Peripheral nerve injuries- an analysis of 75 cases
2 Plastic and Reconstructive Surgery, Sher-I-Kashmir Institute of Medical Sciences, Soura, Srinagar, India, Email: uvish@yahoo.com
3 Darul Aloom University, Riyadh, KSA, Email: uvish@yahoo.com
4 Neurosurgery, Sher-I-Kashmir Institute of Medical Sciences, Soura, Srinagar, India, Email: uvish@yahoo.com
Received: 25-Mar-2018 Accepted Date: Mar 26, 2018; Published: 18-Apr-2018
Citation: Ovais H, Adil H, Mukhtar B, et al.. Peripheral nerve injuries- an analysis of 75 cases. Pulsus J Surg Res. 2018;2(1):34-39.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objectives: The study focuses on demographic patterns of various patterns of peripheral nerve injury patients in a tertiary hospital.
Methods: Seventy five patients of peripheral nerve trauma were studied over 2 years (June 2006 to September 2008). Most of the patients were subjected to early proper exploration of the wounds and direct nerve repair. Nerve conduction studies were performed in late cases. Standard microsurgical nerve repair was performed in majority. Recovery patterns were noted at regular intervals on follow up examinations.
Results: Most of the patients were young students with an average age of 26.4 years. Glass was the main agent inflicting the injury (58.7%) and wrist injuries were common in our group (62.8%). Median nerve and Ulnar nerves were the most frequently injured nerves in our patients. Epineural microsurgical nerve repair technique was applied to most of our patients. On follow up examinations, excellent recovery patterns were noted in clean lacerated nerves which were repaired early.
Conclusion: Peripheral nerve injuries are quite common and challenging to a plastic surgeon. They are mostly overlooked upon in trivial traumatic injuries and subsequently lead to loss of various functional modalities. Proper early exploration in glass cut injuries along the volar aspect of the wrist and use of standard microsurgical nerve repair procedures, yields excellent results in this group of patient population.
Keywords
Glass; epineural repair; highest scale
Introduction
Peripheral nerve trauma has been quite common in the civilian practice and the surgeons have had to manage severe extremity trauma with underlying neural damage. These injuries are on an increase presently due to modernization and undeclared warfare. Despite advances in surgical technique, peripheral nerve function after injury is dependent on many factors that elude the surgeon. The process of wallerian degeneration and peripheral nerve regeneration is complex, inter-related and influenced by multifactorial determinants. The age of patient, the level of injury and perhaps even the flexibility of the patient’s psyche seem to be the major determinants of how well the nerve regenerates in the clinical setting.
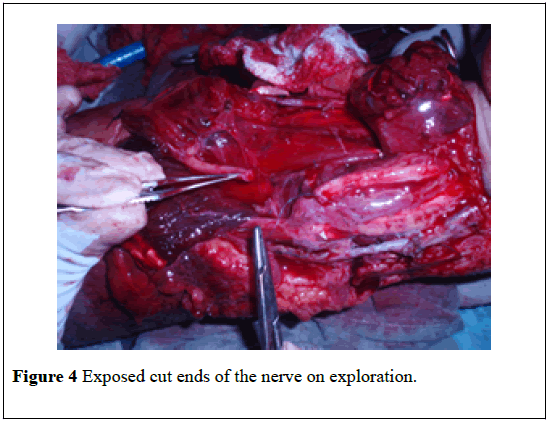
Glass has been the major culprit in inflicting serious neural damage and a small looking skin wound often disguises the extensive nature of the injuries beneath. A thorough exploration of the wound under general anesthesia is a prerequisite to identify the underlying nerve injury. The more recent innovations in repair are the use of delicate technique, the process of operative magnification, the use of smaller sutures and avoidance of excessive tension across the repaired site [1-13].
Methods
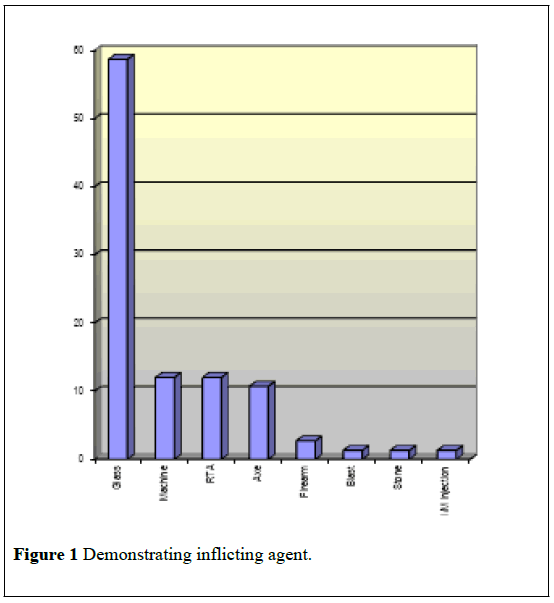
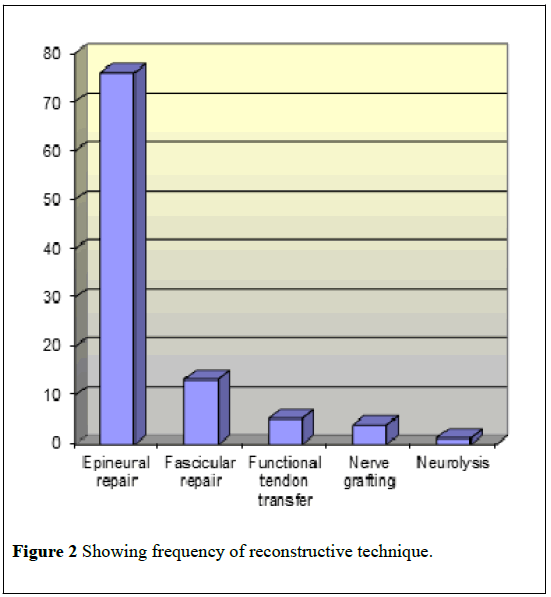
Seventy five patients with peripheral nerve trauma, were admitted to the Plastic and Reconstructive unit of Sher-i-Kashmir Institute of Medical Sciences, and were studied between June 2006 and September 2008 (Figures 1 and 2).
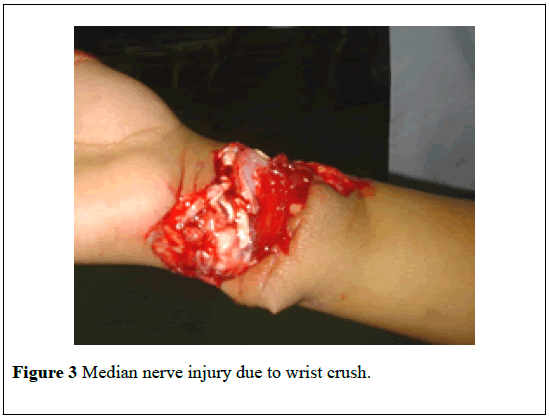
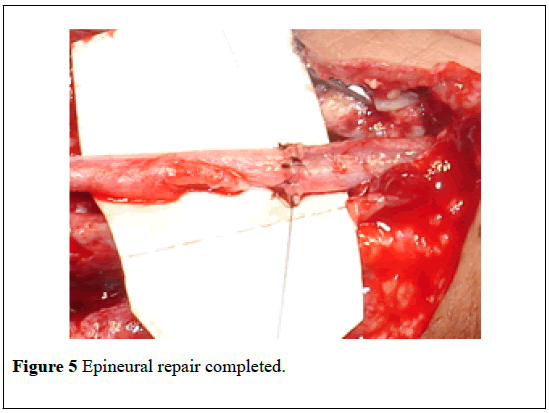
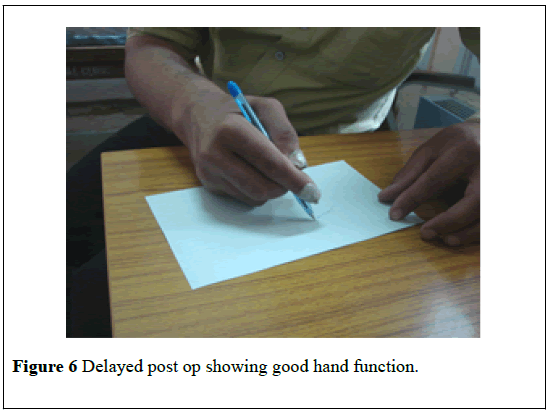
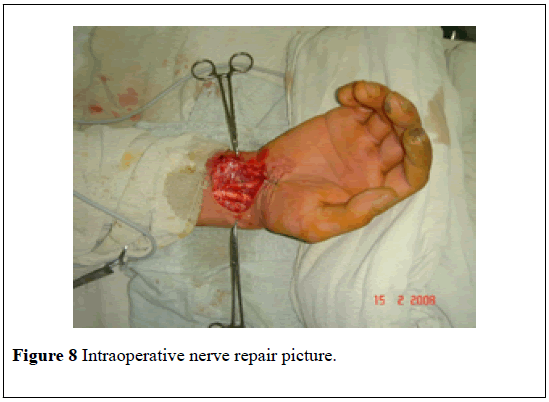
The average age of the patients was 26.4 (range 7-65 years). Sixty four patients (85.3%) were men and eleven were women (14.7%).Thirty three patients were students (44%), who suffered a sharp wrist cut. Glass was the main agent inflicting the injury (58.7%) and wrist injuries were common in our group (62.8%). Most of the patients reported on the day when the injury took place (Figures 3 and 4). Majority of the patients had absent all sensory modalities (98.7%) and motor deficit due to loss of adductor function of the thumb and wrist drop was noted in 53.3% of the patients. The patients were explored under general anesthesia and cut ends of the nerve were identified. For some of the patients who reported late, in addition to the clinical examination, Nerve conduction velocity and Electromyography also aided in the preoperative diagnosis of the injured nerve. Median nerve (33%) and Ulnar nerve (32%) were the most frequently injured nerves in our patients. Epineural microsurgical repair was carried out in majority of our patients under loop magnification with nylon 8-0 sutures. Three patients had a significant gap between the divided ends of the nerve and these were repaired using sural nerve cable grafts. Postoperatively the patients were assessed for the restoration of sensory modalities and the degree of motor recovery on subsequent follow-ups (Figures 5 and 6).
Results
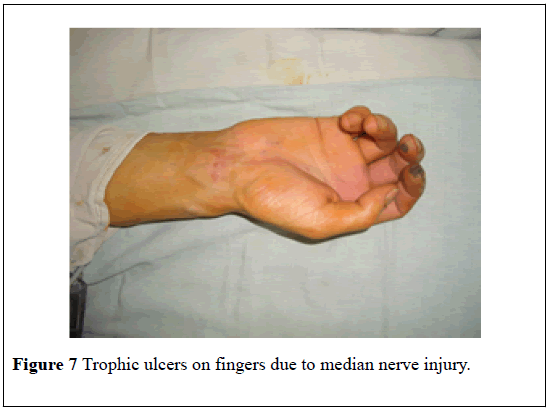
The results were evaluated as per the highest scale adopted by British Medical Council grading system for sensory and motor recovery (Table 1) (Figures 7 and 8).
| Motor grade | Level of recovery |
| M0 | No recovery |
| M1 | Perceptible contraction in proximal muscles |
| M2 | Perceptible contraction in proximal and distal muscles |
| M3 | Contraction possible against gravity |
| M4 | Contraction possible against resistance |
| M5 | Full recovery in all muscles |
| Sensory grade | Level of recovery |
| S1 | No recovery |
| S1 | Recovery of deep cutaneous sensibility |
| S1+ | Recovery of superficial pain and sensibility |
| S2 | Recovery of superficial pain and some touch |
| S2+ | S2 recovery with hypersensitivity |
| S3 | Recovery of pain and touch without hypersensitivity |
| S3+ | S3+ recovery with localization and some two-point discrimination |
| S4 | Complete recovery with normal two-point discrimination |
Table 1: The British Medical Research Council’s rating system for motor and sensory recovery.
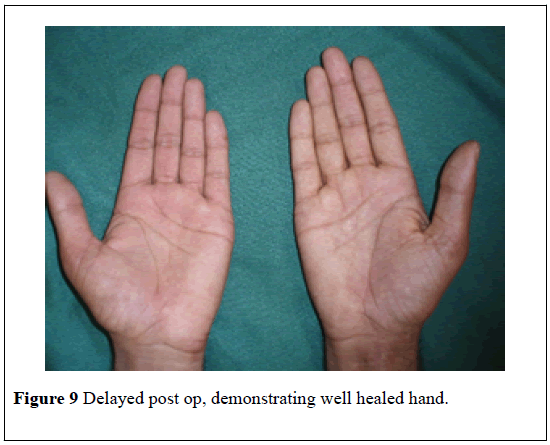
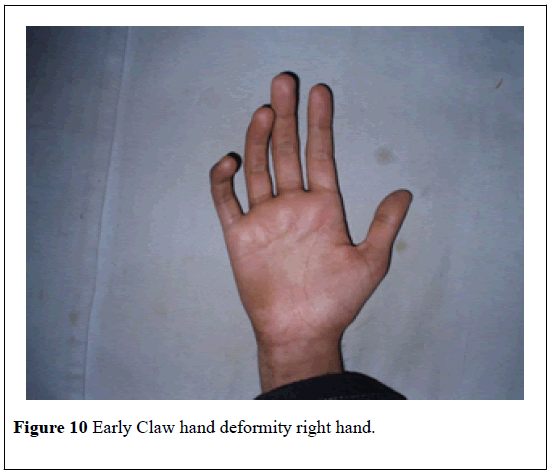
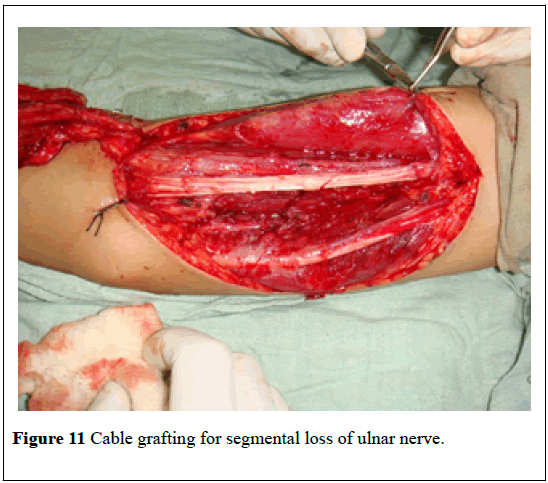
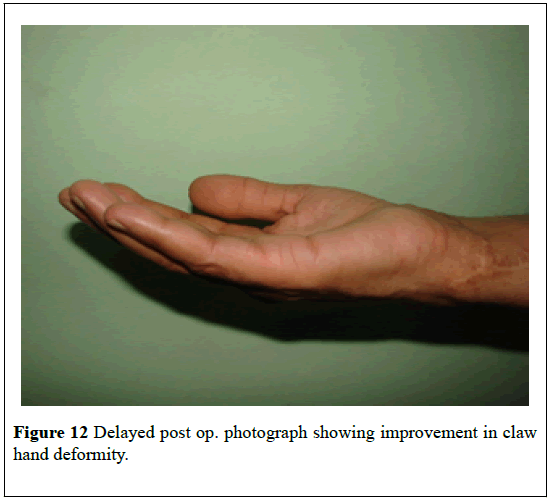
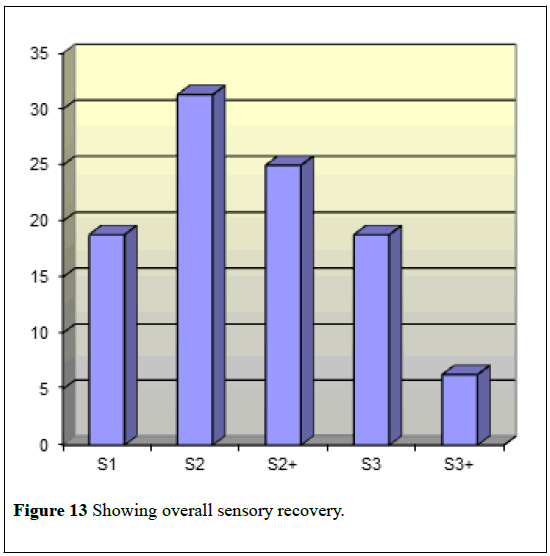
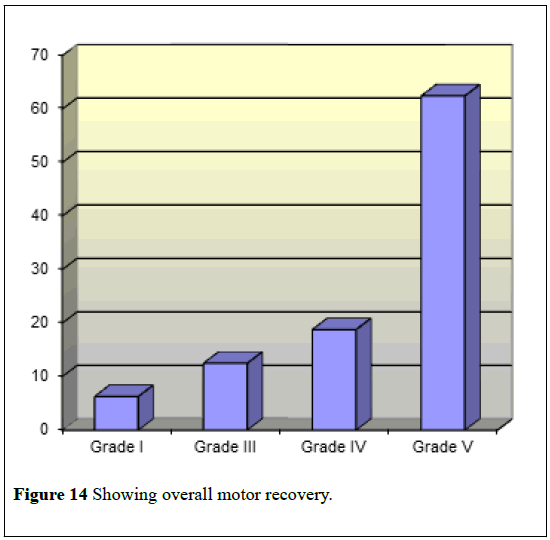
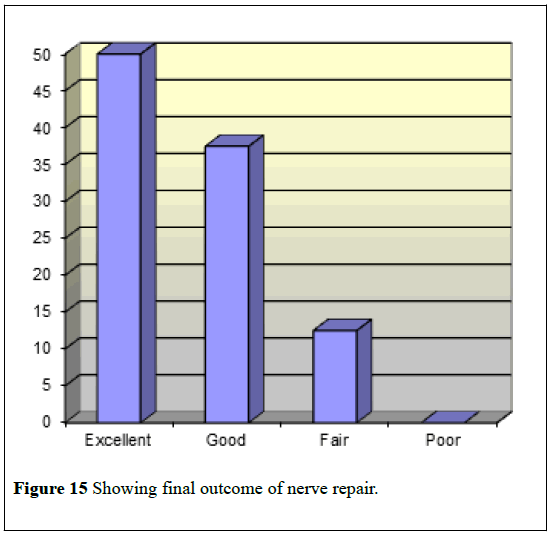
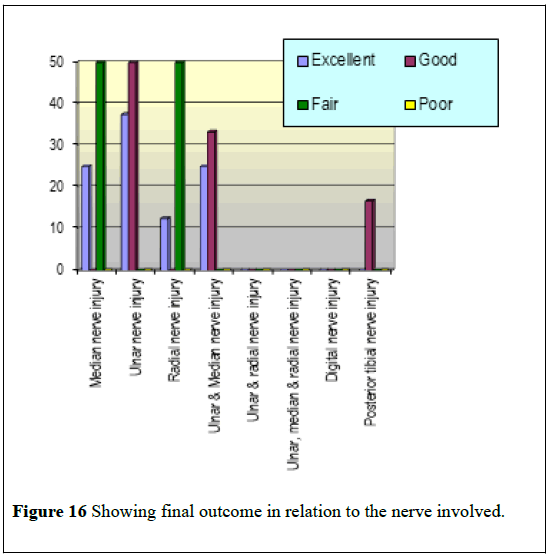
In our patients , at 27 months of follow up, we achieved, S3+ sensory recovery in 6.3% of the patients, S3 in 18.8% ; S2+ in 25%, S2 in 31.3% and S1 in 18.8% of the patients. Selma et al. observed at mean follow up of 5 years ; S4 sensory recovery in 35.7% of their patients , S3+ in 28.5%, S3 in 4.2%, S2+ in 7.14%, S2 in 10.7% and S1 in 3.5% of their patients. Daoutis et al. observed at mean follow up of 26 months, results for median nerve repair were: S4 recovery in 8.5%, S3+ in 42.5%, S3 in 36.5%, S3 in 39%, S2 in 12% of their patients. In terms of motor recovery, M5 motor restoration was noted in 62.5% of the patients, M4 in 18.8%, M3 in 12.5% and M1 in 6.3% of the patients. Daoutis et al. reported M4 recovery in 51% of their patients of median nerve injury, M3 in 17% and M2 in 31.9% at 26 months of follow up. For ulnar nerve injuries, their motor recovery was M4 in 70.7%, M3 in 14.6% and M2 in 14.6% (Figures 9-12). When we compared the results with the world literature we found that we had excellent results in 50% of the patients, good in 37.5% and fair in 12.5% of our patients [10-15].
Figure 11: Cable grafting for segmental loss of ulnar nerve.
Discussion
Microsurgical nerve repair has got revolutionized in the recent past following considerations given to the level and extent of injury, technical skill and strategy employed by the surgeon and the physiologic or pathologic milieu of the patient and the injury. Suspected open nerve injuries, in which an open wound is accompanied by an anatomically appropriate neurologic deficit, mandate timely but not emergent exploration. However, if the nerve is intact on exploration, management proceeds according to the protocol for closed injuries. Proximal v/s distal injuries also play a role in predicting the outcome. In our series of patients, the experience in terms of outcome was comparable with the worldwide literature taking all the above criteria into consideration (Figures 13 and 14).
Glass cut, the main offending agent in our patients, inflicts substantial damage to the underlying nerves beneath the skin wound (Figures 15 and 16).
Furthermore, our group of patients were mostly students, therefore, and were probably not experienced in handling the causative agent properly. The skin wounds harbour severe underlying nerve injuries and early exploration of the wound aids in identifying the damage. This too has been supported by the literature whereby the patients have been explored under general anesthesia to look for underlying nerve damage [8-10].
Epineural microsurgical repair offers good results in an emergency setting where the time factor has to born in mind. Use of magnifying loop, micro instruments and micro sutures have a definite role in the outcome (Table 2). Whenever the defect is >5cm or when excessive traction is required to approximate the divided ends of the nerve, grafting becomes necessary. In our patients we used sural nerve in the form of cable grafts to bridge the gaps as also has been reported [8,10,11].
| Results at 6 month FU | Results at 1 year FU | Results at 2 years FU | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Excellent | Good | Fair | Poor | Total | Excellent | Good | Fair | Total | Excellent | Good | Fair | Poor | Total | ||
| Median nerve injury | n | 0 | 0 | 14 | 11 | 25 | 0 | 15 | 10 | 25 | 2 | 0 | 1 | 0 | 3 |
| % | 0 | 0 | 34 | 64.7 | 34.2 | 0 | 28 | 55.6 | 34.2 | 25 | 0 | 50 | 0 | 19 | |
| Ulnar nerve injury | n | 0 | 11 | 12 | 0 | 23 | 1 | 22 | 0 | 23 | 3 | 3 | 0 | 0 | 6 |
| % | 0 | 73 | 29 | 0 | 31.5 | 100 | 41 | 0 | 31.5 | 38 | 50 | 0 | 0 | 38 | |
| Radial nerve injury | n | 0 | 2 | 5 | 0 | 7 | 0 | 6 | 1 | 7 | 1 | 0 | 1 | 0 | 2 |
| % | 0 | 13 | 12 | 0 | 9.6 | 0 | 11 | 5.6 | 9.6 | 13 | 0 | 50 | 0 | 13 | |
| Ulnar and median nerve injury | n | 0 | 0 | 6 | 5 | 11 | 0 | 56 | 5 | 11 | 2 | 2 | 0 | 0 | 4 |
| % | 0 | 0 | 15 | 29.4 | 15 | 0 | 11 | 27.7 | 15 | 25 | 33 | 0 | 0 | 25 | |
| Ulnar and radial nerve injury | n | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| % | 0 | 0 | 2 | 0 | 1.4 | 0 | 1.9 | 0 | 1.4 | 0 | 0 | 0 | 0 | 0 | |
| Ulnar, median and radial nerve injury | n | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| % | 0 | 0 | 0 | 11.7 | 2.7 | 0 | 0 | 11.1 | 1.4 | 0 | 0 | 0 | 0 | 0 | |
| Digital nerve injury | n | 0 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| % | 0 | 0 | 5 | 0 | 2.7 | 0 | 3.7 | 0 | 2.7 | 0 | 0 | 0 | 0 | 0 | |
| Posterior tibial nerve injury | n | 0 | 2 | 0 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 1 | 0 | 0 | 1 |
| % | 0 | 13 | 0 | 0 | 2.7 | 0 | 3.7 | 0 | 2.7 | 0 | 17 | 0 | 0 | 6 | |
| Total | n | 0 | 15 | 41 | 17 | 73 | 1 | 54 | 18 | 73 | 8 | 6 | 2 | 0 | 16 |
| % | 0 | 21 | 56 | 23.3 | 100 | 1.4 | 74 | 24.7 | 100 | 50 | 38 | 13 | 0 | ## | |
| p value | 0.00 (sig) | 0.005 (sig) | 0.928 (NS) | ||||||||||||
Table 2: Final outcome of peripheral nerve injury patients.
We used the Highest scale for the assessment of the recovery. We were able to achieve upto S3+ and S3 sensory recovery and upto M5 and M4 motor recovery in those patients who completed 27 months of the followup. Selma et al report upto S4 and S3+ recovery in their patients, but their follow-up was for a longer time than ours. Further, our patients are still recovering and better results are expected as they are being continuously followed up [15-20].
Conclusion
We thus concluded that for small looking glass cut wounds, the injury must not be underestimated from the description of the wound only and thorough exploration should be done to identify the underlying peripheral nerve injury. Timely address should be made to repair the damaged nerve making full use of the surgical skill, instrumentation and magnification. Further the epineural nerve repair for these clean cut nerve lacerations gives excellent results.
REFERENCES
- Bunnell S. Surgery for the nerves of the hand. Surg Gynecol Obstet 1927;44:145.
- Babcock WW. Standard technique for operations on peripheral nerves with special reference to closure of large gaps. Surg Gynecol Obstet 1927;45:364.
- Seddon HJ. Autogenous grafts for the repair of large gaps in the peripheral nerves. British Journal of Surgery 1947;35:151-167.
- Holmes W. Histological observations on the repair of nerves by autografts. British Journal of Surgery 1947;35:167-173.
- Strange FG. An operation for nerve pedicle grafting. British Journal of Surgery 1947;34:423-425.
- Hafiz M, Lee S, Wolf P, Parviz H. A comparative study of autologous peripheral nerve grafts. Microsurgery 1985; 6:135-140.
- Zhong SZ, Wang GY, He YS, et al. The relationship between structural features of peripheral nerves and suture methods for merve repair. Microsurgery 1988;9:181-185.
- Nunlay JA, Ugino MR, Goldner RD, et al. Use of anterior branch of the medial antebrachial cutaneous nerve as a graft for the repair of defects of the digital nerve. The Journal of Bone and Joint Surgery 1989;71:563-567.
- Mailander P, Berger A, Schaller E, et al. Results of primary nerve repair in the upper extremity. Microsurgery 1989;10:146-150.
- Iconoumon TG, Zuker RM, Michelow BJ. Management of major penetrating glass injuries to the upper extremities in children and adolescents. Microsurgery 1993;14:91-96.
- Medinaceli LD, Prayon M, Merle M. Percentage of nerve injuries in which primary repair can be achieved by end-to-end approximation. Microsurgery 1993;14:244-246.
- Oberlin C, Beal D, Leechavengvongs S, et al. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus. The Journal of Hand Surgery (Am.) 1994;19:232-237.
- Daoutis NK, Gerostathopoulos NE, Efstathopoulos DG, et al. Microsurgical reconstruction of large nerve defects using autologous nerve grafts. Microsurgery 1994;15:502-505.
- Hattori Y, Doi K, Fuchigani Y, et al. Experimental study on donor nerves for brachial plexus injury: Comparison between the spinal accessory nerve and the intercostal nerve. Plastic and Reconstructive Surgery 1997;100:900-906.
- Selma P, Emre O, Oguz P, et al. Evaluation of the improvement of sensibility after primary median nerve repair at the wrist. Microsurgery 1998;18:192-196.
- Wang KK, Nemeth IR, Seckel BR, et al. Hyaluronic acid enhanced peripheral nerve regeneration in vivo. Microsurgery 1998;18:270-275.
- Blaauw G, Sauter Y, Lacroix CLE, et al. Hypoglossal nerve transfer in obstetric brachial plexus palsy. Journal of Plastic, Reconstructive and Aesthetic Surgery 2006;59:474-478.
- Llyoyd BM, Luginbuhl RD, Brenner MJ, et al. Use of motor nerve material in peripheral nerve repair with conduits. Microsurgery 2007;27:138-145.
- Birch R, Benney G, Payan J, et al. Peripheral nerve injuries. Journal of Bone and Joint Surgery 1986;68:1.
- Millesi H, Meissl G, Berger A. The interfascicular nerve grafting of the median and ulnar nerves. Journal of Bone and Joint Surgery (Am.) 1972;54:727.