Orbital trauma management - Nurturing past understanding with 21-st century ideas
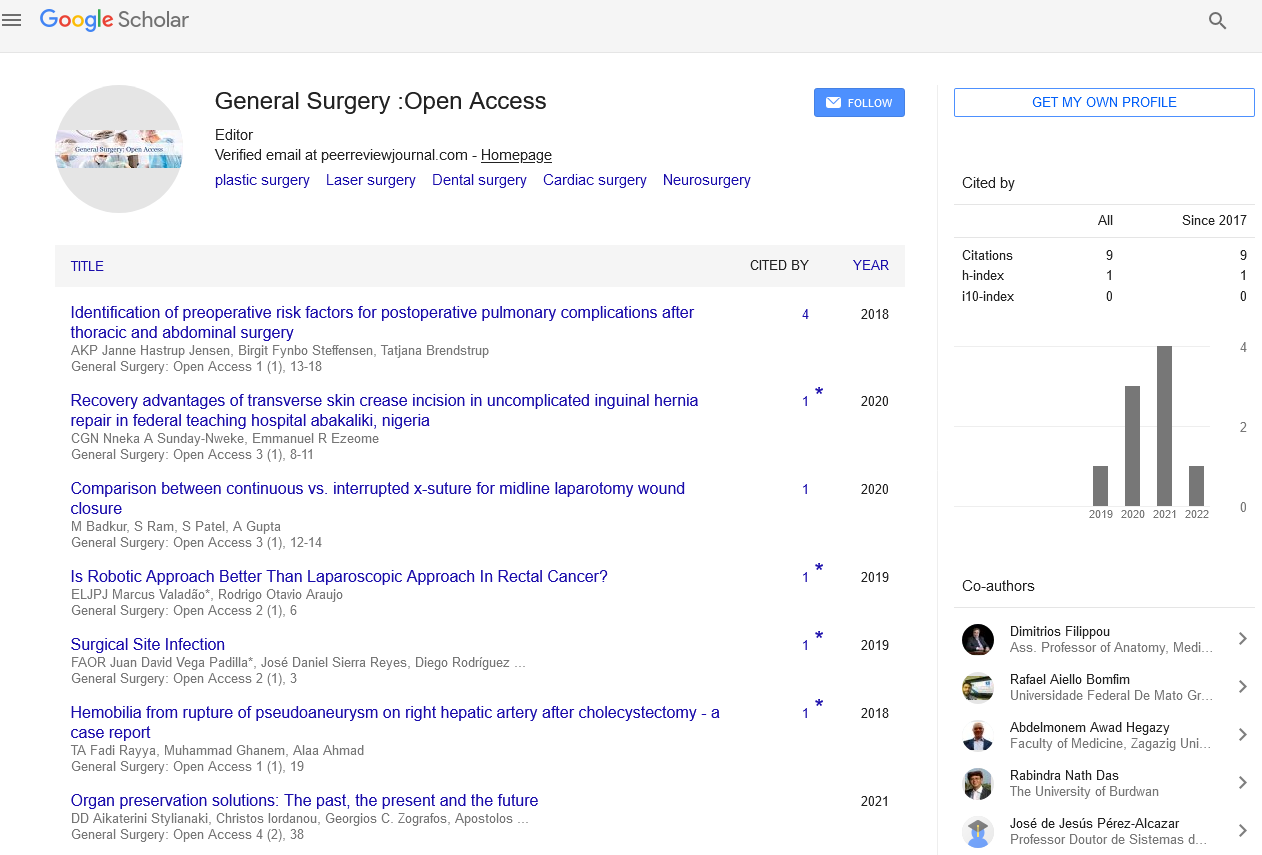
Received: 03-Dec-2021, Manuscript No. PULGSOA-22; Editor assigned: 08-Jan-2022, Pre QC No. PULGSOA-22(PQ); Accepted Date: Jan 05, 2022; Reviewed: 18-Dec-2021 QC No. PULGSOA-22(QC); Revised: 04-Jan-2022, Manuscript No. PULGSOA-22(R); Published: 14-Jan-2022, DOI: 10.37532/pulgsoa.2022.5(1)-01
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Orbital fractures account for a significant portion of traumatic facial injuries. The management of these fractures is often challenging due to the impact that they can have on vision. Acute treatment involves a thorough clinical examination and management of concomitant ocular injuries. The clinical and radiographic findings for each individual patient must then be analysed for the need for surgical intervention. Deformity and vision impairment can occur from these injuries, and while surgery is intended to prevent these problems, it can also create them. Therefore, surgical approach and implant selection should be carefully considered. Accurate anatomic reconstruction requires complete assessment of fracture margins and proper implant contouring and positioning. The implementation of new technologies for implant shaping and intraoperative assessment of reconstruction will hopefully lead to improved patient outcomes. Not all orbital fractures require operative repair. However, bony disruption can cause enophthalmos, hypothalamus, tele canthus, epiphora, cerebrospinal fluid leaks, orbital hematoma, and even blindness to name a few. Timing of operative repair as well as reconstructive method is dictated by the patient's individual presentation. Successful fracture management requires a detailed understanding of the anatomy and pathophysiology to ensure restoration of the patients' preoperative state. Orbital trauma encompasses a wide variety of mechanisms of injury and resulting fracture patterns. A variety of surgical approaches to the orbit exist as has been discussed allowing the surgeon access to all area of interest. Regardless of the fracture complexity, the principles of atraumatic technique, anatomic reduction, and stable fixation apply in all cases.
Introduction
Aconsiderable proportion of traumatic face injuries are caused by orbital fractures. Although plastic surgery material is useful, this essay provides additional pearls and insights from the expertise of an oculoplastic surgeon. The principles stay the same, but perspectives shift, providing a fresh take on a long-standing issue. The most essential thing to remember is that the ideal management plan is frequently varied, and the right decision of which strategy to adopt is dependent on the clinical circumstance and the surgeon's honest evaluation of his or her degree of knowledge and comfort level. Because of the functional and cosmetic defects that frequently emerge from orbital fractures, the treating physician must have a thorough grasp of them.
According to studies, orbital fractures account for around 10% to 25% of all occurrences of facial fractures1–3 and, like other face injuries, are most typically found in connection with assaults and motor vehicle accidents (MVAs). MVA-related orbital fractures are more destructive and are linked with more simultaneous organ injuries, zygoma fractures, and numerous orbital wall fractures than other prevalent causes of assault, such as sportsrelated, falls, and so on. Penetrating orbital injuries are less common, but they are associated with a greater than 10% chance of mortality or a future vegetative state, due mostly to neighboring cerebral injuries. Furthermore, injury to the globe, optic nerve, and extraocular muscles is always a possibility. Awareness of the important nuances of orbital injuries necessitates an understanding of the orbital examination, effective therapy, and potential consequences. As with any maxillofacial injuries, proper assessment begins with Advanced Trauma Life Support protocols. Based on clinical indicators and the manner of damage, orbital fractures should be suspected after patient stabilization.