sigmoid colon and rectum were normally located.
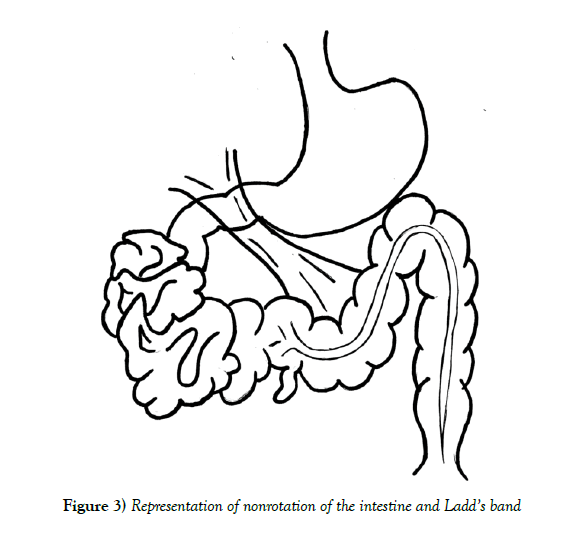
The left kidney was normal while the right kidney was located closer to the midline. A fibrous Ladd’s band was found to cross the duodenum to the cecum. It extended from the posterior abdominal wall, crossed and tightly held the intestines coiled and was found attached to the greater omentum and also to the cecum (Figures 1-3).
Discussion
Early in embryonic life, before approximately 4 weeks of gestation, the gut is a short, straight, featureless tube. By 12 weeks, it has grown rapidly and, after a series of complex steps involving a total rotation of 270°, has undergone fixation in the normal position in the abdomen [2,3]. First, the duodenum rotates 90° counterclockwise to a position at the right of the superior mesenteric artery, while the colon rotates 90° to a location to the left of the superior mesenteric artery. The midgut then herniates into the umbilical cord to continue its growth. During this time, the duodenum rotates counterclockwise another 90°, while the colon undergoes no rotation. At ten weeks, the embryonic bowel returns to the abdominal cavity, and both the duodenum and the colon rotate again. At this time, the duodenum completes its final 90° counterclockwise rotation, until the duodeno-jejunal junction is located to the left of the spine, while the colon rotates counterclockwise 180° until the cecum is located in the right lower quadrant of the abdomen. The completed normal rotation of the bowel produces a long mesenteric attachment for the small bowel [4].
A defect in stage II of midgut rotation had resulted in the presentation described in this case report. Stage I defect results in omphalocele. Stage II defect leads to malrotation, nonrotation or reversed rotation. Stage III defect results in the unattached duodenum, mobile cecum, unattached mesentery [5]. Malrotation tends to occur when the umbilical ring is wider, and the normal sequence of the return of the pre-arterial and post-arterial segment is lost [6]. The following anatomical variations may be associated with malrotation namely, Absence of kidney and ureter, Biliary atresia, Congenital diaphragmatic hernia, Duodenal or small bowel stenosis or atresia, Duodenal web, Gastroschisis, Hirschsprung disease, Imperforate anus, Meckel diverticulum, Omphalocele [7]. Some of the syndromes associated with malrotation include Apple-peel intestinal atresia, Cornelia de Lange syndrome, Cantrell syndrome, Cat-eye syndrome, Chromosomal abnormalities (trisomies 13, 18, and 21) [8]. The presented case did not have evidence of these abnormalities.
Other rare types of rotation include a. Reverse rotation of the duodenojejunal limb resulting in a duodenum that rests anterior to the superior mesenteric artery. b. Reverse rotation of the cecocolic limb resulting in a transverse colon that is posterior to the superior mesenteric artery. c. Reverse rotation of the duodenojejunal limb with the normal rotation of the cecocolic limb resulting in a para duodenal hernia. In reverse rotation, the duodenum is located anterior to the superior mesenteric artery. Anterior to the duodenum, the cecocolic limb rotates normally, and the mesentery of the right colon creates a pouch into which the small bowel can herniate [9].
Although the clinical history of the cadaver was not available, her age at death and absence of a large scar on the anterior abdominal wall signify that she may not have had any major surgical complication. The classic clinical manifestation of malrotation in newborns is bilious vomiting with or without abdominal distention associated with either duodenal obstructive bands or midgut volvulus. A delay in diagnosis and treatment may result in small bowel necrosis, short gut syndrome, and dependence on total parenteral nutrition [1]. The clinical presentation associated with nonrotation of gut ranges from vague intermittent pain to symptoms of acute bowel obstruction, although it may be asymptomatic too. The abnormally located appendix may lead to misdiagnosis of appendicitis. The peritoneal bands may lead to intestinal compression or volvulus. Nonrotation is not as dangerous for the patient as malrotation because, in general, the base of the mesentery is wider than in malrotation, and the risk of volvulus is less compared to that in malrotation. However, nonrotation can be a difficult diagnosis radiologically; symptomatic patients may warrant laparoscopic or open exploration to confirm the diagnosis. Asymptomatic patients with radiologic findings suggesting nonrotation can be observed [9].
Conclusion
The altered anatomical location of the abdominal organs in nonrotation of intestine may not always result in clinical presentation. However, misunderstanding of incidental clinical or diagnostic findings may compromise the health of the patient. Adequate knowledge of Embryology and such resultant variations aid in understanding the abnormal findings during diagnostic interventions and also prevent surgical complications.
Acknowledgement
The authors would like to thank the donor sincerely for donating her body to aid Medical education and scientific research.
References
- Applegate KE, Anderson JM, Klatte E. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006;26:1485-1500.
- Dott NM. Anomalies of intestinal rotation: their embryology and surgical aspects-with report of five cases. Br J Surg. 1923;11:251-86.
- Mall FP. Development of the human intestine and its position in the adult. J Morphol 1898;14:197-208.
- Snyder WH, Chaffin L. Embryology and Pathology of the intestinal tract: presentation of 40 cases of malrotation. Ann Surg. 1954;140:368-79.
- Monty ML, Gohl MC. Midgut Nonrotation in Adults. Am J Surg. 1975;129:319-23.
- Marx R. Nonrotation of Intestine. Ann Surg. 1939;109:49-56.
- Jamieson D, Stringer D. Small bowel. In: Babyn PS (ed.) Pediatric gastrointestinal imaging and intervention (2nd edn.), Hamilton, Ontario: Decker. 2000;311-32.
- Taybi H, Lachman R. Radiology of syndromes, metabolic disorders, and skeletal dysplasias (3rd edn.). Chicago, Ill: Yearbook Medical Publishers, 1990;825-6.
- Stockmann PT. Malrotation. In: Oldham KT (ed.) Colombani PM, Foglia RP, Skinner MA (eds.) Principles and Practice of Pediatric Surgery (2nd edn.), Philadelphia, Lippincott Williams & Wilkins. 2005;2:1283.
Velavan SS* Castellanos B, Gulfam N and Rich S
Touro College of Osteopathic Medicine, New York, NY-10027, USA
- *Corresponding Author:
- Dr. Sumathilatha Sakthi Velavan
Touro College of Osteopathic Medicine
230 W 125th Street, New York
NY-10027, USA
Tel: +646 981-4629
E-mail: sumathilathads@yahoo.co.in
Citation: Velavan SS, Castellanos B, Gulfam N, Rich S. Nonrotation of the intestine: embryological and clinical correlation. Int J Anat Var. 2017;10(3):53-4.
Copyright: This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A defect in the rotation of midgut to assemble the parts of the gut in the normal anatomical location results in nonrotation. This is a very rare variation with an incidence of 1:500. This case is reported for its extreme rarity and its resultant clinical implications. During routine dissection, the entire small intestine was found to lie on the right side of the abdominal cavity. The duodenum was located to the right of superior mesenteric artery. The ileocecal junction was traced to the hypogastrium. The colon formed a loop on the left half, and sigmoid colon was typically located. A fibrous Ladd’s band extended from posterior abdominal wall to the colon, crossing anterior to the duodenum. The clinical presentation of nonrotation ranges from vague intermittent pain to acute bowel obstruction. Adequate knowledge of Embryology and resultant variations aid in understanding the abnormal findings during diagnostic interventions and prevents surgical complications.
-Keywords
Malrotation; Nonrotation; Embryology; Midgut; Ladd’s band
Introduction
The Embryology of the gastrointestinal tract is complex and involves a particularly well-orchestrated rotation of midgut. The complex steps result in assembly of the parts of the gut in the normal anatomical location. Error at the stage of midgut rotation may result in an array of variations in the abdominal organs. The extreme form of malrotation of the midgut is non-rotation and is a very rarely reported variation with the incidence of less than 1:500 [1]. The completely altered architecture of the organs in the peritoneal cavity poses a surgical risk and deserves embryological reasoning. The aim of this study is to report an extremely rare anatomical variant. The altered arrangement of viscera is combined peritoneal relations also and hence may lead to complications such as intestinal obstruction, volvulus, and misdiagnosis. For the benefit associated with its clinical implications. This report might aid in the understanding of this anatomical variant and optimize patient management.
Case Report
During routine dissection of the abdomen in a 93-Year old, Caucasian female cadaver, abnormal location of the small intestine was noted. The cadaver was donated and embalmed with formalin based on appropriate ethical principles. A detailed analysis of the intestines was done by tracing from pyloric end of the stomach to the rectum. The vasculature of the abdominal organs was dissected. The liver, pancreas, spleen and the genitourinary tract were dissected to note any variation. The Stomach was normal in a location with the pyloric end just to the right of the midline. The duodenum was oriented vertically, coiled, lacked its usual ‘C’ loop and to the right of the vertebral column. The entire small intestine was found to lie on the right side of the abdominal cavity. The duodenum was located to the right of the superior mesenteric artery and was not crossed by the artery. The superior mesenteric vein was found on the left side of the artery. Mesenteric root was short and was in the prevertebral region. The ileocecal junction was traced to the hypogastrium where cecum and appendix were situated. The ascending, transverse and descending colon formed a‘s’ shaped loop while sigmoid colon and rectum were normally located.
The left kidney was normal while the right kidney was located closer to the midline. A fibrous Ladd’s band was found to cross the duodenum to the cecum. It extended from the posterior abdominal wall, crossed and tightly held the intestines coiled and was found attached to the greater omentum and also to the cecum (Figures 1-3).
Discussion
Early in embryonic life, before approximately 4 weeks of gestation, the gut is a short, straight, featureless tube. By 12 weeks, it has grown rapidly and, after a series of complex steps involving a total rotation of 270°, has undergone fixation in the normal position in the abdomen [2,3]. First, the duodenum rotates 90° counterclockwise to a position at the right of the superior mesenteric artery, while the colon rotates 90° to a location to the left of the superior mesenteric artery. The midgut then herniates into the umbilical cord to continue its growth. During this time, the duodenum rotates counterclockwise another 90°, while the colon undergoes no rotation. At ten weeks, the embryonic bowel returns to the abdominal cavity, and both the duodenum and the colon rotate again. At this time, the duodenum completes its final 90° counterclockwise rotation, until the duodeno-jejunal junction is located to the left of the spine, while the colon rotates counterclockwise 180° until the cecum is located in the right lower quadrant of the abdomen. The completed normal rotation of the bowel produces a long mesenteric attachment for the small bowel [4].
A defect in stage II of midgut rotation had resulted in the presentation described in this case report. Stage I defect results in omphalocele. Stage II defect leads to malrotation, nonrotation or reversed rotation. Stage III defect results in the unattached duodenum, mobile cecum, unattached mesentery [5]. Malrotation tends to occur when the umbilical ring is wider, and the normal sequence of the return of the pre-arterial and post-arterial segment is lost [6]. The following anatomical variations may be associated with malrotation namely, Absence of kidney and ureter, Biliary atresia, Congenital diaphragmatic hernia, Duodenal or small bowel stenosis or atresia, Duodenal web, Gastroschisis, Hirschsprung disease, Imperforate anus, Meckel diverticulum, Omphalocele [7]. Some of the syndromes associated with malrotation include Apple-peel intestinal atresia, Cornelia de Lange syndrome, Cantrell syndrome, Cat-eye syndrome, Chromosomal abnormalities (trisomies 13, 18, and 21) [8]. The presented case did not have evidence of these abnormalities.
Other rare types of rotation include a. Reverse rotation of the duodenojejunal limb resulting in a duodenum that rests anterior to the superior mesenteric artery. b. Reverse rotation of the cecocolic limb resulting in a transverse colon that is posterior to the superior mesenteric artery. c. Reverse rotation of the duodenojejunal limb with the normal rotation of the cecocolic limb resulting in a para duodenal hernia. In reverse rotation, the duodenum is located anterior to the superior mesenteric artery. Anterior to the duodenum, the cecocolic limb rotates normally, and the mesentery of the right colon creates a pouch into which the small bowel can herniate [9].
Although the clinical history of the cadaver was not available, her age at death and absence of a large scar on the anterior abdominal wall signify that she may not have had any major surgical complication. The classic clinical manifestation of malrotation in newborns is bilious vomiting with or without abdominal distention associated with either duodenal obstructive bands or midgut volvulus. A delay in diagnosis and treatment may result in small bowel necrosis, short gut syndrome, and dependence on total parenteral nutrition [1]. The clinical presentation associated with nonrotation of gut ranges from vague intermittent pain to symptoms of acute bowel obstruction, although it may be asymptomatic too. The abnormally located appendix may lead to misdiagnosis of appendicitis. The peritoneal bands may lead to intestinal compression or volvulus. Nonrotation is not as dangerous for the patient as malrotation because, in general, the base of the mesentery is wider than in malrotation, and the risk of volvulus is less compared to that in malrotation. However, nonrotation can be a difficult diagnosis radiologically; symptomatic patients may warrant laparoscopic or open exploration to confirm the diagnosis. Asymptomatic patients with radiologic findings suggesting nonrotation can be observed [9].
Conclusion
The altered anatomical location of the abdominal organs in nonrotation of intestine may not always result in clinical presentation. However, misunderstanding of incidental clinical or diagnostic findings may compromise the health of the patient. Adequate knowledge of Embryology and such resultant variations aid in understanding the abnormal findings during diagnostic interventions and also prevent surgical complications.
Acknowledgement
The authors would like to thank the donor sincerely for donating her body to aid Medical education and scientific research.
References
- Applegate KE, Anderson JM, Klatte E. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006;26:1485-1500.
- Dott NM. Anomalies of intestinal rotation: their embryology and surgical aspects-with report of five cases. Br J Surg. 1923;11:251-86.
- Mall FP. Development of the human intestine and its position in the adult. J Morphol 1898;14:197-208.
- Snyder WH, Chaffin L. Embryology and Pathology of the intestinal tract: presentation of 40 cases of malrotation. Ann Surg. 1954;140:368-79.
- Monty ML, Gohl MC. Midgut Nonrotation in Adults. Am J Surg. 1975;129:319-23.
- Marx R. Nonrotation of Intestine. Ann Surg. 1939;109:49-56.
- Jamieson D, Stringer D. Small bowel. In: Babyn PS (ed.) Pediatric gastrointestinal imaging and intervention (2nd edn.), Hamilton, Ontario: Decker. 2000;311-32.
- Taybi H, Lachman R. Radiology of syndromes, metabolic disorders, and skeletal dysplasias (3rd edn.). Chicago, Ill: Yearbook Medical Publishers, 1990;825-6.
- Stockmann PT. Malrotation. In: Oldham KT (ed.) Colombani PM, Foglia RP, Skinner MA (eds.) Principles and Practice of Pediatric Surgery (2nd edn.), Philadelphia, Lippincott Williams & Wilkins. 2005;2:1283.