Health status in India: A study of urban slum and non-slum population
Received: 22-Dec-2017 Accepted Date: Jan 08, 2018; Published: 18-Jan-2018
Citation: Usmani G, Ahmad N. Health status in India: A study of urban slum and non-slum population. J Nurs Res Pract. 2018;2(1):09-14.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
India has the second largest urban population in the world. Among the urban poor population only 40 per cent of under 3-year children were completely immunized in 2004-05, 54 per cent of under five years were stunted. Thus, this paper seeks to examine the large disparities within the urban population in health-related indicators for India and for some of its selected states. It shows the disparities for child and maternal health. The paper also shows the poor performance in some health-related indicators in slum and non-slum population- for instance under-five mortality rate. The increasing population in urban India and the poor health condition of slum and non-slum population makes the present study more relevant and useful for further research.
Keywords
Health care; Urban health; Child and maternal health; Health of slum and non-slum population; Under five-mortality
Introduction
Urbanization is emerging as the most challenging and serious concern facing our country Today. Urban population has grown from 18 per cent in 1955 to 33 per cent in 2015. Cities and towns are the centers or base of investments, technology, economic growth, and for the creation of jobs. The contribution of cities and towns in GDP of the country is immense. With the expansion and spread of urbanization the population growth in the urban areas has been growing rapidly, people have migrated from rural to urban areas in search of better jobs and life style. There are some negative consequences of urbanization such as the high population density, slums and un-notified settlements, pollution, health problems, unemployment etc.
Figure 1 shows the growth of urban population in India. In 1901 only 10.80 per cent population lived in urban areas as compared to 89.2 per cent rural population. The percentage of urban population has been growing since then year after year, in 1931 share of urban population increased to 12 per cent, this percentage further increased to 17.30 in 1951 against the rural population of 82.7 per cent. Share of urban population increased to 23.30 in 1981 against the 76.7 per cent of rural population. In 2001 urban population reaches to the level of 28.50 per cent of total population and in 2011 the urban population further increased to 31.20 per cent against the 68.8 per cent rural population. This continuous growth of urban population creates alarming problems related to health and wealth into the urban areas of the country. An estimated 25 per cent of urban population still subsists on income that is below poverty line (Report of the committee on slum statistics/census). The majority of this percentage lives in slums, in inhuman condition that deny their right to basic civic amenities or social services such as proper health care utilization, sanitation, education, adequate diet etc. As urbanization grows, the share of urban population to total population also go on increase, thus we may expect from this that the slum population share to the countries total population will tend to grow even on more faster rates [1].
According to the Encyclopedia Britannica slums is defined as “the residential area that are physically and socially deteriorated and in which satisfactory life style is impossible.” The NSSO defines slums as declared and undeclared slums. The declared slums are those which have been formally declared as slums by the respective governing bodies and the undeclared slums is defined as “an aerial part having twenty-five or more kutcha houses mostly of temporary nature, or inhabited by persons with practically no private latrine and inadequate public latrine and safe water supply. India is also the home for world’s largest urban population with below poverty line incomes, and to the world’s largest population living in slums. In 2004-05, 25.6% urban dwellers were below the poverty line and the largest concentration of urban population was in Maharashtra (14.6 million), Uttar Pradesh (11.7 million), and Madhya Pradesh (7.4 million). The latest National Sample Survey Office (NSSO) survey estimates that the number of slums in India at 33,510 with 8.8 million households in them. Census 2011 found that there are 40,309 identified slums, constituting 37 per cent of the total.
Many of health problems in slums comes from the lack of access to or demand for the basic services. Lack of safe drinking water, clean environment and garbage disposal creates serious threats to the health of slum population especially women and children as they spend most of their time in and around the area [2].
Objectives and data source of the study
• The paper seeks to examine the disparities within the urban population in health-related indicators for India and for some of its selected states.
• To study the inequalities in health-related indicators of slum and non-slum population (under five mortality).
The data is collected from the census reports, NFHS survey reports, and from some other government reports as well.
Health care in urban India
The population in urban India is about 38 crores (census 2011). The level of urbanization increased from 27.81% (2001) to 31.6% (2011) census, and the proportion of rural population to the total population declined from 72.19% to 68.84% in 2011 census. According to the census 2011 improvement in education level in rural areas is two times than in urban areas. Almost 33 per cent of India’s population lives in urban India. As per to the data from various sources the health condition of urban India is better than those of rural India, but the migration from rural to urban areas has resulted rapid growth in urban population and slums; the slum population faces greater health hazards due to over-crowding, environmental pollution as shown in Table 1 [3].
| BP % | IMR | U5MR | |
|---|---|---|---|
| URBAN | 20.9 | 31 | 41 |
| RURAL | 33.8 | 51 | 71 |
| TOTAL | 29.8 | 47 | 64 |
Table 1: Health conditions of rural and urban India, 2005-06
The existing health infrastructure in urban areas is insufficient to meet the basic needs of growing urban population. The municipalities, state government, and the central government have tried to build up urban health care infrastructure. Majority of hospitals, doctors and para-professionals are in urban areas but unlike to the rural health services there have been no efforts to provide the health care services to the areas that are geographically delineated. Thus, in many urban areas the primary health care facilities are not available; some of them are underutilized while there are overcrowding in secondary and tertiary care services. With no referral and screening system, most of the equipment’s and machinery in secondary and tertiary care centers are underutilized. The local government (municipalities) has to provide both preventive and curative services to the urban population, however the existing infrastructure with municipalities are not sufficient to cater to the growing burden of urban population.
Children’s health in urban India
The increasing number of urban residents and migrants into the urban areas creates environmental problems that are directly affects their health. The child living in household greater than 5 persons per sleeping room is 1.4 times higher than the household with less than 4 persons per sleeping room. Poor environmental condition, sanitation, and inadequate diet, results in high malnutrition in urban areas especially in slums. Children’s are the most vulnerable portion of urban population, especially urban poor children living in urban slums. Out of a billion of child population living in urban India, about 300 million faces exclusion from essential health services and other services like safe drinking water, sanitation, education etc. their existence is not recognized, as neither their births nor their deaths are registered. Children’s are the victim of many diseases, and disasters. Childhood to them is only a fantasy or nightmare. Figure 2 shows children under nutrition below 3 years of age in urban India, 1992-2000.
Source: NFHS Survey Reports, Govt. of India.
Figure 2) Child under nutrition below 3 years of age in urban India, 1992-2000
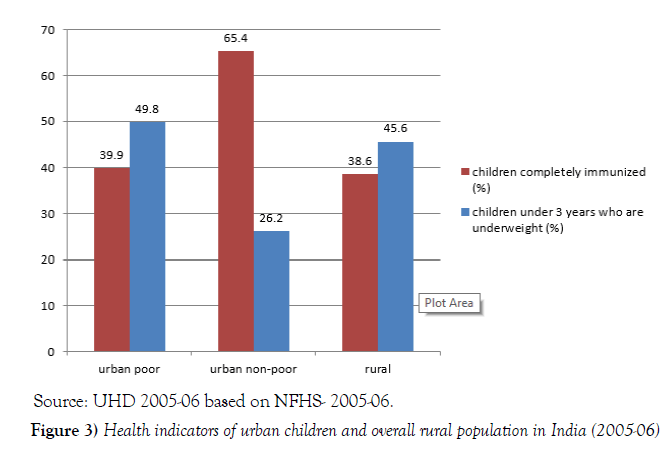
The urban-rural health disparity has long been studied, but the disparity that exists among the urban children has been neglected. Over 60 per cent urban poor children do not receive complete immunization as compared to 58% rural children; 47.1% urban poor children under 3 years of age are underweight as compared to 45% rural children. More than half of the India’s urban poor children are underweight or stunted. In most parts of the country, undernutrition among the urban poor children is more than the rural children. According to NFHS-3 only 39.9 per cent of urban poor children get full immunization against the 65.4 per cent of urban non-poor children. 49.8 per cent of urban poor children under 3 years of age was underweight as compared to 26.2 per cent of urban non-poor children [4].
Figure 3 shows that the urban poor population is on a par with that of the rural population. We can see from the bar of the figure for urban poor children and for rural children that the health condition of urban poor children is not good as much as to the rural children.
Source: UHD 2005-06 based on NFHS- 2005-06.
Figure 3) Health indicators of urban children and overall rural population in India (2005-06)
Annual health survey 2010-11 shows that the neo-natal mortality rate (NNMR) among the empowered action group (EAG) and Assam is very high. Uttar Pradesh has the highest neo-natal mortality 54 and lowest in Jharkhand (26).
From Figure 4, during the period of 2009-10, most of the states showed a sharp decline in infant mortality rate but still there is a long way to go. The IMR is very high in urban areas of the country together with the national level. In Uttarakhand, total IMR is 43 against the 33/1000 in urban areas.
Source: Annual Health Survey, 2009-10, Office of Registrar General of India.
Figure 4) Neo-natal mortality rate, India
According to the Annual Health Survey as shown in Figure 5, likewise Uttarakhand, the Urban areas of other states also shows a high number of infant mortality, as in Rajasthan it is 43/1000 live births, Uttar Pradesh (54), Bihar (44), Assam (35), Jharkhand (26), Orissa (44), Chhattisgarh (40), Madhya Pradesh (50) reported.
Source: Annual Health Survey, Office of Registrar General of India.
Figure 5) Estimated Infant Mortality Rate, India
As from the data above mentioned we can say that the IMR for urban poor for the states of Rajasthan, Uttar Pradesh, Bihar, Chhattisgarh, and Madhya Pradesh is relatively very high or even above the national average of infant mortality rate (47).
Maternal health in urban India
Among the urban population, the maternity services also show the disparity between urban poor and urban population. The proportion of urban poor women received full antenatal care is very low as compared to the urban non-poor women. Although urban India has a relatively very sound and strong healthcare infrastructure with public as well as private management, but there is marked a huge disparity of distribution of service availability, and utilization of resources within the regions between rich and poor.
About 56,000 women die each year in childbirth, which accounts almost 19 per cent of the world. On the one side India show economic progress but on the other side, the country still faces the heavy burden of maternal deaths. As shown in Figure 6, according NHP (2011) the MMR for India is 212/100,000 live births. 44.4 per cent of urban poor women have access to institutional deliveries against the 67.5 per cent of urban non-poor women [5].
Source: NFHS-3.
Figure 6: Births in health facilities in urban and rural areas (%), (2005-06)
Utilization of healthcare services is poor among urban poor women as compared to urban non-poor women. The primary health facilities have not increase in proportion to the growth of the urban poor population. As per to the Figure 7 only 54.3 per cent of urban poor mothers have at least 3 antenatal care checkups during pregnancy, while it is 83.1 per cent for urban non-poor women and 43.7 per cent for rural mothers [6].
Source: NFHS-3.
Figure 7) Mothers who had at least 3 antenatal care visits (%), (2005-06)
According to the Figure 8, 56.0 per cent deliveries among urban poor families are home deliveries, against 21.5 per cent home deliveries among the urban non-poor families. The percentage for rural women is also quite high; it is 71.1 per cent for rural women as compared to 32.6 per cent of urban women [7].
Health of urban slums in India
Urbanization is not a new process; it starts with the industrial revolution in Western Europe, when people start migration from rural to urban areas in search for jobs, and satisfactory life style. It is common knowledge that slums lack basic need services like, safe drinking water, healthcare facilities, sanitation, housing problems, education etc. The lack of these basic services has both direct and indirect effect on the health of the urban slum dwellers. Since independence, urban health is not at the focus of the public health practitioners because India viewed as to be a rural based society and most of the population belongs and lives in rural India and, thus, the government conception of public healthcare is almost rural oriented.
Figure 9, shows the share of states slum population to India’s total population. According to the census 2011, the states with highest contribution to the slum population are Maharashtra (18%), Andhra Pradesh (15.6%), West- Bengal (9.8%), Uttar Pradesh (9.5%), and Tamil Nadu (8.9%).
Understanding public health needs in urban slum areas demands a different framework. Generally, we thought that the alleviation of poverty is the most important weapon of improving general health. But in urban slums areas, the income for the poor increase marginally, which does not assure a better health condition due to the un-affordability of safe drinking water and air. The poor of the urban areas are driven to the outer space of urban, where living conditions are the most degraded and has a little economic value.
The relative difference in urban areas income and wealth is much more than the rural areas. The urban non-poor has a higher purchasing power which drives up the demand for food and healthcare services, making them unaffordable to weaker section or urban poor. Urban policy makers look upon poor as the root of every problem. They impose penalties and pass laws on the urban poor, such as deny them the right to housing, refusing them a ration card. Thus, the slums become more vulnerable and face many socioeconomic problems in urban areas [8-10].
Health challenges in urban slums
• Poor access to healthcare- although slums live in close to many healthcare centers, but they generally have little access to high quality healthcare.
• Large proportion of urban poor not notified- a large proportion of migration to into urban areas, is in search of employment. When they arrive, most migrants find only one affordable housing option: illegal settlements, where they use plastic sheets, discarded scrap of metal, and mud for house making. The slums in urban India which are making cities denser and crowded, lack not only basic civil or social services of government but also political recognition. According to NSSO (2002) around 49.4 per cent of slums are nonnotified in India, and due to the delays in updating official slums data many slums remain unlisted for years and continued to be deprived from these governmental services.
• Environmental condition- access to safe and clean drinking water is the basic human right and forms an important component of primary health care. Provision of safe drinking water show an effective heath intervention which has shown to reduce the mortality caused by food poisoning. Environmental condition not only causes more sickness and mortality but also causes low productivity, lower school enrollment etc. Access to safe and clean drinking water among urban slums is very poor as compared to the urban average: about half of the urban slums do not receive safe drinking water or piped water.
• Under-utilized public health infrastructure- a single primary health care center in an urban area serves a greater proportion of population compared to the norm of 1 center for every 50,000 population. From the provider side it is an enormous challenge to provide health care for such a large population covered by a single health worker. Also, there is an imbalance focus on curative care, and a neglect of preventive and primitive care. There is an over-emphasis in urban areas on the super-specialty centers in private sector which are totally out of reach of the urban poor. A large number of positions of health workers or officers are vacant at the primary health centers, which are supposed to serve the slum population. Table 2 is illustrating urban slum and non-slum population from 2005-06.
| Urban poor | Urban non-poor | Overall urban | All India | |
|---|---|---|---|---|
| Higher order births (%) | 28.6 | 11.4 | 16.3 | 25.1 |
| Births assisted by a doctor (%) | 50.7 | 84.2 | 73.4 | 46.6 |
| Children completely immunized (%) | 39.9 | 65.4 | 57.6 | 43.5 |
| Children age 0-5 months exclusively breastfed (%) | 44.7 | 38.6 | 40.7 | 46.4 |
| Household access to piped water supply (%) | 18.5 | 62.2 | 50.7 | 11.8 |
Table 2: Health indicators for urban slum and non-slum population, 2005-06
Under-five mortality among slum and non-slum children
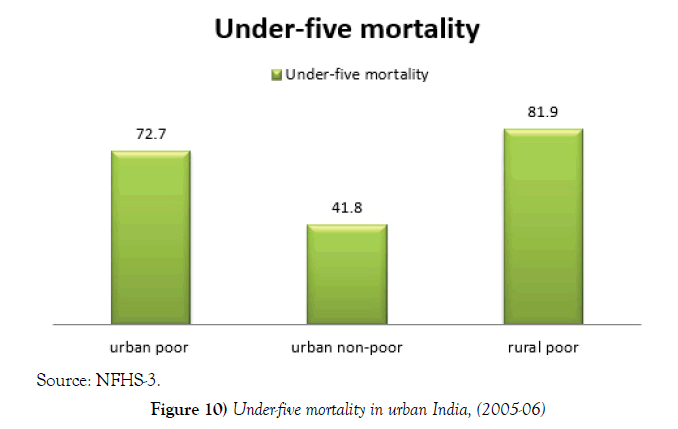
Figure 10 shows the under-five mortality (U5MR) among the urban poor and urban non-poor children for 2005-06. The under-five mortality is 72.7 per 1,000 live births in the urban poor families and 41.8 per 1,000 live births in the urban non-poor families.
Children’s are the most vulnerable section in the urban slum areas because they spent most of their time in and around the area. Children’s have very weak immune system, they expose to many communicable and non-communicable diseases from their elder counter-parts which affect their health both directly and indirectly. Here we show the mortality data of under five years children, but the health condition of child under 3 years, infant mortality, neo-natal mortality, underweight, stunted etc. also did not show a good performance.
CONCLUSION
The paper shows the inequalities in urban health among urban poor and non-poor. Paper also highlights the inequalities in the selected states of India between urban poor and non-poor population.
The urban poor in India are the most vulnerable section of the urban population regarding the health indicators showed in this paper, and for many indicators the differentials is very high. Almost all of the urban poor population has less access to healthcare facilities as immunization, antenatal care, delivery by health professionals etc. Infant and child undernutrition is also very high among the urban poor population or rather more than the rural population.
The figures presented in the paper clearly point towards the urban slum population for a better counting, and for more focused steps to facilitate the large proportion of the urban poor who faces inequalities in health status, access to healthcare facilities, although they are living in the urban areas that are becoming the economic power in the country. Thus, there is an urgent demand to focus on the urban health, with the given pace of urbanization, the increasing number of urban slum with little access to healthcare facilities to cater to the essential living needs of urban population [11].
REFERENCES
- Agarwal S, Sangar K. Need for dedicated focus on urban health within national rural health mission. Indian J Public Health. 2005;49(3):141-51.
- http://pdf.usaid.gov/pdf_docs/Pnadk385.pdf
- Ramachandran R. Urbanization and urban system in India. New Delhi: Oxford University Press. 2001.
- http://nbo.nic.in/images/pdf/report_of_slum_committee.pdf
- Urban Health Resource Centre, “Health of the urban poor in India; key results from the NFHS, 2005–2006”. 2007.
- Chela C. Environmental Impact on Child Health, Washington DC: Pan American Health Organization (PAHO) and WHO. 2000.
- Ghosh S, Shah D. Nutritional problems in urban slum children. Indian Pediatr. 2004;41(7):682-96.
- Gupta K, Arnold F, Lhungdim H. Health and living conditions in eight Indian cities. National Family Health Survey (NFHS-3) India 2005-06. 2009.
- Mugisha F. School enrollment among urban non-slum, slum and rural children in Kenya: Is the urban advantage eroding? Inter J Edu Development. 2006;26(5):471-82.
- Agarwal S, Taneja S. All slums are not equal: child health conditions among the urban poor. 2005.
- Rao S, Joshi SB, Kelkar RS. Changes in nutritional status and morbidity over time among pre-school children from slums in Pune, India. Indian J Pediatr. 2000;37(10):1060-71.