Partial surgerical nephrectomy
Received: 03-Feb-2022, Manuscript No. pulpjsr-22-5352; Editor assigned: 06-Feb-2022, Pre QC No. pulpjsr-22-5352 (PQ); Accepted Date: Feb 25, 2022; Reviewed: 18-Feb-2022 QC No. pulpjsr-22-5352 (Q); Revised: 24-Feb-2022, Manuscript No. pulpjsr-22-5352 (R); Published: 28-Feb-2022
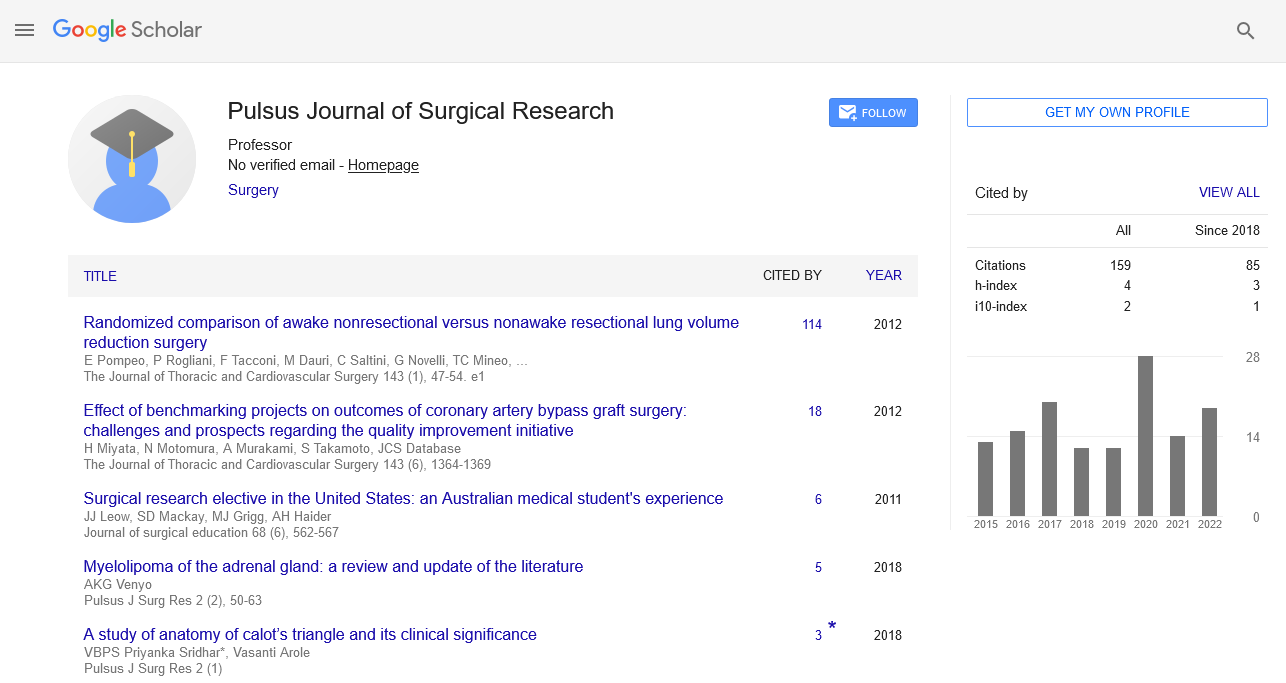
Citation: Leahy M. Partial surgerical nephrectomy. J surg Res. 2022; 6(1)):13-15.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
With the paradigm shifting from radical to partial nephrectomy, the surgical therapy of small renal tumours (4 cm) has undergone significant evolution in recent decades. When performed by skilled surgeons, Laparoscopic Partial Nephrectomy (LPN) provides comparable results to open partial nephrectomy with less patient morbidity. Analyzing LPN's present situation and potential future course was the goal of this review. Over the past 20 years, LPN has developed quickly, and technical improvements along with new surgical technologies have aided in its wider use in urologic practise. However, there are still several drawbacks, such as the inadequacy of procedures for achieving cold ischemia laparoscopically, the high technical demands of intracorporeal suturing, and the restricted capacity to analyse surgical anatomy outside of the field of view. These are research objectives that aim to reduce the invasiveness of LPN while also enhancing surgical precision and outcomes in the future.
Keywords
Thoracic surgery; Pancreatic surgery; Neurosurgery; Primordial
Introduction
With an estimated 65,150 new cases and 13,680 fatalities in the United States in 2013, kidney cancer is the third most prevalent genitourinary malignancy and the third greatest cause of genitourinary cancer-related mortality [1]. In the past, kidney cancer often manifested as a large, symptomatic, invasive, or metastatic renal tumour. The appearance and management of kidney cancer, particularly Small Renal Masses (SRM), which are defined as tumours smaller than 4 cm in size, have undergone a noteworthy change during the past three decades. Nguyen et al. observed a 52% increase in the overall rate of kidney malignancies identified in the United States from 1983 to 2002, from 7.1 instances to 10.8 instances per 100,000 people, with the highest prevalence occurring in the kidneys. Clinical stage T1a was present in 70% of newly diagnosed kidney malignancies. This has largely been due to the widespread use of contemporary cross-sectional imaging techniques including Magnetic Resonance Imaging (MRI), Computed Tomography (CT), and ultra sound. Preservation of renal function has become a crucial factor in renal oncologic surgery as a result of recent research showing a clear correlation between decreased kidney function and increased risk of cardiovascular disease and mortality. As a result, Partial Nephrectomy (PN) has expanded its list of approved uses to the point where it is now the norm for treating all SRM. In the 1960s, Poutasse enhanced the procedure by dividing the segmental blood supply to the level of the kidney, which marked the beginning of advancements toward the contemporary PN. Kerr and Klotz developed renal hypothermia, which reduced renal ischemia damage and enabled lengthier surgeries and intricate kidney reconstructions in a largely bloodless environment. The possibility of laparoscopic nephrectomy for the removal of a kidney containing a tumour was demonstrated in 1991, marking a significant turning point in the laparoscopic surgical revolution that had started in the 1970s. This was the first documented solid organ excision performed entirely laparoscopically. This opened the door for the development of the first Laparoscopic PN (LPN) procedure. Early LPN faced major difficulties in reproducing the positive oncologic results of its open counterpart, in addition to its demanding technical requirements. Various advancements in surgical technique and technology, including the introduction of the robotic surgical platform for LPN as first described by Gettman et al in 2004, have helped to lessen these difficulties over time. In this review, we seek to update the reader on recent developments in the field of minimally invasive treatment of small renal masses, as well as the findings of significant research on functional and oncologic outcomes [1].
Similar to OPN, LPN may be utilised in SRM patients with nephronsparing surgery being necessary, such as those with a single kidney, renal insufficiency, or bilateral renal tumours. This will depend on the surgeon's level of comfort. The majority of elective T1 tumours as well as more complicated tumours like T1b, central, hilar, numerous, and/or cystic tumours are now included in these indications, which have grown over time. In these situations, the selection of the patient and the preparation for renal surgery are similar to those for open surgery. A thorough physical examination and relevant medical history are required to find any potential problems that might occur during surgery. Laparoscopic surgery is no longer viewed as being contraindicated in cases of prior abdominal, retroperitoneal, or renal surgery. However, the type and amount of previous abdominal surgery will determine the placement of trocars and the surgical technique (transperitoneal versus extraperitoneal). In the hands of skilled surgeons, patient characteristics like obesity have been shown to have little effect on perioperative results. However, one study found that although generally modest, the frequency of Clavien grade III sequelae was higher for obese patients than for nonobese patients. The RENAL nephrometry score has been used to help create a repeatable, uniform classification system that quantitates the key renal mass architecture. The five crucial and repeatable anatomical characteristics of solid renal masses form the basis of the nephrometry score. Radius (R; tumour size as maximum diameter), exophytic/endophytic characteristics of the tumour (E), the proximity of the tumour to the sinus or collecting system (N), anterior/posterior descriptor, and location with respect to the polar line are all included (L). Tumors that are close to the main renal artery or vein are given the suffix "h" (hilar). The fifth component indicates the mass's anterior or posterior placement in relation to the other four components, which are scored on a 1-point, 2-point, or 3-point scale. This has evolved into a helpful tool for classifying patients according to the various renal extirpation techniques. According to Canter et al's analysis of the association between a tumor's NS and the treatment given, the more complicated the tumour, the more probable it was that the patient would have a Radical Nephrectomy (RN). Rates of RN were 6%, 23%, and 66% for tumours with low, moderate, and high scores, respectively. According to other research, the RENAL NS is a thorough and repeatable technique that could help surgeons properly communicate tumour features. Because of the high interobserver correlation, it is a high-fidelity assessment method. In a retrospective analysis, several researchers have demonstrated that RENAL NS predicted surgeon preference for choosing RN over PN [2].
The preoperative features and dimensions used for anatomic (PADUA) classification and Centrality (c)-index scores are two more standardised scoring systems. One study found that each of the three grading methods had a substantial link with some perioperative outcomes, such as the duration of warm ischemia, and strong interobserver reliability (WIT). Transperitoneal, retroperitoneal, handassisted, robotic, Laparoendoscopic Single-Site Surgery (LESS), and natural orifice transluminal endoscopic surgery are now the available laparoscopic surgical techniques to the kidney during PN (NOTES). A pneumoperitoneum is produced with each approach to expand the intra-abdominal working area. The most recent advancements in laparoscopic renal surgery, LESS and NOTES, aim to significantly reduce surgical morbidity, in part by reducing the size and quantity of abdominal trocars. Through a single abdominal incision, many laparoscopic instruments are utilised in LESS, with the occasional auxiliary instrument being used to aid triangulation. In NOTES, abdominal incisions are completely avoided using endoscopic intervention through natural orifices. LESS and NOTES currently have extremely limited clinical relevance, with NOTES being essentially experimental, pending future technology advancements and evaluation in preclinical and clinical settings [3-6]. The transperitoneal approach was the first procedure for LPN7 to be described, and it is also the method that is still most frequently employed. Since its creation, it has undergone substantial evolution and technological advancement. During the first experience, maintaining hemostasis, reducing WIT, and successfully repairing the collecting system were the key challenges. The earliest transperitoneal LPN experience was treatments for benign disease, and renal ischemia was not attained. With the help of the argon beam coagulator, hemostasis was established. Later, a variety of energy-based technologies and tourniquet devices were used, such as monopolar shears, ultrasonic shears, microwave tissue coagulators, electrosurgical snares, laser devices, and radiofrequency-assisted resection, to seal blood vessels and the renal collecting system simultaneously. Gill et al. in 2002 described the repetition of OPN procedures during LPN [7]. Laparoscopic Satinsky clamps and laparoscopic bulldog clamps were used to achieve en bloc hilar control during transperitoneal and retroperitoneal LPN, respectively. Sharp tumour excision was performed either alone or in conjunction with electrocautery [8,9]. Although challenges still exist, surgical robotics has substantially improved the surgeon's capacity to do more precise and advanced minimally invasive surgery. Currently, real-time intraoperative decision-making is facilitated by tactile feedback when available, surgeon experience, and recall of the preoperative imaging of the surgical anatomy. One of the main objectives of image-guided surgery research is to be able to visualise objects that are not directly in the field of vision, such as underlying arteries and/or resection margins, as this would further improve surgical precision. A 3D reconstruction of the surgical anatomy is placed on the live surgical view in an imageguided technology known as augmented reality. From preoperative CT or ultrasound imaging investigations, the reconstructed image is produced. In order to identify the deep tumour margin, this method was initially used in LPN in 2006. It has since been utilised to visualise the course of the renal arterial tree in order to provide zeroischemia PN using image input from 3D CT angiography. Recent research described an augmented reality system that can superimpose a CT scan's 3D reconstructed image over a da Vinci robot's 3D stereoscopic view. More research is being done to adapt this method for real-time intraoperative applications. Another area of advancement involves further minimising the invasiveness of laparoscopy. A tiny robot that can be deployed entirely in vivo and has payloads for physiologic sensing, a camera, and biopsy tools has been created and tested in animal models. These robots are autonomously controlled from a location outside the body. If they were developed further, they might make it possible to execute difficult laparoscopic procedures using just one abdominal incision. Other specialised robotics platforms for LESS and NOTES are also being developed, and these may make it easier to use these methods in clinical settings in the future. Since the procedure was first described in 1993, LPN has experienced tremendous development and is now used more frequently to treat SRM. In the published series, functional and oncological outcomes are comparable to those for OPN with tolerably low morbidity rates. Future developments in robotic and image-guided surgery are projected to increase surgical accuracy and success while further reducing the invasiveness of the procedure.
References
- Winfield HN, Donovan JF, Godet AS, et al. Laparoscopic partial nephrectomy: initial case report for benign disease. J Endourol. 1993;7(6):521–526.
- Gettman MT, Blute ML, Chow GK, et al. Robotic-assisted laparoscopic partial nephrectomy: technique and initial clinical experience with DaVinci robotic system. Urology. 2004;64(5):914-8.
- Aboumarzouk OM, Stein RJ, Haber GP, et al. Laparoscopic partial nephrectomy in obese patients: a systematic review and meta-analysis. BJU Int. 2012;110(9):1244–1250.
- Smith IJ. The Joint Commission guide to improving staff communication. Joint Commission on; 2005.
- Denise MK, John PF, David JG, et al. Improving the patient experience through provider communication skills building. Patient Exp. J.: 2014;1.
- Reason J. Human error: models and management. Bmj. 2000 Mar 18;320(7237):768-70.
- Parasuraman A, Zeithaml VA, Berry LL, et al. SERVQUAL: a multiple item scale for measuring, consumer perceptions of service quality. Journal of Retailing1988;64:12-40.
- Wofford MM, Wofford JL, Bothra J. Patient complaints about physician behaviors: a qualitative study. Acad Med 2004;79:134-138.
- Chang ACS, Read J. The Effects of Listening Support on the Listening Performance of EFL Learners. TESOL Quarterly 2006;40:375-397.