Pericardial lipoma: Diagnosed unexpectedly during heart failure investigation- Case Report
2 Department of Internal Medicine, Hypertension Clinic, State Medical School of São Jose do Rio Preto (FAMERP), Sao Paulo, Brazil
3 Department of Medicine, Centro Universitario de Votuporanga, Unifev, Sao Paulo, Brazil, Email: cestario@cardiol.br
Received: 12-Aug-2017 Accepted Date: Oct 11, 2017; Published: 13-Oct-2017, DOI: 10.4172/2368-0512.1000094
Citation: Da Silva MEFE, De Campos AMF, Vieira Baldo RC, et al. Pericardial lipoma: Diagnosed unexpectedly during heart failure investigation– Case Report. Curr Res Cardiol 2017;4(4):55-57.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
OBJECTIVE: To report the case of a patient with pericardial lipoma diagnosed unexpectedly during heart failure investigation with diagnosis definitive after surgery.
METHODS: A review of medical records and analysis of photographic records of the diagnostic exams, to which the patient was submitted, were performed and a literature review was carried out.
FINAL CONSIDERATIONS: Cardiac lipomas are very rare neoplasms in the population. Often patients with these tumors are asymptomatic or with nonspecific symptomatology. Echocardiographic diagnosis is sometimes quite difficult. Surgical treatment is reserved for cases that bring discomfort or risk to the patient. In the current case, the surgical procedure had therapeutic and diagnostic importance. This case demonstrates the importance of associating diagnostic methods in the search for an accurate diagnosis. This patient was medicated and had side effects of the therapy, because she had the diagnosis initially given only by the chest X-ray.
Keywords
Pericardial; Lipoma; Heart failure; Surgery
Heart neoplasms have a low incidence and so they are considered rare in medicine [1]. They are classified as malignant or benign neoplasms, which can be either primary or secondary (metastatic) [2].
In the literature, there are divergent estimates that show an incidence ranging from 0.001% to 0.28% [1], with from 0.02% to 0.05% being found in autopsy studies [2]. Most of these tumors (75%) are benign with myxoma accounting for 50% of the cases [2]. The other benign tumors include lipomas, rhabdomyomas and papillary fibroelastomas [2]. Metastatic tumors, epidemiologically, have an incidence of 1% [2], with this rate reaching up to 5% in autopsy studies with most originating from lung and breast carcinomas, leukemias, lymphomas and melanomas [3]. The main areas affected by metastases are the pericardium and right chambers [3].
Lipomas account for 8.4% to 10% of the cases of primary heart neoplasms and approximately 14% of benign cardiac masses [1,4].
Lipoma is a tumor comprised of adipocytes, which can be located anywhere in the body, including the heart. Although very common, especially in subcutaneous tissue, the location of lipomas in the heart is relatively rare and often just incidentally found during an autopsy [1,5].
Objective
To report the case of a patient with pericardial lipoma diagnosed unexpectedly during heart failure investigation where the diagnosis was defined after surgery, and to report on the reason why this pathology is difficult to diagnose.
Method
A review of medical records and analysis of photographic records of the diagnostic exams, to which the patient was submitted, were performed and a literature review was carried out.
Case Report
A 65-year-old female patient was referred for preoperative assessment for noncardiac surgery. She was asymptomatic from a cardiovascular point of view, however, she reported that in the weeks leading up to her consultation she had been losing her appetite, feeling weak with a postprandial sensation of fullness after ingesting little food and mastalgia.
As a personal background, she reported positive serology for Chagas disease and hypertension. She had been taking enalapril, nifedipine and hydrochlorothiazide for hypertension over a long time.
She also reported that since the diagnosis of Chagas disease, she had taken amiodarone, but she did not remember having cardiac arrhythmia. She had recently started being prescribed spironolactone and digoxin due to a change found in her chest X-ray.
She denied alcoholism and referred to lower limb varicose veins with episodes of evening edema. She denied any history of surgeries or stroke but she was being followed-up by a nephrologist due to a kidney problem.
Since the patient would perform non-cardiac surgery, we chose to better evaluate the presence of heart failure in this patient before we released for surgery.
Physical examination
She was in a good general condition, eupneic and eutrophic.
Pulmonary auscultation: Vesicular murmur present bilaterally without adventitious noises.
Heart auscultation: Regular rhythm with normal, rhythmic, hyphonic heart sounds. Presence of systolic murmur in lower left sternal border with irradiation to a mitral focus.
Abdomen: Flaccid to palpation, without visceromegaly.
Extremities: Absent of edema but she had varicose veins bilaterally. Perfusion was maintained.
Vital sounds: Blood pressure: 140/80 mmHg; Heart rate: 65 bpm;
Respiratory rate: 20 ipm
Diagnostic hypothesis
Chagasic Heart Failure
Complementary examinations
To evaluate the presence of heart failure in this patient, the following tests were requested:
1) The electrocardiogram showed a sinus rhythm with right bundle branch block and axis deviation to the left (Figure 1).
Thoracic X-ray showed an overall increase in the cardiac area (Figure 2).
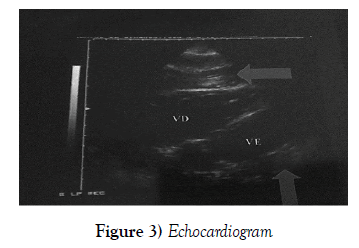
The echocardiogram showed preserved left ventricular function, the heart chambers had normal internal dimensions with the presence of anomalous echoes filling the pericardial space, whose image suggested the presence of ‘blood’ and/or a dense serous fluid in the process of organization (Figure 3).
Management
No definitive diagnosis was reached after the patient had been evaluated by three teams of experienced echocardiographers. As contrast was contraindicated, computed tomography (CT) could not be performed and magnetic resonance imaging (MRI) was not available and thus it was decided to perform an exploratory surgery.
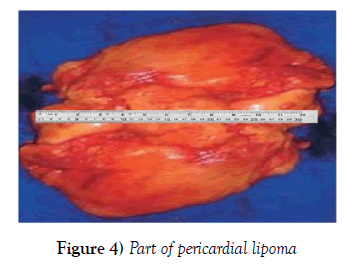
During surgery, a large pericardial tumor was resected; total resection was not possible due to the involvement of coronary arteries (Figure 4).
The intraoperative and the immediate postoperative periods were without complications. The patient was discharged without any medication to treat heart failure, just antihypertensive drugs. The histopathological report found a specimen of multiple irregular structures weighing 468 grams and measuring 20 cm × 12 cm × 9 cm. Macroscopically, the outer surface was bosselated and bright yellow-gold; its consistency was soft and brown spots were seen.
Evolution and follow-up
The patient had monthly follow-ups for one year without any complications. Control echocardiograms showed preserved left ventricular ejection fraction, mitral and tricuspid regurgitation and posterior image of residual lipoma in the pericardium. After withdrawal of digoxin and spironolactone the patient’s appetite improved, and the mastalgia and weakness disappeared.
Blood pressure at the last visit: 130 mmHg × 81 mmHg.
Discussion
Benign tumors composed of fat in the heart can be classified in two ways: lipomas or lipomatous hypertrophy of the atrial septum - an unencapsulated mass of mature and fetal adipocytes [5]. Primary tumors are further classified according to their cardiac location as pericardial, endocardic or epicardial [6].
Comparatively, lipomas in the heart behave and appear similar to lipomas in other regions of the body and consist of a mass of encapsulated adipose tissue composed of mature cells; they may also be composed of muscle tissue, when they are called myolipomas, or fibro-fatty tissue, fibrolipomas [7,8]. Generally, they are single and delimited, with wide or spherical shapes and can grow to large sizes [1]. The most commonly involved sites are the epicardial region of the cardiac muscle, the atrium or the ventricle [1] with the wall of the left chambers being the most commonly affected region [5-9].
The cause is unknown, although it is accepted that they can be congenital or associated with obesity [1]. Most of the published reports state that the frequency is similar for both sexes, and without predilection by age group. However, Durak and Eren report a prevalence in males and in the age group between 40 and 60 years old [8].
Typically, lipomas are asymptomatic however, when symptoms are present they vary depending on the location and mass size [1-8]. The main clinical findings are associated with mechanical compression [7-9] and include cough, angina, malaise, palpitations and arrhythmias, atrioventricular block, precordialgia, fatigue, dyspnea, syncope and even sudden death (7,9,10). Tumors extending into the cavity can produce symptoms consistent with right heart failure [4]. Subendocardial tumors are, in most cases, an accidental finding [6]. An arrhythmia may be caused by an intramyocardial tumor due to its interference in the electrical conduction system of the heart [6-8].
Karigyo and Silva [3] divide the symptomatology of heart tumors as: Obstructive - chest pain, dyspnea, precordialgia, mimicking valve stenosis; Embolization - in the tumor itself or in adjacent structures mimicking vasculitis, endocarditis or evolution of stroke; and Arrhythmias – caused by myocardial infiltration or by the mass itself [3].
Several imaging methods allow an analysis of the relationship between mass and adjacent structures [10]. On the chest X-ray, lipomas are seen as a mass with intermediate density that is indicative of fat content [1]. CT and MRI are the methods with good diagnostic accuracy [5]. The diagnosis and characterization of the tumor can be made through echocardiography, CT or MRI [4].
Fat tissue is easily differentiated in CT as a hypodense tissue with characteristic attenuation of 20 to 50 HU [3-9], while MRI reveals a hypersignal in T1 and attenuated images in T2, with total interruption of the signal using fat saturation images [3].
Pleuropericardial cysts are part of the differential diagnosis and are distinguished by their net content. Other conditions included in the differential diagnosis are descending aortic aneurysm, dilation of the right atrium and Morgagni hernia [1].
Treatment is reserved for symptomatic patients in order to avoid complications, although they are uncommon. Most are amenable to surgical resection, although this procedure is rarely required for lipomas. The surgical approach can involve different methods including thoracotomy, clamshell incision or sternotomy depending on the characteristics of the tumor seen on imaging studies, in particular by MRI [9,10]. Complete resection of the neoplasm is recommended because of the risk of recurrence [11].
Jayle et al. list three reasons to justify the surgical exploration of a tumor of adipose tissue located in the thoracic cavity: diagnostic confirmation by a histopathological study, resolution of the clinical symptoms of the patient and the possibility of progressive compression of adjacent organs [12].
In 1968, Donald described the existence of only 30 case reports of cardiac lipomas in an article [7]. In 2002, according to García-Ramos et al., there were few more than 70 reported cases [4]. Durak and Eren argue that because of the insidious growth of lipomas, their incidence described in the literature is much lower than the actual number of cases (8). Felix Girrbach, Friedrich- Wilhelm Mohr and Martin Misfeld agree with this statement [11].
Conclusion
Cardiac lipomas are neoplasms of very low incidence in the population. In the literature, there are few reports on the diagnosis of lipomas located in the pericardium. Often patients with these tumors are asymptomatic or with nonspecific symptomatology. Such characteristics increase the difficulties for the clinical suspicion of lipomas, as occurred in the patient reported herein. CT, which was contraindicated in this case due to the need of contrast, and MRI (equipment not available at our hospital), although they are great aids in the investigation, could not be performed, making diagnosis more difficult for the doctors involved in this case. As has been mentioned, surgical treatment is reserved for cases that cause discomfort or risk to the patient.
In this case, the surgical procedure had not only therapeutic impact, providing relief from the symptoms, but also diagnostic importance. This case demonstrates the importance of associating diagnostic methods in the search for an accurate diagnosis. This patient was medicated and had side effects of the therapy, because she had the diagnosis initially given only by the chest X-ray.
Acknowledgement
The authors acknowledge the subject, his parent, other healthcare practitioners who participated in his care.
Disclosures
None.
Ethical Disclosures
Informed and written consent were obtained from the parent of this reported case. The necessary institutional protocols on the publication of the data were duly followed.
Funding
This case report did not receive financial support
Conflict of Interest
No conflict of interest among the authors.
REFERENCES
- Valido RP, Estévez AL. Lipoma Pericárdico: presentación de un caso. Rev Ciencias Medicas 2013;17(6):196-201.
- Karigyo CJT, Silva FBF. Tumores cardíacos: uma breve revisao de literatura. Rev Med Res 2014;16(1):27-34.
- García-Ramos G, Oseguera J, Najera RG. Lipoma cardiaco: Reporte de un caso. Medica Sur Sociedad del Medicos 2002;9(2):88-90.
- Puvaneswary M, Edwards JR, Bastian BC, et al. Pericardial lipoma: Ultrasound, computed tomography and magnetic resonance imaging findings. Australas Radiol 2000;44(3):321-4.
- Acceta P, Acceta I, Acceta, et al. Lipomas Gigantes. Revista do Colégio Brasileiro de Cirurgioes 1998;25(5):359-61.
- Valencia A, Lombo M, Correa J. Lipoma intrapericárdico gigante silente. Rev Colomb Cir 2011;26(3):222-5.
- Heath D. Pathology of Cardiac Tumor. 1968;21.
- Durak D, Eren B. Pericardial lipoma: An autopsy case and review of the Literature. J Forensic Sci 2007;52(4):949-50.
- Mourad OMA, Andrade FM, Abrahao P, et al. Massa mediastinal gigante assintomática: um raro caso de timolipoma. J Bras Pneumol 2009;35(10):1049-52.
- Valencia A, Lombo M, Correa J. Lipoma intrapericárdico gigante silente. Rev Colomb Cir 2011;26:222-5.
- Girrbach F, Mohr FW, Misfeld M. Epicardial lipoma-A rare differential diagnosis in cardiovascular medicine. Euro J Cardio-Thoracic Surg 2012;41:699-701.
- Jayle C, Hajj-Chahine J, Allain G, et al. Pleural lipoma: A non-surgical lesion? Interact Cardiovasc Thorac Surg 2012;14(6):735-8.