Post-obstruction pulmonary edema complicated by transient cardiac dysfunction in a young woman
Received: 26-Dec-2017 Accepted Date: Jan 16, 2018; Published: 22-Jan-2018
Citation: Otsuka T, Nishizawa Y, Yoshino K, et al. Post-obstruction pulmonary edema complicated by transient cardiac dysfunction in a young woman. Anesthesiol Case Rep. 2018;1(1):4-6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A 17-year-old woman who had been healthy since birth developed postobstruction pulmonary edema (POPE) after maxillofacial surgery. She was extubated in a semi-conscious state after general anesthesia, and developed severe airway obstruction due to glossoptosis, and blood and secretions in the oral cavity. When the obstruction was released approximately 10 min later, the chest radiograph showed an increased cardiothoracic ratio, and cardiac ultrasonography showed a reduction in the left ventricular ejection fraction when compared to the normal values for the same age. A diagnosis of type-I POPE with associated left ventricular dysfunction was made, and oxygen and diuretic administration were initiated. When continued hypoxemia is found, even after the elimination of any airway obstruction, it is important to evaluate left cardiac function, with due consideration to the possibility of POPE.
Keywords
Pulmonary edema; Post-obstruction Pulmonary edema; Hypoxemia; Left ventricular dysfunctionIntroduction
Post-obstruction pulmonary edema (POPE) has been defined as non-cardiogenic pulmonary edema that follows upper airway obstruction. It is classified as either type-I POPE, which is primarily negative-pressure pulmonary edema, or type-II POPE, in which venous perfusion is increased by the elimination of expiratory disorders, leading to an increase in hydrostatic pressure in the pulmonary capillaries [1].
In patients developing acute upper airway obstruction, the incidence of POPE has been estimated to be up to 12 % [2]. Laryngospasm during intubation or after anesthesia is reported to be the most common cause of upper airway obstruction leading to POPE in adults, and it has been reported to account for as much as 50% of the cases [3].
This report presents the case of a young woman who had been healthy since birth. She underwent maxillofacial surgery under general anesthesia with endotracheal intubation, and at the time of extubation developed a type-I POPE associated reduction of cardiac function.
Case Report
This was a 17-year-old woman with height 154 cm, body weight 48 Kg, no previous medical history, and American Statistical Association category I.
Maxillary and mandibular osteoplasties were performed for cleft lip, alveolus, and palate. General anesthesia was rapidly initiated using propofol and remifentanil, followed by the administration of vecuronium. Transnasal intubation was carried out with a nasotracheal tube having an internal diameter of 6.5 mm. Intubation was achieved without complication during first attempt, and anesthesia was maintained during surgery using sevoflurane and remifentanil. During the surgery, no abnormalities associated with breathing or circulatory dynamics were observed, and the operation was completed in 5 h and 40 min. The estimated blood loss was 440 mL, and the total blood transfusion volume was 3030 mL; hence, the intraoperative balance which includes the total urine volume (128 ml) and insensible perspiration (1086 mL approx 4 mL/Kg/h) was plus 1376 mL.
At the completion of the operation, the patient was semi-conscious and was able to follow commands to a limited degree. Spontaneous respirations with associated sufficient tidal volumes were present, so extubation was carried out. However, immediately after extubation, she developed stridor accompanied by seesaw breathing involving marked inspiratory efforts. The patient's lower jaw was raised manually, and her progress was monitored closely, but the hypoxemia gradually worsened, and her level of consciousness waned. Her oxygen saturation decreased from 99% to 70%, even with the supplemental administration of 100% oxygen at 10 L/min using a face-mask.
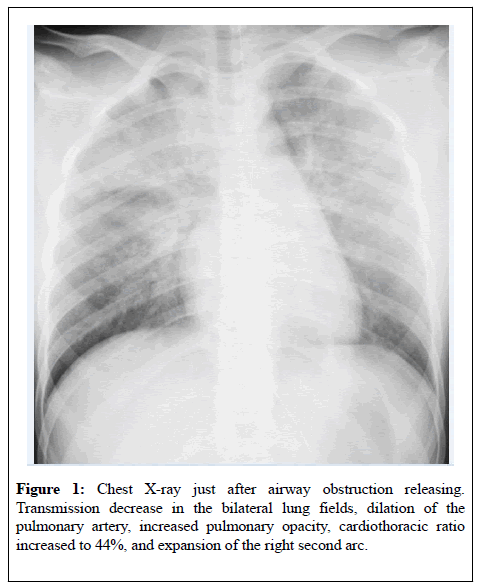
The buccal cavity contained large quantities of blood and saliva, which were removed by suction. At this point, the airway obstruction symptoms were gradually alleviated, and her oxygen saturation returned to 98% after 5 min. Her consciousness level also gradually improved, at which point she complained of breathing difficulties. Her airway was checked using a fiberoptic scope. The bilateral vocal cords were open, and although mild swelling of the arytenoid region was found, the larynx did not appear to have any functional or organic abnormalities. Arterial blood gas results after alleviation of the upper airway obstruction symptoms were low for both PaO2 and PCO2, at 97 and 43 mmHg, respectively, despite having 100% oxygen supplied at 10 L/min by face-mask. The patient continued to complain of shortness of breath, so a chest X-radiography was performed which showed evidence of the following: transmission decrease in the bilateral lung fields, dilation of the pulmonary artery, increased opacity in the pulmonary hilum, cardiothoracic ratio (CTR) increased to 44%, and expansion of the right second arc (Figure 1).Transthoracic echocardiography revealed cardiac dysfunction, involving an expansion of the left ventricular lumen, and a reduction of the left ventricular ejection fraction (LVEF) to 50% or less. No marked changes were found by 12-lead electrocardiography. When diuretics were administered, her symptoms were alleviated somewhat, so the patient was transferred to the general hospital ward approximately 3 h after extubation.
Figure 1: Chest X-ray just after airway obstruction releasing. Transmission decrease in the bilateral lung fields, dilation of the pulmonary artery, increased pulmonary opacity, cardiothoracic ratio increased to 44%, and expansion of the right second arc.
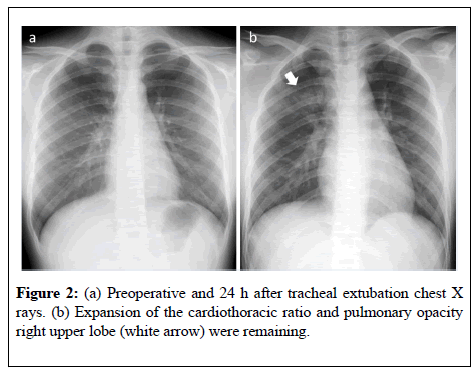
She had no subsequent return of the previous respiratory symptoms and her progress was followed closely. She was managed with oxygen administration alone, and without treatments such as positive endexpiratory pressure (PEEP). The following day, a cardiac ultrasonography exhibited a further reduced LVEF. Chest X-radiography showed a protrusion of the right and left second arcs that had not recovered to preoperative levels, a persistent dilation of the pulmonary arteries, and an unchanged CTR (Figure 2). Cardiac function recovered to the normal state by 3 days after surgery, and the patient was discharged from the hospital 10 days after surgery.
Discussion
Various causes for this patient's upper airway obstruction can be suggested, including insufficient recovery from anesthesia at the time of extubation, reduced gag reflex and cough strength, and an accumulation of blood, phlegm, and saliva in the oropharynx. The simultaneous occurrence of laryngeal spasms stimulated by one or more of these processes cannot be ruled out. The mechanism of development of pulmonary edema in connection with this type of upper airway obstruction begins with an increase in the left ventricular pre-load due to excessive inspiratory efforts. Increased venous perfusion associated with excessive decreases in pulmonary internal pressure, and increased ventricular post-load due to stress causing sympathetic nerve tension, results in increased pulmonary blood flow, pulmonary venous pressure, and capillary hydrostatic pressure, ultimately leading to the development of pulmonary edema. In addition, strong negative pulmonary pressures cause the leakage of fluid from the pulmonary capillaries into the interstitium, resulting in edema.
Pulmonary edema resulting from both of these mechanisms is classed as type-I POPE [4,5].
In the case of the present patient, her inspiratory effort was not great, and stridor began at the time of extubation, which makes her condition consistent with type-I POPE. The pulmonary edema in type-I POPE consists primarily of negative-pressure pulmonary edema, but it also includes hydrostatic pulmonary edema [6]. After elimination of the patient's airway obstruction, chest X-radiography showed an increased CTR, and transthoracic echocardiography showed a reduced LVEF. The patient's progress was followed for more than 12 h after elimination of the airway obstruction. Chest X-radiography the following day indicated that the protrusion of the right and left second arcs had not yet recovered to their preoperative levels, and the pulmonary arterial diameters were still increased. As this patient was a young adult, her intraoperative water balance would have been within the acceptable range, and it is uncertain whether the above changes can be explained solely on the basis of the mechanism of pulmonary edema in type-I POPE. Stress cardiomyopathic symptoms are known to occur after upper airway obstruction [7] but for this patient, the 12-lead electrocardiography showed no changes, so no attempts were made to detect troponin T or other myocardial biomarkers. However, the patient's increased CTR and decreased LVEF suggested such the cardiomyopathy, and it is possible that the level of pulmonary edema was affected. After upper airway obstruction, it is important to consider obtaining myocardial deviant enzyme measurements, electrocardiography, echocardiography, and if necessary, a consultation with a cardiovascular specialist.
The recommended treatment for POPE is airway management, oxygen administration, and the application of PEEP [3]. It can be suggested that for this patient the application of PEEP would have resulted in a more rapid alleviation of POPE, but because of her recent facial osteoplasty, the use of a non-invasive positive pressure ventilation (NPPV) face mask, which would be needed to apply PEEP, could lead to increased postoperative pain, swelling and/or bleeding. Additionally, it would be difficult to drain her sputum and secretions because of the nasal blockage that occurs after a facial osteoplasty. For these reasons, NPPV and PEEP were not good options for this patient. Fortunately, her symptoms were alleviated rapidly by oxygen and diuretic administration, so the administration of positive airway pressure was not required.
Conclusion
General anesthesia for the maxillofacial surgery performed on this young woman, was achieved with endotracheal intubation, and type-I POPE developed at the time of extubation. When continued hypoxemia is observed even after the elimination of an airway obstruction, it is important to evaluate the left-sided cardiac function, at the same time as taking appropriate prophylactic measures with the possibility of POPE in mind.
Acknowledgement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- Udeshi A, Cantie SM, Pierre E. Postobstructive pulmonary edema. J Crit Care. 2010;25(3):538.e1-e5.
- Lemyze M, Mallat J. Understanding negative pressure pulmonary edema. Intensive Care Med. 2014;40(8):1140-3.
- Louis PJ, Fernandes R. Negative pressure pulmonary edema. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(1):4-6.
- Lang SA, Duncan PG, Shephard DA, Ha HC. Pulmonary oedema associated with airway obstruction. Can J Anaesth. 1990;37(2):210-8.
- Guffin TN, Har-el G, Sanders A, et al. Acute Postobstructive Pulmonary Edema. Otolaryngol Head Neck Surg. 1995;112(2):235-7.
- Ringold S, Klein EJ, Del Beccaro MA. Postobstructive pulmonary edema in children. Pediatr Emerg Care. 2004;20(6): 391-5.
- Keshtkar F, Dale OT, Bennett WO, et al. Management of airway obstruction with nebulized adrenaline resulting in takotsubo cardiomyopathy: case report. J Laryngol Otol. 2016;130(9): 883-6.