Presence of a simple lateral extramural diverticulum at the junction of second and third parts of the duodenum – a case report
Bincy M. George*, Satheesha Nayak B, Snigdha Mishra and Sudarshan S
Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), International Centre for Health Sciences, Madhav Nagar, Manipal, Udupi District, Karnataka State, India
- *Corresponding Author:
- Bincy M. George, PhD
Assistant Professor of Anatomy, Melaka Manipal Medical College (Manipal Campus), International Centre for Health Sci. Madhav Nagar, Manipal, Udupi Karnataka State, 576104, India
Tel: +91 (820) 2922519
E-mail: bincyrajakumary@yahoo.com
Date of Received: November 22nd, 2011
Date of Accepted: September 22nd, 2012
Published Online: December 26th, 2012
© Int J Anat Var (IJAV). 2012; 5: 132–133.
[ft_below_content] =>Keywords
duodenum, diverticulum, pot shaped, valveless, lumen
Introduction
Though the exact etiology is not clear, the prevalence of duodenal diverticula increases with age and is found in less than 5% of post-mortem examinations [1]. Progressive weakening of the intestinal smooth muscles and increase in intraduodenal pressure is said to be the reason for this out pouching of the duodenum [2]. Most (70-75%) of duodenal diverticula occur in the periampullary region, within 2-3 cm radius of the ampulla of Vater [3]. Concave medial border of the duodenum is the common site for diverticula [2]. Because of its proximity to the head of the pancreas, fluid filled duodenal diverticula can be misinterpreted as pancreatic psuedocysts [2,3].
Case Report
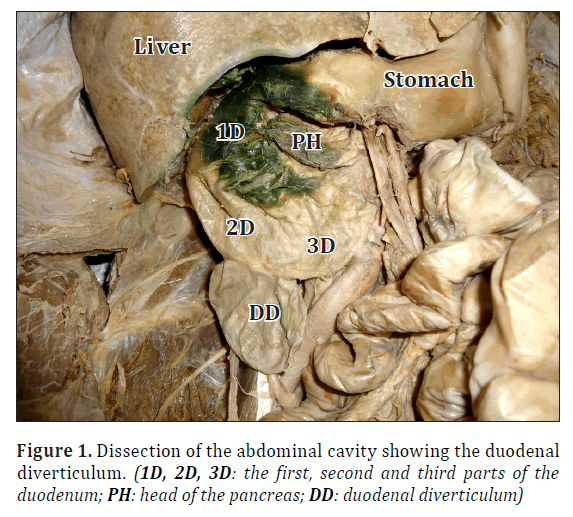
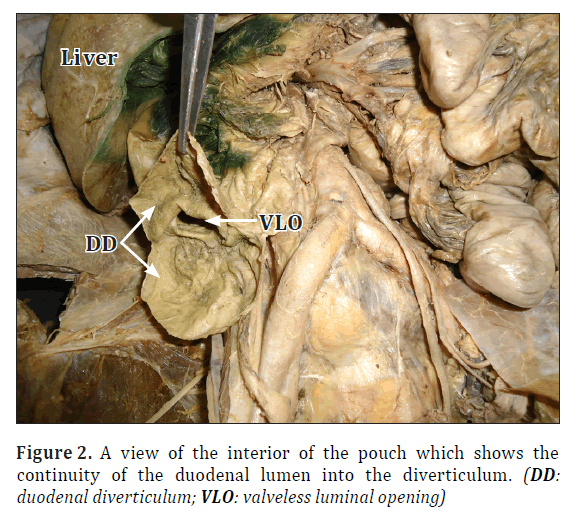
During the routine dissections for the medical undergraduates, a ‘pot shaped’ diverticulum was seen to arise from the lateral border, at the junction of the second and third parts of the duodenum in an approximately 55-year-old male cadaver (Figure 1). The diverticulum was covered by peritoneum and was about 3 cm in length and 2 cm wide at the base. After removing the peritoneal covering, the lateral border of the diverticulum was incised. There was a valveless opening seen, which communicated with the duodenal lumen (Figure 2). Undigested food particles were observed in the lumen of the diverticulum. The subject’s medical history is not known to us.
Discussion
Small bowel diverticula are usually acquired (false diverticula) and multiple in contrast to the Meckel’s diverticulum [4]. Most of the duodenal diverticula are extramural, but the presence of it in the outer border is rare [5,6]. Extramural duodenal diverticula are again classified into two types, (a) peri-ampullary diverticula, which is present adjacent to the ampulla of Vater or it may even contain ampulla of Vater or common bile duct; (b) juxta-periampullary duodenal diverticula, when the diverticula are located within the 2 cm radius of the major duodenal papillae [5]. According to the literature the larger pouches usually lack a muscular coat. The extramural duodenal diverticula are classified into types (a) congenital or true pouches, if the muscular layer is present; (b) acquired or false pouches if muscular layers are absent [5]. The thickness of the wall of the extramural pouch we found had the similar thickness as the second and the third part of the duodenum in the cadaver, suggesting a congenital origin. Previous studies suggest that clinical presentation of the duodenal diverticula is upper abdominal pain, duodenal ulcers, diverticulitis, perforations or symptoms of the delayed emptying of the diverticulum [7]. The knowledge of this kind of duodenal pouch is very important for surgeons, radiologists, gastroenterologist and physicians.
References
- Hayee B, Noor Khan H, Al-Mishlab T, McPartlinJF. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003; 9: 883–884.
- Rizwan MM, Singh H, Chandar V, Zulfiqar M, Singh V. Duodenal diverticulum and associated pancreatitis: Case report with brief review of literature. World J Gastrointest Endosc. 2011; 3: 62–63.
- Hariri A, Siegelman SS, Hruban RH. Duodenal diverticulum mimicking a cystic pancreatic neoplasm. Br J Radiol. 2005; 78: 562–564.
- Lin CH, Hsieh HF, Yu CY, Yu JC, Chan DC, Chen TW, Chen PJ, Liu YC. Diverticulosis of the jejunum with intestinal obstruction: A case report. World J Gastroenterol. 2005; 11: 5416–5417.
- Mahajan SK, Kashyap R, Chandel UK, Mokta J, Minhas SS. Duodenal diverticulum: Review of literature. Indian J Surg. 2004; 66: 140–145.
- Mendelson RM, Shepherd HA, Mitchell A. “Inverted” diverticulum mimicking an ulcerated duodenal tumour. Br J Radiol. 1984; 57: 426–430.
- Graur F, Bala O, Bodea R, Geczi-Toth I, Vlad L, Lancu C. Laparoscopic resection of duodenal diverticulum. A case report. Rom J Gastroenterol. 2005; 14: 405–408.
Bincy M. George*, Satheesha Nayak B, Snigdha Mishra and Sudarshan S
Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), International Centre for Health Sciences, Madhav Nagar, Manipal, Udupi District, Karnataka State, India
- *Corresponding Author:
- Bincy M. George, PhD
Assistant Professor of Anatomy, Melaka Manipal Medical College (Manipal Campus), International Centre for Health Sci. Madhav Nagar, Manipal, Udupi Karnataka State, 576104, India
Tel: +91 (820) 2922519
E-mail: bincyrajakumary@yahoo.com
Date of Received: November 22nd, 2011
Date of Accepted: September 22nd, 2012
Published Online: December 26th, 2012
© Int J Anat Var (IJAV). 2012; 5: 132–133.
Abstract
Extramural duodenal diverticulum along the convex margin of the duodenum is a rare entity. Though its exact etiology is not clear, diverticulum of duodenum usually occurs at weak spots in duodenal walls near the major and minor duodenal papillae. Here we present a case, where we found an unusual diverticulum at the junction of the second and third parts of the duodenum. This was unique as it was very prominent with about 3 cm diameter and was along the lateral convex margin. Gastroenterologist and surgeons who deal with gastrointestinal obstructions or infections should be alert about this particular variation.
-Keywords
duodenum, diverticulum, pot shaped, valveless, lumen
Introduction
Though the exact etiology is not clear, the prevalence of duodenal diverticula increases with age and is found in less than 5% of post-mortem examinations [1]. Progressive weakening of the intestinal smooth muscles and increase in intraduodenal pressure is said to be the reason for this out pouching of the duodenum [2]. Most (70-75%) of duodenal diverticula occur in the periampullary region, within 2-3 cm radius of the ampulla of Vater [3]. Concave medial border of the duodenum is the common site for diverticula [2]. Because of its proximity to the head of the pancreas, fluid filled duodenal diverticula can be misinterpreted as pancreatic psuedocysts [2,3].
Case Report
During the routine dissections for the medical undergraduates, a ‘pot shaped’ diverticulum was seen to arise from the lateral border, at the junction of the second and third parts of the duodenum in an approximately 55-year-old male cadaver (Figure 1). The diverticulum was covered by peritoneum and was about 3 cm in length and 2 cm wide at the base. After removing the peritoneal covering, the lateral border of the diverticulum was incised. There was a valveless opening seen, which communicated with the duodenal lumen (Figure 2). Undigested food particles were observed in the lumen of the diverticulum. The subject’s medical history is not known to us.
Discussion
Small bowel diverticula are usually acquired (false diverticula) and multiple in contrast to the Meckel’s diverticulum [4]. Most of the duodenal diverticula are extramural, but the presence of it in the outer border is rare [5,6]. Extramural duodenal diverticula are again classified into two types, (a) peri-ampullary diverticula, which is present adjacent to the ampulla of Vater or it may even contain ampulla of Vater or common bile duct; (b) juxta-periampullary duodenal diverticula, when the diverticula are located within the 2 cm radius of the major duodenal papillae [5]. According to the literature the larger pouches usually lack a muscular coat. The extramural duodenal diverticula are classified into types (a) congenital or true pouches, if the muscular layer is present; (b) acquired or false pouches if muscular layers are absent [5]. The thickness of the wall of the extramural pouch we found had the similar thickness as the second and the third part of the duodenum in the cadaver, suggesting a congenital origin. Previous studies suggest that clinical presentation of the duodenal diverticula is upper abdominal pain, duodenal ulcers, diverticulitis, perforations or symptoms of the delayed emptying of the diverticulum [7]. The knowledge of this kind of duodenal pouch is very important for surgeons, radiologists, gastroenterologist and physicians.
References
- Hayee B, Noor Khan H, Al-Mishlab T, McPartlinJF. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003; 9: 883–884.
- Rizwan MM, Singh H, Chandar V, Zulfiqar M, Singh V. Duodenal diverticulum and associated pancreatitis: Case report with brief review of literature. World J Gastrointest Endosc. 2011; 3: 62–63.
- Hariri A, Siegelman SS, Hruban RH. Duodenal diverticulum mimicking a cystic pancreatic neoplasm. Br J Radiol. 2005; 78: 562–564.
- Lin CH, Hsieh HF, Yu CY, Yu JC, Chan DC, Chen TW, Chen PJ, Liu YC. Diverticulosis of the jejunum with intestinal obstruction: A case report. World J Gastroenterol. 2005; 11: 5416–5417.
- Mahajan SK, Kashyap R, Chandel UK, Mokta J, Minhas SS. Duodenal diverticulum: Review of literature. Indian J Surg. 2004; 66: 140–145.
- Mendelson RM, Shepherd HA, Mitchell A. “Inverted” diverticulum mimicking an ulcerated duodenal tumour. Br J Radiol. 1984; 57: 426–430.
- Graur F, Bala O, Bodea R, Geczi-Toth I, Vlad L, Lancu C. Laparoscopic resection of duodenal diverticulum. A case report. Rom J Gastroenterol. 2005; 14: 405–408.