Pleuro pulmonary blastoma presenting as bullous disease of the lung in an infant
2 Department of Pediatric Pulmonology, G Kuppuswamy Naidu Memorial Hospital, Coimbatore, Tamil Nadu, India
3 Department of Pathology, G Kuppuswamy Naidu Memorial Hospital, Coimbatore, Tamil Nadu, India
Citation: Sundaram M, Raju V, Poddar A, et al. Pleuro pulmonary blastoma presenting as bullous disease of the lung in an infant. Surg Case Rep. 2018;2(2):28-9.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A pleuro pulmonary blastoma (PPB) is a very rare and aggressive malignant tumour of lung in infants and children. Varying clinical and radiological presentation of pleuro pulmonary blastoma has been described. In this report, we are reporting an infant who presented with respiratory distress due to large bullae of the left lung and diagnosed to have pleuro pulmonary blastoma of the lung. bleeding. However follow-up is required to ensure complete resolution of the haemorrhage and to rule out a true adrenal mass. We report a case of unilateral adrenal haemorrhage secondary to motor vehicle accident.
Keywords
Pleuro pulmonary blastoma; Bullous disease; Cystic lesion of the lung; Respiratory distress
Primary pulmonary neoplasms are uncommon in children. One such tumor, pleuro pulmonary blastoma (PPB), is very rare, highly aggressive and malignant, and originates from either the lungs or pleura. In this case report, we present a case of pleuro pulmonary blastoma presenting as bullous disease of the lung in an infant.
Case Presentation
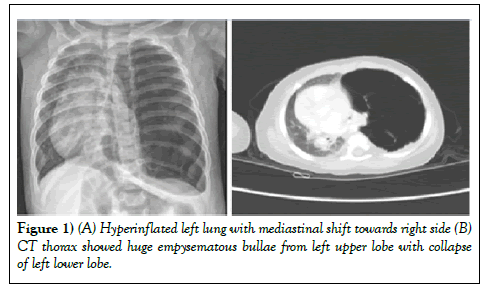
A ten-months-old male infant was admitted in the intensive care unit with worsening respiratory distress since ten days duration. There was no history of fever. On general examination, child had severe chest wall retraction with respiratory rate of 60/min, heart rate of 180/min and room air oxygen saturation of 80%. On Respiratory system examination, Trachea was shifted to the right and there was absent breath sound on the left side. Rest of the system examination were unremarkable. Baseline blood investigations were within the normal range. Chest X-ray showed hyper inflated left lung with mediastinal shift towards right side (Figure 1A). Computed Tomogram (CT) of thorax showed giant emphysematous bulla arising from left upper lobe with complete collapse of left lower lobe. The CT appearance was similar to congenital lobar emphysema.
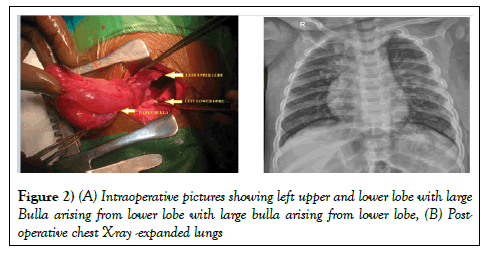
However, there were few dilated vascular channels seen in to the bulla (Figure 1B). In view of persistent respiratory distress, baby was taken up for emergency left thoracotomy and excision of bullae or lobe lobectomy. Under general anasthesia, left posterolateral thoracotomy was performed and chest was entered through 4th intercostal space. There was a hyperinflated large bullae measuring about 10 × 8 cm, arising from the left lower lobe causing the collapse of the entire left lung (Figure 2A).
Patient was then admitted to orthopedic ward for conservative management of fractured right scapular body, right sided ribs, liver contusion and right adrenal haemorrhage. Daily monitoring of liver function and haemoglobin level was done and was normal. He also did not show signs of adrenal insufficiency. He was discharge well after one week. Follow-up of ultrasound abdomen is done at one-month post injury. Figure 3 showed complete resolution of right adrenal haemorrhage, right retroperitoneal haemorrhage and residual liver contusion. No definite adrenal lesion was seen. There were few dilated blood vessels seen at the base of bullae. The entire Bulla was excised (Bullectomy). After bullectomy, both the left upper and lower lobes expanded completely. The entire left lung parenchyma was looking healthy. Chest was closed in the usual manner after leaving a chest tube. Child was extubated on the operating table. Post-operative chest X-ray showed well expanded bilateral lung fields (Figure 2B). Post-operative period was uneventful. Child was sent home on third post-operative day with stable haemodynamics.
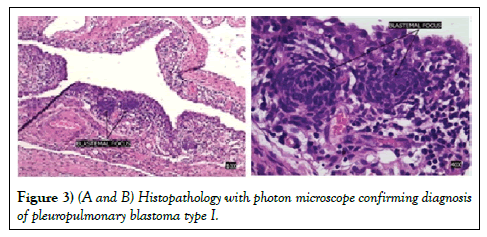
Histopathology of the bullectomy specimen showed features of cystic neoplasm with multi-loculation. The septae consist of fibrous stroma which was lined by the flattened cuboidal epithelium with focal squamous metaplasia with blastemal cells and focal micronodule formation. There was no evidence of rhabdomyomatous differentiation or cartilagenous foci. These findings are in favour of cystic pleuropulmonary blastoma (type I) (Figures 3A and 3B).
The histopathology was discussed with multidisciplinary team including the pediatric oncology team. Ultrasound (USG) abdomen ruled out other associated intra-abdominal pathology. In view of complete surgical resection and type I of pleuro pulmonary blastoma child was advised regular follow up without any adjuvant chemo or radiotherapy. At the end of one year follow up, the child is doing well with no evidence of local recurrence.
Discussion
Pleuro-pulmonary blastoma (PPB) is a rare primary lung malignancy, comprising only 0.25–0.5% of all malignant lung neoplasm and less than 1% of all primary malignant lung tumors in the pediatric population (1). PPB usually presents like cystic lesions of the lungs. It is often diagnosed initially as one of the congenital lung lesions before making the final diagnosis especially in the early stage of the disease. PPB can also arise from structures derived from splanchno-pleuric or somatopleuric mesoderm like mediastinum, diaphragm and pleura. Common metastatic sites include the brain, bone, lymph nodes, liver, pancreas, kidney, and adrenal glands. Denher and associates classified PPB into three groups; type I with purely cystic tumors, type II as an intermediate type, and type III with predominantly solid tumors (2). Type I has better prognosis than type II and type III. Type I has better survival compared to type II and III. A progression from type I to type III may occur over time (3). The histologic appearance is variable. The tumor is characterized by primitive blastoma and a malignant mesenchymal stroma often showing multidirectional differentiation as Rhabdomyosarcomatous, Chondrosarcomatous or Liposarcomatous. The cystic component is lined by benign metaplastic epithelium (4). Polysomy of chromosome 8 is a constant feature of pleura-pulmonary blastoma as reported by Vargas et al. with cytogenetic analysis (5). PPB has no special characteristic findings on imaging studies. CT angiogram had picked up a multiple dilated blood vessel in the wall of cystic lesion in this child. The blood vessels are usually absent in the congenital cyst wall or benign cystic lesion. PPB should be considered in the differential diagnosis of all benign cystic lung lesions in children 4. This case report is unique in such a way that PPB had presented like a bullous disease of the left lung with mediastinal shift. This type of clinical presentation has not been reported in the literature sofar. Surgical resection is the mainstay of treatment for the patients with PPB. Type I has better survival compared to type II and III. The five-year survival in type II and type III are around 40% with a combination of therapy. Complete surgical resection alone will be sufficient in patients with type Í disease. Various combinations of chemotherapeutic drugs have been tried as neoadjuvant and adjuvant treatment in type II and type III PPB (6). Chemo-reduction followed by complete excision may be the satisfactory treatment of this highly aggressive tumour in childhood (7). Radiotherapy has shown to be effective in patients with local recurrence. A large series of case studies is required to further analyze and establish a framework for the definite treatment. Pleuro-pulmonary blastoma should be considered as one of the differential diagnosis in infants and children presenting with any lung pathology. High index of suspicion is mandatory for early detection. Early detection and complete resection of the tumour may favour a better clinical outcome.
Conclusion
Pleuro-pulmonary blastoma should be considered as one of the differential diagnosis in infants and children presenting with any lung pathology. High index of suspicion is mandatory for early detection. Early detection and complete resection of the tumour may favour a better clinical outcome.
REFERENCES
- Calabria R, Srikanth MS, Chamberlin K, et al. Management of pulmonary blastoma in children. Am Surg. 1993;59(3):192–6
- Dehner LP, Watterson J, Priest J. Pleuropulmonaryblastoma: A unique intrathoracic- Pulmonary neoplasm of childhood. PerspectPediatrPathol. 1995;18:214.
- Wright JR. Pleuropulmonaryblastoma: A case report documenting transition from type I [cystic] to type III [solid]. Cancer. 2000;88(12):2853–8.
- Priest JR, McDermott MB, Bhatia S, et al. Pleuropulmonaryblastoma: A clinico-pathological study of 50 cases. Cancer. 1997;80(1):147–61.
- Vargas SO, Nose V, Fletcher JA, et al. Gains of chromosome 8 are confined to mesenchymal components in pleuro-pulmonary blastoma. PediatrDevPathol. 2001;4(5):434–45.
- Indolfi P, Casale F, Carli M, et al. Pleuropulmonaryblastoma: management and prognosis of 11 cases. Cancer. 2000;89(6):1396–401.
- Çorapçioglu F, Liman T, Aksu G, et al. A case report with type II pleuropulmonary blastoma: Successful treatment with surgery and chemotherapy. The Turkish Journal of Pediatrics. 2009;51(1):78–81.