Medication management in tertiary care hospitals
Received: 06-Dec-2017 Accepted Date: Dec 20, 2017; Published: 02-Jan-2018
Citation: Raval S, Kapadia N, Gadhave P, et al. Medication management in tertiary care hospitals. J Nurs Res Pract. 2018;2(1):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Medication management is one of the vital parts of patient care. Medication errors occurring most commonly in prescribing, dispensing or administration. Research from the USA suggests that medication errors often result from lack of sufficient information during the prescribing stage. Other work from the USA has estimated that each adverse drug event costs $2000–2500.
Medication management includes Prescription, Medication Reconciliation, Transcription, and Appropriateness review, Dispensing, Administration, Monitoring and Discardation of medications. Doctor follows the prescription writing rules, Pharmacists follows storage and Dispensing rules and Nurse follow the six rights of administration which is result in better outcomes of patient care.
High alert drug management is also very important for patient safety. Effective medication management and involvement of pharmacists in process can reduce the patient’s medication cost and over all reduce the stay of patient in hospitals.
Appropriateness review is most important for prevention of medications errors. Effective review process in tertiary care hospitals can significant reduce the errors happen during prescription and Transcription.
Keywords
Medication management; Patient safety; Tertiary care; Medical officers
Introduction
Medication management in hospitals that medications are selected, procured, delivered, prescribed, Appropriateness Review, administered and Monitored and that is effective for final outcomes of patients care.
There are four pillars of Medication Management i.e., Consultants, Medical officers, Pharmacists and Nurses. Medication management in tertiary care hospitals requires excellent coordination between Doctors, Pharmacists and Nurses which can result for better outcomes.
Safety of the medication in tertiary care hospitals is the main challenging job for Nursing, Pharmacy and Doctors. For improve the safety of medications continue monitoring and Audit need to be done in every stage of use of medications. Medications are flow as prescription, Reconciliation, transcription, Appropriateness review, indenting, Dispensing, Administration, Monitoring and Discard of Medicines [1-3].
Methodology
Prescriptions
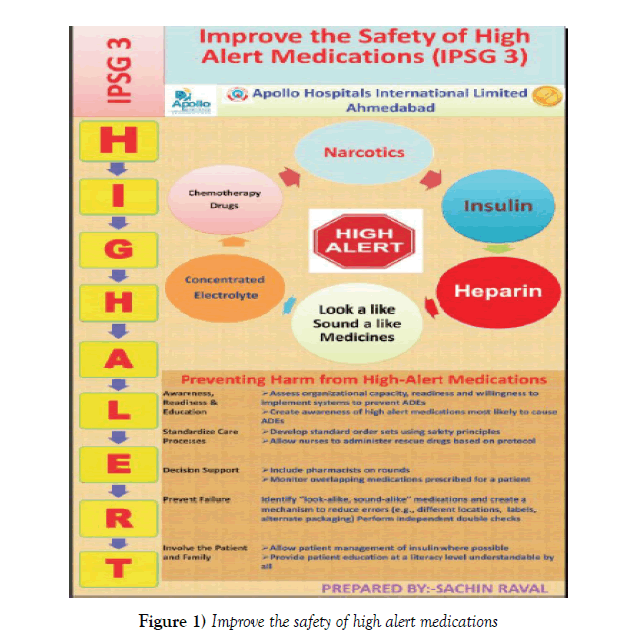
Doctor prescribe medicines should be in Capital writing for avoid confusion of pharmacist and Nursing. Reconciliation of medications need to do with proper reference and verified by Pharmacists. High alert medications should be prescribed with proper instruction for administration (Figure 1). LASA (Look alike and Sound alike medicines) should be prescribed with proper rules. SOS/STAT Order should be prescribed with indications. Narcotic medications should be prescribed with proper rules and regulation and in Triplicate copy. Always use a leading zero before a number less than one (e.g. 0.5 mg) and never use a terminal zero (e.g. 5.0 gm) [4-7]. Prescription should be PAT verified (Prescription Audit Team) for dose, indication, route of medicines, allergy, Physiological information, Drug-drug interaction, drugfood interaction etc. Avoid abbreviations of drug names and preparations as these can be misinterpreted - eg, Mist. Expect. Insulin order must be signed by doctor and preferred to use sliding scale for insulin order to avoid High alert medication errors. Avoid verbal order, if it is follow read back policy to avoid Medication order. Concentrated electrolyte order should be written at designated place in drug chart.
Transcription
Nursing should do transcription of doctor order in his. In any confusion related to brand or dose nursing should confirm with ward pharmacist or Doctor. Indent should be for 24 hours as per unit dose system which help to reduce management of medicines at Bed side. The transcriber must make sure it is complete, including all of the following information: the date, name of medication, how much to take, how to take it, how often, and the physician’s or practitioner’s signature. The transcriber must transfer the order to Drug Chart exactly as the order reads and in legible writing [8,9]. If Nurse cannot read it, medication errors can result that can be fatal to the patient. It continues process for medicines discontinuing/changing in chart. Each time transcriber will have written in new column. Discontinue medicines must be cross check and sign and date by duty doctor. Medication errors due to improper transcription account for roughly half of adverse reactions in patients, which is why it is so important to transcribe medication orders correctly. The person who transcribes medication orders is accountable for any inaccuracies.
Appropriateness Review
Appropriateness should be done after prescription and before indenting, dispensing, and administration of medicines by clinical pharmacists. Clinical pharmacists should have checked following points before indenting and dispensing [10-13].
1. The appropriateness of the drug, dose, frequency, and route of administration;
2. Therapeutic duplication;
3. Real or potential allergies or sensitivities;
4. Real or potential interactions between the education and other medications or food;
5. Variation from hospital criteria for use;
6. Patient’s weight and other physiological information;
7. Other Contraindications.
Dispensing
Dispensing of medicines should be double checked from pharmacy. Dispense medicines should be in unit dose system to avoid medication errors. Storage of medicines should be categorized as per risk related to medicines, Adult, pediatric, High alert, LASA, Refrigerated medicines. LASA (Look alike and Sound alike medicines) should be stored in separate rack and boxes in Pharmacy as well as in wards/ICU. High alert medications should be label and then dispense from pharmacy [14-16]. High alert labeled should be with the indications to avoid High alert errors. Narcotic storage and dispensed with proper accountability and as per government laws. Narcotic must be kept in double locked and dispense with proper documentations. Refrigerated items should be dispensing with ice pack and storage label. Antibiotic and costly medicines should be label which contains patient name, expiry, batch number and qty. Chemicals should be dispensed with proper label and hazardous instructions.
Administration
Administration of High alert medicines should be with senior nursing and double checked. Preparation of medicines should be in aseptic area and dilution should be clear. Follow the medication preparation steps to prevent the infections. Chemotherapy administration should monitor continuously hydration, Cannulation, rate of infusion and premedication. Narcotic medicines administration should be with proper prescription and supervision of doctor only. Documenting administration at the scheduled time, but giving the drug early or late. Identification of the patient to whom the medicine is to be administered. Check that the patient is not allergic to the medicine before administering it. Know the therapeutic uses of the medicine to be administered, its normal dosage, side effects, precautions and contra-indications. Check that the prescription or the label on medicine dispensed is clearly written and unambiguous. Check the expiry date before preparing of medications. Check the weight base medication and dosage. Follow the 6R while administer medications. Right Patient, Right Drug, Right dose, Right Time, Right Route, Right Documentation [17].
Monitoring
Monitoring of drug after administration need to do for ADR. Training for Monitoring of ADR and reporting need to be improve continuously. Chemotherapy vesicants and irritant should be categorized and protocol for monitoring. Should be monitoring Inj Avil and Inj Hydrocortisone consumptions for adverse drug reaction. Chemotherapy monitoring should be every 15 min.
Discard
Proper Discard of medicines is one of the important criteria for global health. Cytotoxic medicines discardation should be compulsory neutralized. Expired medicines need to submit to organization for proper discardation.
High alert medications
High alert medications are medicines that are most likely to cause significant harm to the patient, even when used as intended. The Institute for Safe Medication Practices (ISMP) reports that the incident rates of this group of medicines may not necessarily be higher than the other medicines but when incidents occur the impact on the patients would be serious (significant).
In seeking to improve patient safety, the primary focus should be on preventing errors with the greatest potential for harm. Many of the highest risk medications – e.g., concentrated electrolyte, Chemotherapy Drugs, Narcotics, Insulin, Heparin and LASA are delivered by IV infusion. The most serious and life threatening potential adverse drug events (ADEs) are IV drug related [18].
Discussion
From the above our review it observed that preventing the harm from High alert medications, is a need and some key points are:
1. Awareness, readiness, education: Training arranged for Nursing, Pharmacists and Doctors for High alert medication. List develops for High alert medications and showcash in every wards/ICUs. Develop Museum for High alert medications.
2. Standardize care process: Double sign and double check at the time of Dispensing and Administration. PAT (Prescription Audit) verified by clinical pharmacist before indenting. Specific label design for each High alert medicine.
3. Decision support: Include pharmacist on ward round and monitor overlapping medications prescribe for patients.
4. Prevent Failure: Identify LASA Medicines and create mechanism to reduce errors (Different Location and double checking/Labeling).
5. Involve the Patient & Family: Patient counseling in case of insulin. Provide patient education at literacy level understandable by all.
REFERENCES
- Department of Health. Organisation with a memory. London: Department of Health 2001.
- Classen DJ, Pestotnik SL, Evans RS, et al. Adverse drug events in hospitalized patients. JAMA 1997;277:301–6.
- Bates DW, Spell N, Cullen DJ, et al. The cost of adverse drug events in hospitalized patients. JAMA 1997;277:307–11.
- Boyko WL, Yurkowski PJ, Ivey MF, et al. Pharmacists’ influence on economic and morbidity outcomes in a tertiary teaching hospital. Am J Health Syst Pharm 1997;54:1591–5.
- Bednall R, McRobbie D, Russell SJ, et al. A prospective evaluation of pharmacy contributions to post-take ward rounds. Pharm J 2003;271:22–3.
- Dean B, Schachter M, Vincent C, et al. Prescribing errors in hospital inpatients: their incidence and clinical significance. Qual Saf Health Care 2002;11:340–3.
- Nicholls JS, Webb DG. The London and South East Clinical Pharmacy Collaborative on Medication Errors. Medication Error Survey. London Clinical Pharmacy Unit, Northwick Park Hospital, November 2002.
- Grosvenor LJ, Verma R, O’Brien R, et al. Does reporting of plain chest radiographs affect the immediate management of patients admitted to a medical assessment unit? Clin Radiol 2003;58:717–8.
- McFadzean E, Isles C, Moffat J, et al. Is there a role for a prescribing pharmacist in preventing prescribing errors in a medical admissions unit? Pharm J 2003;270:896–9.
- Dodds LJ. An objective assessment of the role of the pharmacist in medication and compliance history taking. Br J Pharm Prac 1982;4:12–24.
- Barber N, Rawlins M, Dean FB. Reducing prescribing error: competence, control and culture. Qual Saf Health Care. 2003;12:i29–32.
- Burns N, Still E. Pharmaceutical care–a model for elderly patients. Hosp Pharmacist 2003;10:66–268.
- Psaila B, Olsen S, Patel T, et al. A multidisciplinary approach to detection and analysis of medication errors in hospital practice; comparing traditional record review with pharmacist interventions (poster). Birmingham: National Patient Safety Agency Conference, February 2004.
- Gaurav Loria. Reduction of harm from high risk medications, Apollo Medicine 2012;9:160-65.
- 2011 Institute for Safe Medication Practices (ISMP) Medication Safety Self-Assessment® for Hospitals.
- Hsaio. Nurses’ knowledge of high -alert medications: instrument development and validation. J Advanced Nursing 66:177-90.
- Lu MC. Nurses’ knowledge of high -alert medications, A randomized controlled trial, Nurse Educ. Today 2011.
- Anderson P. Preventing High-alert Medication Errors in Hospital Patients. Am Nurs Today 2015;10.