Occurrence of ischemic stroke on the contralateral side of a hemorrhagic stroke in the subacute phase: About an observation
2 Department of Neurosurgery, University of Zimbabwe, Harare, Zimbabwe, Email: kkabulo@gmail.com
3 Department of Preventive Medecine and Public Health, Faculty of Medecine, Pharmacy and Odontostomatology, University of Cheikh Anta Diop, Dakar, Senegal
Received: 04-Nov-2017 Accepted Date: Jan 03, 2018; Published: 10-Jan-2018
Citation: Ntenga P, Kabulo K, Mourabit S, et al. Occurrence of ischemic stroke on the contralateral side of a hemorrhagic stroke in the subacute phase: About an observation. J Neurol Clin Neurosci. 2018;2(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The annual rate of stroke is eloquent and is responsible for some 60,000 deaths with 130,000 to 150,000 new cases per year, or a stroke every four minutes. This pathology is a public health priority that is underestimated in terms of morbidity and mortality as well as in terms of medico-economic costs and burden for the health system. Recidivism is a predictive factor of lethality for the victim. We report in this article the case of a 58-year-old patient who had been admitted in the Neurology department at the Fann National University Hospital and who had an ischemic stroke 14 days after hospitalization for a hemorrhagic stroke. Its evolution was unfavorable marked by the death on day 33 of his hospitalization.
Keywords
Stroke; Recurrence; Sub-acute phase; Lethality
Introduction
Stroke numbers speak for themselves and illustrate its high incidence worldwide, resulting in 15 million strokes each year. With 10% of the causes of death, of which a quarter during the first year. Stroke is the third leading cause of death in France and the second in the world. It is a disease of the elderly subject, the average age of onset is 73 years, however, 15% of strokes occur before age 50. In the United States, stroke was the 4th leading cause of death in 2013 with approximately 800,000 people being affected each year. In 2010, ischemic stroke deaths attributable to high tobacco use in Russia, China and India accounted for more cases than in the rest of the world. He is responsible for some 60,000 deaths with 130,000 to 150,000 new cases per year, or a stroke every four minutes. If 70 to 80% of people return to their homes after a stroke, one in two will still have a disability [1].
This pathology is characterized by any clinical abnormality resulting either from the sudden interruption of the blood supply to a brain territory related to an occlusion by thrombosis or embolism, or following a rupture of an arterial vessel on aneurysm for example leading to death of cells and tissues in the area of the brain that has been affected [2] and is the primary reason for hospitalization in the neurology department.
Stroke is the first cause of acquired disability in adults, the second cause of dementia (after Alzheimer’s disease, 30% of dementia are wholly or partly due to stroke) and the third leading cause of death in France. This pathology is a public health priority that is underestimated in terms of morbidity and mortality as well as in terms of medico-economic costs and burden for the health system, and remains unknown among the public health professionals. His biomedical research is very insufficient in view of the stakes [3].
Hemorrhagic strokes account for 10 to 15% of all strokes, or 10 to 20 cases per 100,000 populations [4].
In 75% of hemorrhagic strokes or 15% of total stroke it is an intra-cerebral hemorrhage, and in 25% of cases aneurysm rupture [1].
Occurrence in the sub-acute phase of a stroke in different hemispheres and of different types is rarely mentioned in the literature. This poses a management problem because this recurrence is a predictive factor of lethality in 24.8% of cases [5]. We report in this article the case of a 58-year-old patient who had been admitted in the neurology department at the Fann National University Hospital and who had had an ischemic stroke 14 days after hospitalization for a hemorrhagic stroke. Its evolution was unfavorable marked by the death on day 33 of his hospitalization.
Observation
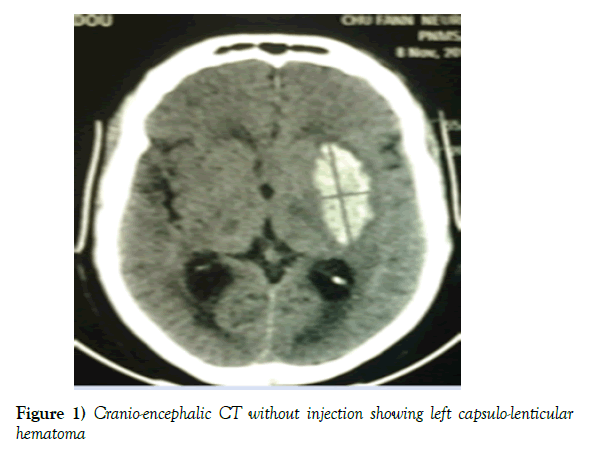
Mr NM, 58 years old, married, without a profession, Senegalese, living in Dakar and right-hander of laterality who had been admitted in the neurology department of the National University Hospital Center of Fann on November 8th, 2015 for a motor deficit of the right hemi body and a language suspension of brutal installation in a context of headache, nausea, vomiting without alteration of consciousness. The clinical examination showed a capsular-like pyramidal syndrome, an intracranial hypertension syndrome, a systolic-diastolic hypertension (220/130 mg). In front of this table, a cerebral CT without injection of the contrast product had been realized and which had revealed a left capsulo-lenticular spontaneous hematoma (Figure 1), thus the diagnosis of a hemorrhagic stroke on ground of arterial hypertension had been retained. For this, the patient had benefited from symptomatic treatment made of an antihypertensive drug (amlodipine 10 mg/day), an analgesic (paracetamol), a functional rehabilitation and nursing measures.
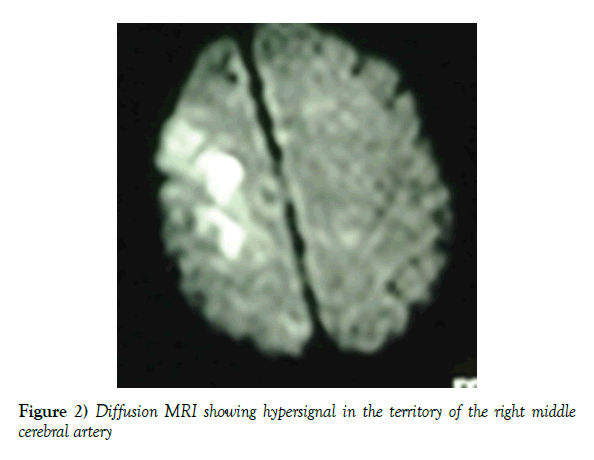
During the course of his evolution, on the 14th day of his hospitalization, the patient had abruptly presented left hemiparesis with a brachio-facial predominance, which required the realization of another brain scan (less than 3 hours after the beginning of the symptomatology) which had not shown any recent lesion, then an encephalic MRI (diffusion) carried out objectified a hypersignal in the superficial territory of the right cerebral artery (ACM) (Figure 2), this time, a ischemic stroke had been retained. The first etiological assessment of the second ischemic stroke has not been able to confirm with certainty an etiology.
Figure 2) Diffusion MRI showing hypersignal in the territory of the right middle cerebral artery
On day 29 of hospitalization, coma with a Glasgow score of 3/15 occurred, whence it was transferred to the neuro-resuscitation unit where the patient died on day 33 of hospitalization.
Discussion
The incidence of hemorrhagic stroke increases with age, especially beyond age 55, but there are also genetic factors and our patient is in the age range. It has been described by some authors that in Black or Japanese subjects, its incidence was approximately doubled compared to the rest of the population [6]. Genetic factors have clearly been identified. O ‘Donnell et al. showed that the presence of the ε2 and ε4 alleles on the genes encoding apolipoprotein E was associated with a three times greater risk of hemorrhagic recurrence after hemorrhagic stroke [7].
The prognosis of our patient was bad, we think that it was related to the large volume of the hematoma as well as the recurrence. In the work of Hemphill 3rd JC et al. [8], three factors most frequently associated with a poor neurological prognosis including hematoma volume, presence of ventricular hemorrhage and impaired consciousness have been described, and that the inconsistent prognostic value of the volume of the hemorrhage taken in isolation was not surprising and stemmed from the pressure-volume relationship inside the cranial box. Our patient was a young adult, and this corroborates this same study, which states that, in the elderly, cortical atrophy would tolerate relatively large hemorrhages, unlike a young subject who may not tolerate a much smaller hemorrhage. In a study conducted by Fogelholm et al. [9], one-year and five-year survival are approximately 42 and 27%, respectively. No studies on survival after hemorrhagic stroke in our environment have been found. A study on a long series would allow us to know the reality in our circles.
But also James et al., In his studies had shown that in Europe, stroke was the third leading cause of death and that in male subjects, was responsible for 10% of deaths, behind ischemic heart disease and cardiovascular disease (32%) and then cancers (21%). In female subjects, this rate was higher: stroke was responsible for 15% of deaths, still behind ischemic heart disease and cardiovascular disease (37%) and cancers (18%) [1]. These same authors had shown in their study that the frequency of recurrence of stroke was of the order of 5 to 15% and that in a population “stroke”, it was generally considered that over one year, about 1/5 Strokes were recurrences and these recurrences had a mortality rate that was twice that of a first stroke. We believe that the interval between recurrences is a mortality factor, hence the interest of doing a study in our circles over a long series to determine the relationship between the two parameters (time-death interval).
Some other authors believe that after a first stroke, the risk of recurrence is important in the order of 10% in the first year and 20% to 30% at 5 years. These same authors had shown that the risk of recurrence was higher than that of a first stroke in the same population, after age and sex matching and that it was maximal immediately after the infarction. Moreover, these authors had shown that more than 90% of stroke recurrences were cerebral infarctions and that cerebral infarction conferred not only a risk of recurrence but also a risk of myocardial infarction (2.1%) and deaths from vascular origin (2.2%) [10].
The occurrence or recurrence in the sub-acute phase of stroke in different hemispheres and of different types is rarely mentioned in the literature. Thus Coutts SB et al had tried to report nonspecifically the recurrence of stroke in terms of time. Thus, 6.7% would occur at 48 h, 10% risk at 7 days,10% at 20% risk at 90 days [11].
Prince Eliot Sounga B et al. [12], in a study of the epidemiological, evolutionary and paraclinical aspects of hemorrhagic stroke in the elderly in Dakar, had shown that the mean age was 65 years and that the risk factor found was high blood pressure in 91.5%, cases. The location of the hematoma and the blood pressure figures in our patient, place it in the range of literature.
Leo T et al., In their study of 885 consecutive patients with recurrent stroke (ischemic or hemorrhagic), found that diabetes was the third risk factor after high blood pressure and that dyslipidemia was present in 24% of subjects, this was comparable to prevalence during a first event. The high blood pressure figures would place our patient in the risk factor margin to repeat a recurrence even though he was not diabetic or did not have dyslipidemia [13].
Conclusion
This observation sufficiently shows the risk of mortality during recurrent stroke regardless of the type and the challenge of the management of patients who present in the acute or sub-acute phase strokes of different types in different hemispheres.
REFERENCES
- Kadouch J. AVanCEZ avec l’AVC. SCOR in FORM. 2014.
- http://www.solidarites-sante.gouv.fr/IMG/pdf/AVC_-_rapport_final_-_vf.pdf.
- http://www.epsilon.insee.fr/jspui/bitstream/1/14704/1/seriesourcemethod30.pdf.
- Qureshi AI, Tuhrim S, Broderick JP, et al. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001;344:1450-60.
- Toure K, Diagne SN, Seck LB, et al. Facteurs predictifs de mortalite par accident vasculaire cerebral (AVC) a la Clinique Neurologique du chu de Fann, Dakar - Senegal. Afri J Neurological Sci. 2010;29(2).
- Qureshi AI, Giles WH, Croft JB. Racial differences in the incidence of intracerebral hemorrhage: effects of blood pressure and education. Neurology. 1999;52:1617-21.
- O’Donnell HC, Rosand J, Knudsen KA, et al. Apolipoprotein E genotype and the risk of recurrent lobar intracerebral hemorrhage. N Engl J Med. 2000;342:240-5.
- Hemphill JC, Bonovich DC, Besmertis L, et al. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32:891-7.
- Fogelholm R, Murros K, Rissanen A, et al. Long-term survival after primary intracerebral haemorrhage: a retrospective population-based study. J Neurol Neurosurg Psychiatry. 2005;76:1534-8.
- Haute Autorité de Santé. Prévention vasculaire après un infarctus cérébral ou un accident ischémique transitoire. Recommandations. Saint-Denis La Plaine: HAS; 2008.
- Coutts SB. Int J Stroke, Le risque de récidive d’AVC), 20 novembre 2015.
- Bandzouzi PES, Adjaratou DS, Dadah SLM, et al. Aspects épidémiocliniques, évolutifs et paracliniques de l’accident vasculaire cérébral hémorragique du sujet âgé à Dakar. 2016;172(1):72.
- Leo T, Lindgren A, Peterson J, et al. Risk factors and treatment at recurrent stroke onset: results from the Recurrent Stroke Quality and Epidemiology (RESQUE) Study. Cerebrovasc Dis. 2008;25(3):254-60.