Peripheral vascular thrombo-embolism and the role of various fogarty arterial thrombo-embolectomy catheters: A comparative prospective study and its result
Received: 25-May-2018 Accepted Date: Jun 06, 2018; Published: 15-Jun-2018
Citation: Haridas AK, Bhat BS. Peripheral vascular thrombo-embolism and the role of various fogarty arterial thrombo-embolectomy catheters: A comparative prospective study and its result. J Vas Dis Treat. 2018;2(2):03-06.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Acute embolism and thrombosis are the commonest cause of peripheral vascular occlusion. Acute ischemic rest pain is the common mode of presentation in an emergency department. Majority of vascular thromboembolism are presented in late stage. Usage of Fogarty arterial embolectomy catheter results in incomplete thromboembolectomy and the poor chance of revascularization. It leads to a greater chance of amputation and mortality. Usage of Fogarty adherent clot catheter with Fogarty arterial embolectomy catheter has an advantage. It does not only improve the rate of better revascularization but also salvage the limbs and reduces the mortality.
Materials and methods: It is randomized prospective study, includes 200 patients from December 2015 to January 2018. 100 patients each in group A and group B. Fogarty arterial embolectomy catheter used alone in Group A and Fogarty arterial embolectomy catheter with Fogarty adherent clot catheter used in Group B.
Results: It is proven that usage of Fogarty adherent clot catheter along with Fogarty arterial embolectomy catheter in thromboembolectomy, results in better peripheral limb revascularization.
Conclusion: Regardless of the time of the presentation, use of Fogarty adherent clot catheter with Fogarty arterial embolectomy catheter has the better outcome.
Keywords
Embolism; Thrombosis; Fogarty catheter; Artery; Amputation
Introduction
Thrombo-embolism is the commonest cause of critical limb ischemia worldwide. They are responsible for the major disabilities and death due to septic gangrene. Acute vascular embolism and thrombosis have different underlying pathophysiology, treatment and outcome. The result of treatment depends on the time of presentation and conditions of the organs affected [1].
Majority of the source of embolism is due to the atrial fibrillation caused by ischemic heart disease and rheumatic heart disease [2,3]. The in-situ thrombosis caused by ulcerated atherosclerotic plaque, hypercoagulable state, vascular stenosis, dehydration, trauma and previous vascular bypass surgery [4].
The lower limb vessels frequently affected compared to upper limbs. Thromboembolism of brain, mesenteric and renal arteries are rare and life-threatening. Cardiac source of emboli inflicts multiple organs with variable severity.
Manifestation depends on the limbs, bowel, renal and cerebral ischemia. Ultimate outcome correlates with organ involved, time of presentation and collaterals. The symptomatic thrombo-embolism needs aggressive assessment and intervention compared to asymptomatic thrombosis [5].
Historically open incomplete thromboembolectomy was associated with higher incidence of amputation and deaths. The invention of Balloon Fogarty catheter and its further modification lead to a decreased incidence of amputation and deaths [6]. No single device offers complete extraction of primary and secondary embolus to achieve total revascularization. Catheters selection is based on cause, source and composition of the thrombus. The rate of revascularization dictated by the type of catheters due to the varied tensile strength of balloons and wires to extract thrombo-embolus [7].
Materials and Methods
It is a prospective study comprising 200 patients, suffering from limb ischemia due to vascular thromboembolism.
Patients with limb ischemia due to thromboembolism, who were symptomatic for 3 months or less included in the study. They have been evaluated for the causes, co-morbidities and conditions of the limb at the time of presentation. The severity of the limb ischemia assessed as per Rutherford classification [8]. Diagnosis confirmed by vascular Doppler study and C T angiogram. Patients who were asymptomatic, thrombosis over 3 months, vascular trauma, peripheral vascular disease and critically ill excluded from the study.
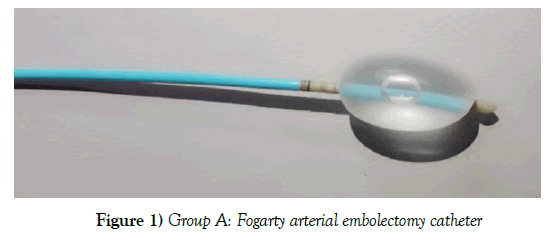
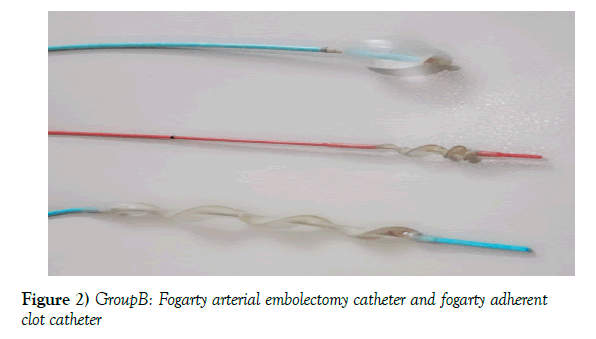
Group A (n-100) underwent thromboembolectomy with Fogarty arterial embolectomy catheter (Figure 1). Group B (n-100) underwent thromboembolectomy with the help of both Fogarty adherent clot catheter and Fogarty arterial embolectomy catheter (Figure 2).
Groups A and B evaluated to compare device efficiency based on the complete extraction of thrombus, revascularization, relief of pain, limb salvage, mortality and the complications.
Majority of the procedure was done under local anaesthesia. Injection heparin 5000 IU, bolus dose given, 3 minutes before clamping vessels. The technique of thromboembolectomy followed based on the group. Post-op patients put on injection Heparin infusion, 20 units per kg body weight per hour, till PT/INR optimised by oral anticoagulants. Activated clotting time (ACT) done twice a day, to maintain between 180 to 250. The peripheral pulse recorded by a palpatory method and Doppler probe.
Patients were assessed by vascular Doppler study of the operated limb to evaluate the extent of the revascularization.
Results
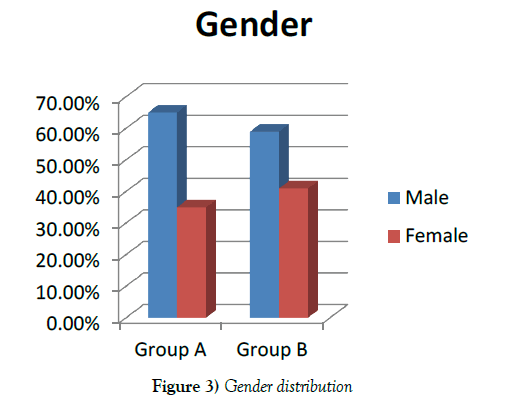
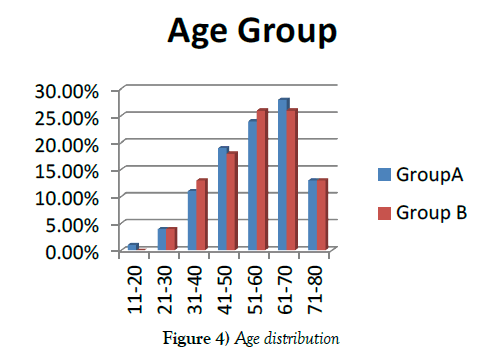
In our study, 65 in group A (65%) and 59 in group B (59%) were male patients (Figure 3). Majority of patients were between 40 to 70 years in both groups (Figure 4).
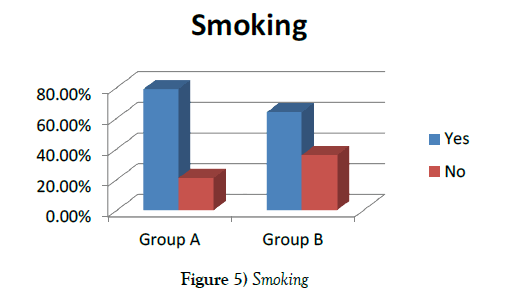
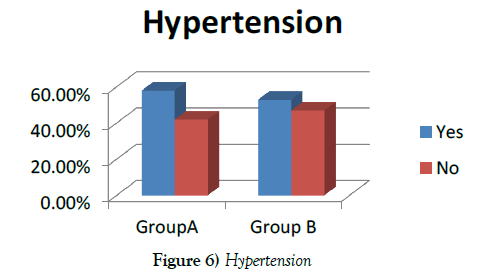
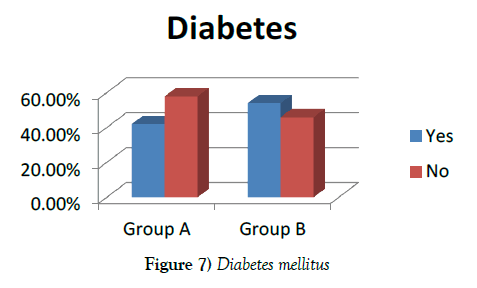
79 group A (79%) and 64 group B (64%) were smokers (Figure 5). 58 group A (58%) and 53 group B (53%) had a history of hypertension (Figure 6). Diabetes mellitus found in 42 group A (42%) and 54 group B (54%) (Figure 7).
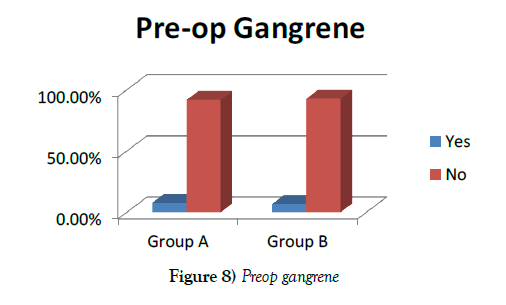
In 8 group A (8%) and 7 group B (7%) cases had pre-gangrene at the time of presentation (Figure 8).
Group A involved, 34 femoral arteries (34%), 36 popliteal arteries (36%), four infrarenal aortae (4%), 12 iliac arteries (12%), ten axillary arteries (10%), four subclavian arteries (4%). In group B, 37 femoral arteries (37%), 39 popliteal arteries (39%), three infrarenal aortae (3%), nine iliac arteries (9%), six subclavian arteries (6%), six axillary arteries (6%) were involved.
In group A 56 right limbs (56%), 36 left limbs (36%) and 8 bilateral limbs (8%). in group B, 52 right limbs (52%), 38 left limbs (38%), 10 bilateral limbs (10%) involved.
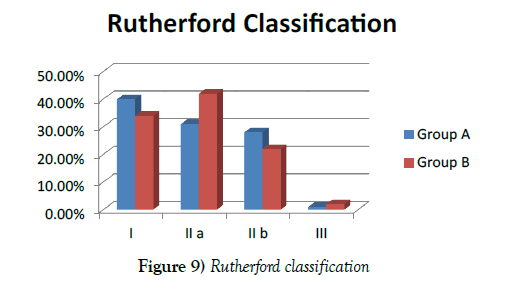
As per Rutherford classification, in group A 40 class I (40%), 31 class II a (31%), 28 class II b (28%) and one class III (1%). in group B 34 class I (34%), 42 class II a (42%), 22 Class II b (22%) and two Class III (2%) were present (Figure 9).
Minor device-related complications found. Group A had two dissections (2%), one haematoma (1%), and one embolization of ruptured bit of balloon (1%). In group B one perforation (1%), three haematoma (3%) and one vascular avulsion (1%).
Postoperatively, eight group A (8%) and two group B (2%) cases had to undergo re-embolectomy for persisting pain and thrombosis of vessels. Post thromboembolectomy, in group A, four below knee amputation (4%), four forefoot amputation (4%) and two toe disarticulations (2%) compared to group B, one below knee amputation (1%) and two toe disarticulation (2%) done, which is a significant finding (p-value 0.05). Three group A (3%) and one group B (1%) patient died due to progressive septicaemia.
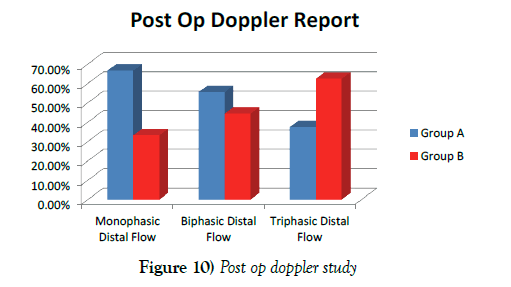
Postoperative Doppler study evidently showed, in group A 20 monophasic flow (20%), 50 biphasic flow (50%) and 30 triphasic flow (30%) compared to group B ten monophasic flow (10%), 40 biphasic flow (40%) and 50 triphasic flow (50%) found, which is significant finding (p-value 0.009) (Figure 10).
Discussion
Cardiac source of embolism and vascular in situ thrombosis are the commonest cause of ischemia leading to disability and mortality. Thromboembolism frequently found in peripheral limbs. The incidence of upper limb ischemia and gangrene less compared to lower limbs due to collaterals [9]. Extent and severity of ischemia dictate the outcome of treatment. The high rate of mortality found in acute arterial ischemia due to the release of toxins from the affected limb [10]. The goal of intervention to re-establish circulation, restoring pulses, pain relief and salvage the limb.
The incidence of chronic arterial thromboembolism unusual but not rare. Early detection and appropriate management either thromboembolectomy or bypass surgery salvage the limbs [11]. In-situ thrombosis due to prothrombotic endothelium caused by hyperhomocysteinaemia or ulcerated atherosclerotic plaque [12]. Ulcerative plaque can induce blue toe syndrome due to the shower of crystal cholesterol microembolization. It can also put life and limbs in danger in case of larger embolization. Proximal major vessel embolectomy required to save the life of patients and distal vessel embolectomy required to save limbs [13].
Options for treatment of the thromboembolism based on cause, time of presentation and severity of limb ischemia. Treatment with Intravenous anticoagulation, catheter-directed thrombolysis, thromboembolectomy by Fogarty catheters and bypass surgery used [14,15].
In selected patients, thrombolysis has a successful role [16]. Emergency dissolving thromboemoblism guarantees the limb salvage and prevents mortality [17]. Catheter-directed thrombolysis has been tried in various studies. It showed, dissolution of embolus in 70%, 80% symptoms free and 80% limbs salvaged. Infusion of thrombolytic agent for 24 hours or more showed better results. The major drawback is the significant incidence of cerebral haemorrhage and embolic stroke [18].
Pre Fogarty arterial embolectomy catheter era, Procedure of thromboembolectomy was cumbersome and time-consuming. Majority of the cases were needed multiple arteriotomies in multiple sites of vessel walls. High incidence of incomplete thromboembolectomy with progressive ischemia terminated into either amputation or death. Innovating newer techniques and devices for thromboembolectomy worked in few and most remained unsuccessful [19-21].
Dr Thomas Fogarty invented Fogarty arterial embolectomy catheter in 1963 and presented a paper in 1965, about his experience. Fogarty catheter embolectomy becomes minimally invasive, the fast technique does complete or near complete embolectomy, re-establishing the circulation. It leads to dramatic reduction in the incidence of amputation and death [22]. Recent studies have shown, simple Fogarty arterial embolectomy catheter, useful in the selective group of patients. Successful in less 50% of cases and remaining 50% of cases would require other forms of percutaneous catheter intervention or bypass surgery [23]. Simple embolectomy enables extraction of the thromboembolic load if presented at an early stage as long as vessels are not diseased [24]. The option of delayed thromboembolectomy has a definitive role in establishing vascularisation with gratifying results. This avoids surgical bypass and related complications [25].
The incidence of in-situ thrombosis has been increased in native vessels and prosthetic grafts. The technique of percutaneous aspiration of thrombus useful in selective patients [26]. Primary success of aspiration is about 60% and secondary technical success is 96% [27].
The mechanical thromboembolectomy catheters have been modified to suit to remove organised adherent thrombus and prosthetic graft thrombus. Endovascular catheters have been developed and utilized as per suitability for underlying disease and time of presentation [28].
The hydrodynamic device is made and used for fragmentation of the thrombus followed by aspiration in selective patients [29]. The hydrodynamic catheter has two lumens, can be used to shred the thrombotic material and aspirated by venture effect simultaneously [30]. Mechanical devices can also be used for complete or partial recanalisation of vessels [31]. Amplatz device is one such a promising option. It helps faster and safe recanalisation of peripheral chronic thromboembolic occlusion of arteries [32].
Surgical thromboembolectomy is a blind procedure. It is difficult to assess on the table about the completion of thromboembolectomy. To overcome this shortfall, studies have been done to improve technique and to asses completeness of thromboembolectomy [33]. It is found that fluoroscopically assisted thromboembolectomy (FATE) greatly improves the results of the treatment. It helps to negotiate the catheter, gives the idea of completion of embolectomy and decreases the catheter-related complications [34].
Nature of consistency of embolus and thrombus varied with an underlying cause and duration of occlusion [35]. Mere usage of Fogarty balloon arterial embolectomy catheter remains inadequate in a majority of the cases, who presents after 72 hours. Such embolus gradually get organises with the intima of a vessel as primary embolus with neo secondary embolus formed proximal and distal to it due to stasis of blood. It is difficult to extract organised thromboembolism with simple Fogarty arterial embolectomy catheter. This is true and evidently seen on our postoperative Doppler study. Secondary embolus remains fragile and unstable, it’s likely chances of migration into the distal smaller vessels are very high. Its clearance by antegrade and retrograde embolectomy dictates completeness of revascularization.
Fogarty arterial embolectomy balloon catheters, inflation volume and pull force has its limitations. Beyond a limit, likely chance of rupture of the balloon is high, if tried for an adherent or organized thromboembolectomy. It is advocated for simple embolectomy in acute embolism preferably lesser than 72 hours. It should not be used for fibrous or adherent thrombus [36]. Acute embolism and presentation of such cases within 72 hours, rare in the Indian scenario. Majority of symptomatic cases presented to us after week or more.
Fogarty adherent clot catheter flexible, made of polyvinyl chloride surrounding stainless steel spring body. It has a handle to modulate spiral cable diameter as per requirement. Device easy to negotiate through organised, even sometimes calcified thrombus and able to clear occlusion. It enhances results of complete revascularization [37]. This unique characteristic of adherent clot catheter helped us to extract maximum embolism and got better revascularisation results. It has reduced number of amputations and deaths.
All types of Fogarty thromboembolectomy catheters and its modified percutaneous devices are an indispensable collection in the armamentarium of thromboembolectomy. Catheters are simple, safe and easy to use. Immensely helped to salvaged millions of limbs and life. Device-related complications were minor and rare. Complications in the form of vessel dissection, perforation, haematoma, rupture and avulsion of vessels found [38]. Majority of the complications treated conservatively. In one of the cases, popliteal artery got avulsed, during usage of adherent clot catheter. Reanastomose of the vessel done uneventfully. Amount of traction and recoiling diameter of adherent clot catheter has to be controlled, based on the quality and diameter of the vessels.
Conclusion
Complete extraction of primary and secondary thrombo-embolus is the mainstay for re-establishing peripheral circulation. Using Fogarty adherent clot catheter with Fogarty arterial embolectomy catheter has the greater advantage in achieving the purpose. Fogarty adherent clot Catheter usage evidently reduced the incidence of amputations and mortality.
It’s safe and easy to use Fogarty adherent clot catheter with the minimum learning curve. No serious complications found if used with appropriate precautions.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/ or publication of this article.
REFERENCES
- Lyaker MR, Tulman DB, Dimitrova GT, et al. Arterial embolism. Int J Crit Illn Inj Sci. 2013;3(1):77-87.
- Abe Y, Asakura T, Gotou J, et al. Prediction of embolism in atrial fibrillation: Classification of left atrial thrombi by transesophageal echocardiography. Jpn Circ J. 2000;64(6):411-5.
- Menke J, Luthje L, Kastrup A, et al. Thromboembolism in atrial fibrillation. Am J Cardiol. 2012;105(4):502-10.
- Saric M, Kronzon I. Aortic atherosclerosis and embolic events. Curr Cardiol Rep. 2012;14(3):342-9.
- Mutirangura P, Ruangsetakit C, Wongwanit C, et al. Clinical differentiation between acute arterial embolism and acute arterial thrombosis of the lower extremities. J Med Assoc Thai. 2009;92(7):891-7.
- Gossage JA, Ali T, Chambers J, et al. Peripheral arterial embolism: Prevalence, outcome, and the role of echocardiography in management. Vasc Endovascular Surg. 2006;40(4):280-6.
- Krueger K, Deissler P, Coburger S, et al. How thrombus model impacts the in vitro study of interventional thrombectomy procedures. Invest Radiol. 2004;39(10):641-8.
- Hardman RL, Jazaeri O, Yi J, et al. Overview of Classification Systems in Peripheral Artery Disease. Semin Intervent Radiol. 2014;31(4):378-88.
- Champion HR, Gill W. Arterial embolus to the upper limb. British J Surg. 2005;60(7):505-8.
- Blaisdell FW, Steele M, Allen RE. Management of acute lower extremity arterial ischemia due to embolism and thrombosis. Surgery. 1978;84(6):822-34.
- Ruangsetakit C, Chinsakchai K, Wongwanit C, et al. Chronic arterial embolism of the lower extremities: an unusual etiology of critical limb ischemia. J Med Assoc Thai. 2011;94(12):1457-64.
- Galbraith K, Collin J, Morris PJ, et al. Recent experience with arterial embolism of the limbs in a vascular unit. Ann R Coll Surg Engl. 1985;67(1):30-3.
- Branchereau A, Laurian C. Emboli-forming arteriopathies of the limbs. J Mal Vasc. 1987;12(4):340-4.
- Results of a prospective randomized trial evaluating surgery versus thrombolysis for ischemia of the lower extremity. The STILE trial. Ann Surg. 1994;220(3)251-66.
- Ouriel K, Veith FJ, Sasahara AA. Thrombolysis or peripheral arterial surgery: phase I results. TOPAS Investigators. J Vasc Surg. 1996;23(1):64-73.
- Lozano P, Flores D, Blanes I, et al. Acute lower limb ischemia complicating endocarditic due to Candida parapsilosis in a drug abuser. Ann Vasc Surg. 1994;8(6):591-4.
- Buhr HJ, Mann B, Lorenz EP. Vascular surgery techniques in peripheral vascular embolism. Chirurg. 1998;69(1):38-47.
- Wongwanit C, Hahtapornsawan S, Chinsakchai K, et al. Catheter-directed thrombolysis for acute limb ischemia caused by native artery occlusion: an experience of a university hospital. J Med Assoc Thai. 2013;96(6):661-8.
- Crawford ES, Debakey ME. The retrograde flush procedure in embolectomy and thrombectomy. Surgery. 1956;40(4):737-46.
- Keeley JL, Rooney JA. Retrograde milking; an adjunct in technic of embolectomy. Ann Surg. 1951;134(6):1022-26.
- Dale WA. Endovascular suction catheters for thrombectomy and embolectomy. J Thorac Cardiovasc Surg. 1962;44:557-8.
- Fogarty TJ, Cranley JJ, Krause RJ, et al. A method for extraction of arterial emboli and thrombi. Surg Gynecol Obstet. 1963;116:241-4.
- Hill SL, Donato AT. The simple Fogarty embolectomy: an operation of the past?. Am Surg. 1994;60(12):907-11.
- Caminiti R, Arrigo G, Broccio G. Our experience with peripheral arterial embolectomy. Minerva Chir. 1975;30(8):466-76.
- Gertler JP, Distant DA, Varughese G. Delayed thromboembolectomy for subacute limb ischemia. Am J Surg. 1991;162(5):468-72.
- Oguzkurt L, Ozkan U, Gumus B, et al. Percutaneous aspiration thrombectomy in the treatment of lower extremity thromboembolic occlusions. Diagn Interv Radiol. 2010;16(1):79-83.
- Schleder S, Diekmann M, Manke C, et al. Percutaneous aspiration thrombectomy for the treatment of arterial thromboembolic occlusions following percutaneous transluminal angioplasty. Cardiovasc Intervent Radiol. 2015;38(1):60-4.
- Carlson GA, Hoballah JJ, Sharp WJ. Surgical thrombectomy: current role in thromboembolic occlusions. Tech Vasc Interv Radiol. 2003;6(1):14-21.
- Hill B, Fogarty TJ. The use of the Fogarty catheter in 1998. Cardiovasc Surg. 1999;7(3):273-8.
- Hopfner W, Vicol C, Bohndorf K, et al. Percutaneous transluminal hydrodynamic thrombectomy the initial results. Rofo. 1996;164(2):141-5.
- Rilinger N, Gorich J, Friedrich JM, et al. Thrombectomy using a high-speed rotatable catheter initial results. Rofo. 1996;164(2):153-7.
- Rilinger N, Gorich J, Pamler RS, et al. Short-term results with use of the Amplatz thrombectomy device in the treatment of acute lower limb occlusions. J Vasc Interv Radiol. 1997;8(3):343-8.
- Shin HS, Kyoung KH, Suh BJ, et al. Acute Limb Ischemia: Surgical Thromboembolectomy and the Clinical Course of Arterial Revascularization at Ankle. Int J Angiol. 2013;22(2):109-14.
- Lipsitz EC, Veith FJ. Fluoroscopically assisted thromboembolectomy: should it be routine? Semin Vasc Surg. 2001;14(2):100-6.
- Krueger K, Deissler P, Coburger S, et al. How thrombus model impacts the in vitro study of interventional thrombectomy procedures. Invest Radiol. 2004;39(10):641-8.
- Fogarty TJ, Cranley JJ, Krause RJ, et al. A method for extraction of arterial emboli and thrombi. Surg Gynecol Obstet. 1963;116:241-244.
- Novotny K, Taborsky J, Semrad M. Thrombectomy and embolectomy using the adherent clot catheter. Sb Lek. 2001;102(3):405-10.
- Schweitzer DL, Aguam AS, Wilder JR. Complications encountered during arterial embolectomy with the Fogarty balloon catheter. Vasc Surg. 1976;10(3):144-56.