Pituitary macroadenoma
Received: 20-May-2022, Manuscript No. PULJEDS-22-4979 ; Editor assigned: 24-May-2022, Pre QC No. PULJEDS-22-4979 (PQ); Accepted Date: Jul 25, 2022; Reviewed: 08-Jun-2022 QC No. PULJEDS-22-4979 (Q); Revised: 20-Jul-2022, Manuscript No. PULJEDS-22-4979 (R); Published: 29-Jul-2022, DOI: 10.37532/puljeds.22.6(4).30-33
Citation: Arlotto MIF, Aguero P. Pituitary macroadenoma. J Endocrine Disorders & Surgery 2022;6(4):30-33.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
SM, 65 years old, from Sayago (Montevideo), merchant. He lives with his mother and brother. Schooling: complete basic cycle of Lyceum and UTU. He wanders with an American cane.
Reason for consultation: First consultation for control of pituitary macroadenoma. Consultation with mobile emergency due to a rise insystolic blood pressure of 240 mmHg. She reported neck pain and dizziness as accompanying symptoms, which made walking difficult from the start of the condition. He denies colliding with door frames. No eye trauma. He denies holocranial headache, nausea, vomiting, phosphenes and tinnitus. No chest discomfort, denies dyspnea, palpitations. No syncope, no neurovegetative syndrome. Blood pressure figures are gradually regulated to 140/100 mmHg, and physical examination findings include bilateral 6th nerve palsy, left palpebral ptosis, alteration of ipsilateral extrinsic ocular motility, visual acuity and horizontal diplopia of less than 24 hours of appearance.
Keywords
Pituitary macroadenoma; Holocranial headache; Nausea; Vomiting; Phosphenes and tinnitus
Introduction
Patronymical record
SM, 65 years old, from Sayago (Montevideo), merchant. He lives with his mother and brother. Schooling: complete basic cycle of Lyceum and UTU. He wanders with an American cane.
Reason for consultation
First consultation for control of pituitary macroadenoma
History of current illness
He or She, The patient is male or female: Consultation with mobile emergency due to a rise in systolic blood pressure of 240 mmHg. She reported neck pain and dizziness as accompanying symptoms, which made walking difficult from the start of the condition. He denies colliding with door frames. No eye trauma. He denies (I prefer report tan denie) holocranial headache, nausea, vomiting, phosphenes and tinnitus. No chest discomfort, denies dyspnea, palpitations. No syncope, no neurovegetative syndrome. Blood pressure figures are gradually regulated to 140/100 mmHg, and physical examination findings include bilateral 6th nerve palsy, left palpebral ptosis, alteration of ipsilateral extrinsic ocular motility, visual acuity and horizontal diplopia, of less than 24 hours of appearance.
Current illness
Sent for evaluation due to pituitary adenoma, a diagnosis was made by MRI to evaluate ocular alterations. Patient who is currently without headache, without vomiting and persists with decreased visual acuity and bilateral palpebral ptosis. No increase in size of hands and feet. Not prognathism. He does not refer dental malocclusion, which has required prosthesis changes. Not macroglossia. No change in voice. He denies an increase in acral parts, not changes in the number of shoes [1].
• Not hyperhidrosis. Not skin tags.
• No dyspnea, denies obstructive sleep apnea syndrome.
• No muscle weakness, no paresthesias, or dysesthesias.
Refers decreased libido, impossibility of erection, impotence. Reports decreased muscle strength. We do not have infertility studies. No decrease in body hair. No change in frequency of facial shaving. He denied unilateral or bilateral spontaneous galactorrhea Not gynecomastia. He denies fragility fractures [2].
• No facial plethora. It denies stretch marks. No easy bruising or bruising. core obesity.
• No cold intolerance, no dry skin, no nail fragility, no constipation.
• No asthenia, no adynamia, denies anorexia. No orthostatic hypotension. He denies increased fluid intake, not increased thirst [3].
Case Presentation
Personal history
Metabolic pole obese, long standing, refers obesity since childhood, does not remember maximum weight. He refers motivation to lose weight, although he presents elements of anguish due to previous failed attempts. Currently without control with nutritionist. Not habitual snorer, not daytime sleepiness. No fetal macrosomia? No gastroesophageal reflux, no hepatic steatosis, no gallstones. Not knee pain. No hemorrhoidal pathology. No chronic venous pathology of the lower limbs. Hypertensive of 10 years of evolution, irregular hyposodium treatment. Pharmacological treatment with Valsartan 80 mg/day. Chronic global heart failure under control with cardiology. Dyslipidemia, does not comply with hygienic dietary or pharmacological treatment [4].
Bone pole: walks with an American cane, with a slight increase in the base of support, due to persistent decreased visual acuity and dizziness. No falls from his height, no spontaneous fractures. Lack of adequate dairy intake. He does not take chronic corticosteroids. He does not receive Vitamin D. He denies any history of osteoporosis in his family. Former smoker does not know how to specify the number of cigarettes. Occasional consumption of alcoholic beverages [5].
Family background
Hypertensive father, unknown other history.
Results and Discussion
Physical exam anthropometric
Data
• Weight: 129 kg, height: 1.84 m,
• BMI: 38.1 kg/m2. BP: 140/90 mmHg. Good general condition, lucid, collaborates with the interrogation. No acromegalic fascia.
• Biotype: Android distribution of fat, with predominance of the visceral abdominal component.
Skin: Suitable temperature. Presence of acanthosis nigricans in the neck fold. No facial plethora. No lesions or wine red striae on the abdomen. No easy bruising, no bruising. Mucous membranes: normo colored.
Neck: Skin without lesions, centered visceral axis, short neck, thyroid gland not seen or palpated, no lymphadenopathy palpated.
Thorax: No dorsal hump, no blown holes. Symmetrical breasts are visualized, no gynecomastia, bilateral negative breast expression.
Cardiovascular: Cardiac apex is not seen or palpated, distant sounds, regular rhythm of 85 rpm. No maneuvers are performed to verify orthostatic hypotension, given the patient's conditions. In the room he uses a wheelchair to get around.
Pleuropulmonary: Eupneic, mav present bilaterally, no rales. Abdomen: globular, depressible, painless, without visceromegaly. Genitals: it was not performed due to the patient's refusal.
NMS: Psychism described, emotional lability during questioning. Muscular strength and sensitivity preserved. No neck stiffness.
Cranial nerves: Bilateral sixth nerve paresis, greater to the left. Impressive paresis of the third nerve to the left. Pupils in intermediate position, reactive to light, symmetrical.
Visual field by confrontation: At the time of the exam, visual field without particularities. Mild left ptosis, bilateral abduction deficit and supraversion.
Humoral paraclinic
06/12/2019: FSH 1.2 mIU/ml (1.5 to 12.4) LH 1.5 mIU/ml (1.7 to 8.6) TSH 1.50 uU/mL (0.27 to 4.2) FT4 1.24 ng/dl (0.93 to 1.70) basal ACTH and cortisol at 8:00 am, for evaluation of the adrenal axis: ACTH 11.6 pg/mL (7.2-63.3) cortisol 10.7 ug/dl (Basal Hour 8: 4.8-19.5) Ac. Ú rich 5.8 mg/dL urea 31.00 mg/dL creatinine 0.79 mg/dL. CKD EPI calculated: 94.2 mL/min/1.73 m2. PRL of 982.1 ng/ml stands out, which we will analyze, and magnetic resonance of the skull (06.04.19) that reports a pituitary adenoma in the sellar region, which enhances with gadolinium, of 13 mm × 22 mm × 16 mm in its L diameters, T and AP respectively, lateralized to the right, involving the ipsilateral cavernous sinus [6].
Positive diagnosis
This is a male patient, older adult, due to being 65 years of age or older, who presented a pituitary tumor in the sellar region, measuring 13 mm × 22 mm × 16 mm in its L, T and AP diameters. Respectively, in the case of a pituitary macroadenoma, since it measures more than 10 mm by definition. Clinically it is expressed by dizziness and compromise of III and VI cranial nerves. The adenoma is lateralized to the right, compromising the ipsilateral cavernous sinus, with extension to the suprasellar cistern, where the pituitary stalk is lateralized to the left. It does not compromise the optic chiasm, the one that is not altered at the time of the examination agrees with visual field by confrontation without alterations, and that will be assessed with computerized visual field.
Regarding the pituitary axes, functionally it presents decreased libido, impossibility of erection due to compromise of the pituitary gonadal axis and decreased muscle strength. Presents with the clinical absence of other pituitary deficits or hyperfunction that lead to the compromise of other pituitary trophins. The deficits can be oligosymptomatic, and paraclinical tests are needed for their evaluation. The proposals against pituitary macroadenoma are prolactinoma, defined as a Prolactin secreting adenoma (PRL), represents 40% of all pituitary adenomas, which we confirmed by prolactinemia of 982.1 ng/ml and imaging studies. Pituitary apoplexy, clinical syndrome caused by hemorrhage or abrupt ischemia of the pituitary gland, generally in the context of a pituitary adenoma, and which presents clinically with severe onset headache, associated with visual disturbances or ocular paresis. All this is presented in the context of a patient with metabolic syndrome, defined as a set of risk factors, such as atherogenic dyslipidemia, high blood pressure, dysglycemia, prothrombotic and proinflammatory state.
Differential diagnosis
A co-secretory (or multi-secreting) tumor may be considered of prolactin and growth hormone, which occurs in 10% of cases, although the patient does not present clinical elements of acromegaly (increased post pubertal growth hormone secretion). Etiology diagnosis In our patient, given the visual alterations, an MRI was performed and where a pituitary adenoma was diagnosed, in the study of the macroadenoma we made a diagnosis of prolactinoma. Prolactinoma represents approximately 40% of all pituitary tumors and 50-60% of functional pituitary tumors. The prevalence is approximately 10/100,000 in men, with a peak prevalence between 24-35 years of age. According to their size they are classified as: microadenomas (<10 mm), macroadenomas ( ≥10 mm ), giant ( ≥40 mm). In the male sex, they present as macroadenomas, since they are diagnosed late as a consequence of the delay in consultation. When faced with hyperprolactinemia, other secondary causes should be ruled out of the physiological causes, in our patient He denies traumatic injuries such as herpes zoster, chest burns (due to neurogenic mechanisms). No stress, no exercise, no AMI, no hypoglycemia. From the pharmacological causes to the questioning, he denied taking drugs that cause hyperprolactinemia.
Etiopathogenic and physiopathological diagnosis
Prolactin is a polypeptide hormone synthesized and secreted by lactotroph cells. The gene that encodes it is located on chromosome and belongs to a superfamily of genes that encode various polypeptide hormones, such as GH. In the male, prolactin increases the number of LH receptors on Leydig cells and testosterone secretion. It seems to have some action on sperm motility. This hormone is produced in a pulsatile manner by the pituitary gland and its concentration varies throughout the day. Its maximum peak usually occurs during sleep (between 4 and 7 hours) and decreases throughout the day. The secretion is inhibited by the hypothalamus by one or more factors (PIF). Dopamine is the most important PIF, it is secreted in the arcuate nucleus of the hypothalamus and transported through the portal system to the pituitary gland, inhibiting prolactin secretion through D2 receptors [7,8].
Substances that stimulate prolactin secretion
Dopaminergic receptor blockers (metoclopramide, phenothiazines), TRH, Vasoactive Intestinal Peptide (VIP), bombesin, neurotensin, histidine methionine peptide, estrogens. Substances that inhibit prolactin secretion: dopamine or precursors (levodopa), GAP (gonadotropin associated peptide; it is in the carboxyterminal region of GNRH), GABA (gamma aminobutyric acid), glucocorticoids, thyroxine. Pathophysiological mechanisms of hyperprolactinemia hypothalamic dopamine deficiency diseases, drugs that deplete dopamine stores. As there is no inhibitory factor, PRL synthesis increases. Defect in the dopamine transport mechanism to the pituitary. Pituitary stalk section (tumors, trauma). Insensitivity of lactotroph cells to dopamine: drugs that block the action of receptors, decreased number of D2 receptors. Hyperstimulation of lactotroph cells: hypothyroidism, chest injuries, estrogens. Clinical manifestations are due to both hyperprolactinemia and mass effect. Hyperprolactinemia alters GnRH pulsatility and inhibits LH and FSH secretion, causing hypogonadotropic hypogonadism and, therefore, in men, erectile dysfunction, decreased libido, and infertility. 80% of prolactinomas in men are macroadenomas and, therefore, show neurological manifestations and clinical signs due to the mass effect on neighboring structures, nausea, vomiting, and visual disturbances due to cranial nerve involvement, hypopituitarism due to compression of the gland and stem. Ocular dysfunction associated with pituitary macroadenoma can be of three types: oculomotor restriction (unilateral or bilateral), visual field defects (<5% of cases), in the context of pituitary apoplexy, even rarer nystagmus. Anatomical bases of oculo motor dysfunction the oculomotor restriction is due to lesions of the cranial or culomotor nerves III (oculomotor), IV (trochlear), and VI (abducens), between the brainstem and the orbit. In pituitary adenomas, the lesion involves the cavernous sinus. It is a structure where veins converge on each side of the Turkish saddle, which contains the pituitary gland. Deficits in eye movements strongly suggest pituitary apoplexy, especially in macroadenomas. It can be produced by two mechanisms: direct, by compression of the nerve by the tumor, or indirect, by compression through the wall of the cavernous sinus. The latter case usually occurs, it is more common in rapid tumor growth, as in apoplexy, followed by intratumoral hemorrhage or ischemic tumor infarction. Of the three oculomotor cranial nerves, the third pair is the most frequently affected, although it is rarely isolated; nerves IV and VI can also be involved. From the patient's report and physical examination, ocular paresis demonstrated the presence of diplopia. Complete paralysis of nerve III is common, and induces complete or partial paralysis in some of the innervated muscle fibers. IV nerve palsy causes difficulty looking down, and VI nerve palsy induces abduction deficit. Field diagnosis This is a male patient, older adult, obese, presenting a BMI ≥ 32 kg/m (In physical exam you said Poids:129 kg, Taille:1,84 m, IMC:38,1 kg/m2) classified as grade I, according to the adjusted values for this age range, with mechanical repercussions of the same, integrating the entity called metabolic syndrome, given by stage 1 arterial hypertension according to the JNC classification due to current BP figures of 140/90 mmHg, and dyslipidemia, both with irregular compliance with hygienic dietary and pharmacological treatment. There are no fasting blood glucose records to complete the metabolic assessment. In the bone pole, he walks with an American cane, although he does not present predisposing factors for osteoporosis on interrogation, prolactin generates an inhibitory effect on sexual steroids, associating a decrease in bone mass. Without dairy contributions. The guide of the American College of Endocrinologists, AACE of 2016, recommends 1,000 IU daily of Vitamin D, in this age group, although obese people usually require more to maintain vitamin D levels above 30 ng/mL. The adequate requirements for this patient are calcium 1200 mg/day, with an estimated decrease in fracture risk of 15% 10 PARACLINIC GOALS confirm the diagnosis of hyperprolactinemia and its etiology. Evaluate structural and functional repercussions. Assessment of the patient's terrain. In order to carry out an adequate treatment [9,10].
Measurement of prolactin prior to treatment: Ideally, its dosage is done in the same laboratory, after 9 am, since it increases with sleep, without venipuncture stress. Slightly elevated values should be confirmed 3. In our patient, prolactin by the ECLIA technique was 982.1 ng/ml (NV: 4.0-15.2) for men aged 20 to 70 years. The diagnosis of Macroprolactinoma is confirmed. Assessment of structural and functional repercussions
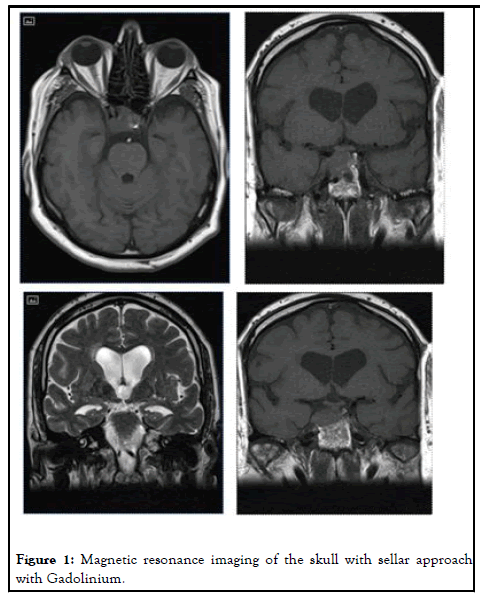
Structural repercussion: Magnetic resonance imaging of the skull with sellar approach with Gadolinium (Figure 1) [11-13].
In the sellar region, a solid isointense lesion is observed on T1, hypertensive and heterogeneous on T2, which enhances with gadolinium. It measures 32 mm × 22 mm × 16 mm in its L, T and AP diameters respectively. It is lateralized to the right, compromising the ipsilateral cavernous sinus, encompassing the carotid artery. It extends to the suprasellar cistern; the pituitary stalk is lateralized to the left. The optic chiasm appears normal, without lesions, with normal appearing intracranial optic nerves and no focal lesions.
Diagnostic conclusion: Findings probably related to a pituitary macroadenoma with involvement of the right cavernous sinus, consultation with ophthalmology.
Computerized Visual Field: Pituitary adenomas can lead to blindness or other causes of visual dysfunction in 58%, and oculomotor disorder. In some cases, patients do not immediately recognize this latter deficit, since the latter is compensated with the vision of the other eye. In our patient, the ocular deficit and paresis developed acutely. It is for this reason that we must evaluate visual acuity, visual field to the confrontation and computerized, and eye fundus. We do not have this information, the patient did not attend consultation. General impact assessment. For this, hormonal dosages are requested: Normal thyroid axis. Secondary adrenal insufficiency is ruled out. IGF-1 not available, although requested.
Assessment of metabolic syndrome: He presents altered fasting glycemia, the study is repeated. I didn’t see his glycemia Hyperuricemia is requested since it is associated with metabolic syndrome. Calculated CKD-EPI 48.6 mL/min/1.73 m2, corresponding to stage III chronic kidney disease, kidney damage with moderate decrease in glomerular filtration rate 2,3,4. hepatic enzymogram, requested to assess hepatic stenosis linked to obesity, which does not present alterations. We do not have a lipid profile, although it was requested 2,3,4. Echocardiogram doppler report from 06.11.19. Left ventricle of normal dimensions with increased parietal thickness. LV mass 156 g/m2. Normal systolic function without sectorial contractility disorders. diastolic dysfunction. Slightly dilated left atrium. Morphologically normal trileaflet aortic valve without pathological flows. Morphologically normal mitral valve, without pathological flows. In short severe concentric LVH. LA dilation. Normal LVEF of 60%. Diastolic dysfunction.
Treatment
Is oriented in our patient, to normalize prolactin levels and reduce tumor size. Medical treatment with dopaminergic agonists is the first line treatment for prolactinomas. And prolactinoma is a hormone sensitive tumor its efficacy in reducing PRL, correcting hypogonadism and reducing tumor size is 80/90% in microprolactinomas and 70% in macroprolactinomas. was started with cabergoline, which is a dopaminergic agonist drug of the dopamine D2 receptor, not ergotamine. Its half-life is long, 7 days, and it can be administered orally 1 or 2 times a week, which improves adherence to treatment.
Indicated initial dose: Cabergoline 0.25 mg once a week. Its most frequent adverse effects are nausea, vomiting, headache, postural hypotension, drowsiness, vertigo, nasal congestion. In a 2008 meta-analysis, it was studied whether there was any relationship between cabergoline for the treatment of hyperprolactinemia and clinically significant valve disease. Many clinicians gave the first warnings about the possibility of the association of the development of restrictive valve disease in patients with parkinson's disease and hyperprolactinemia. The echocardiographic pattern demonstrated severe mitral regurgitation. According to this fact, follow up with an echocardiogram every 6-12 months was recommended. The primary endpoint of this study was the development of moderate or severe valvular regurgitation in any of the four valves. In them, severe regurgitation is rarely observed, so a second point of study was the development of mild or moderate valvular regurgitation in any of them. Data were extracted from 836 patients treated with cabergoline, from 13 studies, and the significant finding was mild tricuspid valve regurgitation, although it is important to establish that its injury is detected by cardiac symptoms. We highlight the study by Colao et al., which found a higher prevalence of moderate tricuspid regurgitation. The cumulative risk dose has not yet been established, and routine echocardiography is not essential in patients in the first 2 years of treatment with weekly cabergoline 1-2 mg, unless there are clinical factors that advise it. It is suggested in those with doses greater than 2 mg weekly and duration greater than 5 years.
Monitoring and evolution
Follow up is clinical, biochemical and imaging. Once treatment is started, a decrease in PRL is observed at 2-3 weeks. The decrease in tumor size is later. PRL measurement prolactin dosage a month after starting treatment, with dose adjustment according to the results, with a frequency between 1-3 months after dose adjustment. Once the PRL dose is normalized, PRL is requested every 6-12 months. New paraclinical on 07.11.19, receiving cabergoline 0.25 mg per week. Prolactin with ECLIA technique: 181.9 ng/ml (range men 20 to 70 years old, 4.0-15.2 ng/ml) this dosage is the only one registered, given that the patient is difficult to follow up, as he does not attend endocrinology consultations.
Computerized visual field: one month after treatment and then according to clinical evolution. Again, we do not have this record. Imaging: the procedure to follow is to request a new MRI of the skull with a sellar approach with gadolinium 6 months after starting treatment to assess the reduction in tumor size. Subsequent imaging follow up will be performed according to clinical evolution. Bone densitometry, due to increased risk of osteoporosis due to hypogonadism. The rest of the pituitary function, in this case, as it is a macroadenoma, I request it at the beginning and then according to its evolution.
Complications
Due to the treatment-side effects of cabergoline: Nausea, arterial hypotension, dizziness, mental confusion, which are minimized by starting with small doses, our patient did not present them.
Conclusion
Vital and functional prognosis is subject to treatment compliance and response. In case of abandonment of treatment, complications such as: Tumor growth with aggravation of the elements of intracranial hypertension, and greater visual compromise. Continue with hypogonadism and have repercussion effects on: bone mineral density and the cardiovascular system. Our patient has major cardiovascular risk factors. Men with prolactinomas have an increased risk of incidence of cardiovascular disease.
Diseases associated with metabolic syndrome: Type 2 diabetes mellitus, hepatic steatosis, obstructive sleep apnea syndrome, chronic kidney disease. Alterations in fertility until normalization of prolactin. In our patient we found FSH/LH deficiency. We cannot propose treatment now, until the prolactin value is corrected.
References
- Varela Pinedo LF. Health and quality of life of the elderly. Rev Peru Med. Public Health Exp. 2016;33(2).
- Blanco Carrera C, Fernandez Fernandez C, Escribano Taioli P. Functioning pituitary adenomas. Medicine. 2016; 12(15): 838-49.
- Melmed S, Casanueva F, Hoffman A, et al. Diagnosis and Treatment of Hyperprolactinemia: An Endocrine Society Clinical Practice Guideline. 2020. J Clin Endocrinol Metab. 2011; 96(2): 273-288.
[Crossreff] [Googlescholar] [Indexed]
- Snyder PJ. Management of hyperprolactinemia. Literature review current though. 2020.
- Civeira Murillo F, Perez Ruiz MR, Baila Rueda L.et al. Metabolic Syndrome: concept, epidemiology, etiopathogenesis and complications. Medicine. 2013; 11(40):2402-9.
- Lucie A, Alain V, Maud L, et al. Neuro ophthalmologic exploration in non-functioning pituitary adenoma. Ann Endocrinol. 2019; 76: 210-19.
[Crossreff] [Googlescholar] [Indexed]
- Ribeiro DBM, Balarini LG, Severo AMA, et al. Prolactinomas may have unusual presentations resulting from massive extrasellar tumor extension. Arch Neuropsychiatr. 2019;74 (7):544-548.
[Crossreff] [Googlescholar] [Indexed]
- Delbono M, Chaftare Y, Perez L, et al. Practical manual of adult obesity. Primary care. Honorary Commission for Cardiovascular Health. Montevideo. Uruguay. 2009.
- Bell K, Twiggs J, Olin BR, et al. Continuing education. The silent killer: Updated JNC-8 Guideline Recommendations. 2015;1(8).
- Pauline MC, Steven MP, Neil B, American Association of Clinical Endoclinologists and American College of Endocrinology Clinical Practice Guidelines for The Diagnosis and Treatment of Postmenopausal Osteoporosis. Endocrine Practice. 2016;22(4):1-42.
[Crossreff] [Googlescholar] [Indexed]
- Craig ES, Eugene TTW, Jonathan P, et al. A meta-analysis of the prevalence of cardiac valvulopapathy in patients with hyperprolactinemia treated with cabergoline. J Clin Endocrinol Metab. Consultado en 2019;104: 523-38.
[Crossreff] [Googlescholar] [Indexed]
- Toulis, Robbins, Balachandran, et al. Males with prolactinoma are at increased risk of incident cardiovascular disease. Clinical Endocrinology. Consultado en 2019;88: 71-6.
[Crossreff] [Googlescholar] [Indexed]
- de Rosa, Ciccarelli, Zarrilli, et al.The treatment with cabergoline for 24 months normalizes the quality of seminal fluid in hyperprolactinaemic males. Clinical Endocrinology. Consultado en 2019;64: 307-13.
[Crossreff] [Googlescholar] [Indexed]