Primary Breast Tuberculosis
2 Professor of Obstetrics and Gynaecology, Head of the Department, Souissi Maternity Hospital, Rabat, Samu CHU Ibn Sina, Hospital in Rabat, Morocco
Received: 13-Jan-2020 Accepted Date: Jan 24, 2020; Published: 03-Feb-2020
Citation: Sarah T, Slaouoi A, Benzina I, et al. Primary Breast Tuberculosis. Surg Case Rep. 2020;5(1):5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Tuberculous mastitis is a rare condition, even in endemic countries. Clinical and radiological examination are not specific, posing the problem of differential diagnosis with neoplastic pathology; this requires the use of cytological and/or biopsy studies for a diagnosis of certainty.
We report one case of breast tuberculosis. The diagnosis was put on histology with good outcome under anti bacillary treatment. Through the literature data we will focus on the epidemiological, clinical, radiological and therapeutic characteristics of this pathology. We will also insist on the difficulties of the differential diagnosis with other mastopathies, especially with breast cancer so as not to engage in mutilating investigations.
http://www.environmentjournals.com/
http://www.eventsupporting.org/
http://www.escientificreviews.com/
http://www.openaccesspublications.com/
http://www.imedpub.org/
http://www.jpeerreview.com/
http://www.escientificres.com/
http://www.scholarlyjournals.org/
http://www.eclinicaljournals.com/
http://www.scischolarsjournal.com/
http://www.intlscholarsjournal.com/
http://www.scholarsresjournal.com/
http://www.sysrevpharma.org/
http://www.environjournal.com/
http://www.jpeerres.com/
http://www.managjournal.org/
http://www.emedicalhub.org/
http://www.biomedresj.org/
http://www.aaccongress.com/
http://www.eclinicalres.org/
http://www.scholarlymed.com/
http://www.eclinicalres.com/
http://www.theresearchpub.com/
http://www.imedpubscholars.com/
http://www.scholarcentral.org/
http://www.journalpublications.org/
http://www.scholarlypub.com/
http://www.imedpublishing.org/
http://www.emedsci.com/
http://www.longdomjournals.org/
http://www.longdomjournal.org/
http://www.emedicalcentral.com/
http://www.lexisjournal.com/
http://www.geneticjournals.com/
http://www.scitecjournals.com/
http://www.microbialjournals.org/
http://www.engjournals.org/
http://www.eneurologyjournals.com/
http://www.pulsusjournal.org/
http://www.biochemjournal.org/
http://www.epharmacentral.com/
http://www.eclinicalsci.com/
http://www.eclinicalcentral.com/
http://www.eclinmed.com/
http://www.jopenaccess.org/
http://www.peerreviewedjournals.com/
http://www.immunologyjournals.com/
http://www.neurologyjournals.org/
http://www.clinicalmedicaljournals.com/
http://www.molecularbiologyjournals.com/
http://www.geneticsjournals.com/
http://www.biochemistryjournals.org/
http://www.psychiatryjournals.org/
http://www.pharmajournals.org/
http://www.alliedresearch.org/
http://www.medicalres.org/
http://www.medicalresjournals.com/
http://www.alliedsciences.org/
http://www.pediatricsjournals.org/
http://www.oncologyinsights.org/
Keywords
Tuberculous mastitis (TM); Breast; Tuberculosis (TB); Caseous necrosis
Introduction
Tuberculosis is an infectious disease usually caused by Mycobacterium tuberculosis bacteria. It has historically been associated with poverty and low socioeconomic status [1]. In Morocco, TB continues to pose a major public health problem, because of its frequency and gravity; despite the existence of national programs of Tuberculosis Control for several years [2]. Some localizations of TB disease are rare or even exceptional. Breast tuberculosis is certainly the last of all visceral locations [3-5]. However, it must be distinguished from other breast pathologies especially breast carcinoma, given the clinical and mammographic similarities. We will review the current knowledge of this rare manifestation of a common disease.
Case Report
A 56-years-old female patient, mother of 5 children, with a history of lactation, without pathological antecedents. Addressed to our department for managing a suspicion of a locally advanced breast cancer.
She presented with a lump in her right breast, which was growing slowly since the past thirty days. Initial painless lump had now become painful with induration of skin and appearance of three cutaneous fistulas two days prior to admission. She denied fever, night sweats, weight loss, or respiratory symptoms.
Physical examination showed that the right breast was enlarged in size, presenting necrotic erythemato-squamous patches, infiltrated, pruriginous and slightly purplish, centered by a blackish zone frankly necrotic. There was a 4 cm × 3 cm lump in the upper-outer quadrant with no adenopathy. There were no clinical manifestations of the disease to the nipple-areolar area, or signs of nipple discharge. No swellings were found in the opposite breast and axilla.
The patient was afebrile, with normal blood pressure. Laboratory workup revealed hypochromic microcytic anemia (Ht 33%, Hb 11 g/dl), lymphocytic white blood cell type, normal liver and kidney function, C-reactive protein (CRP < 10 mg/L).
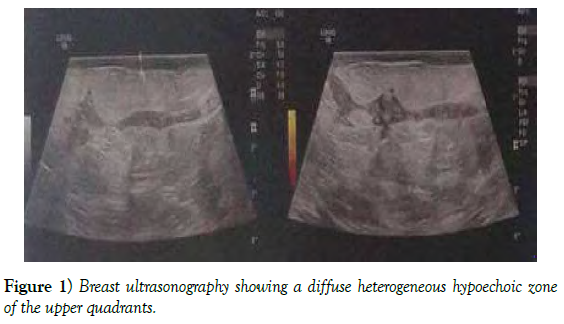
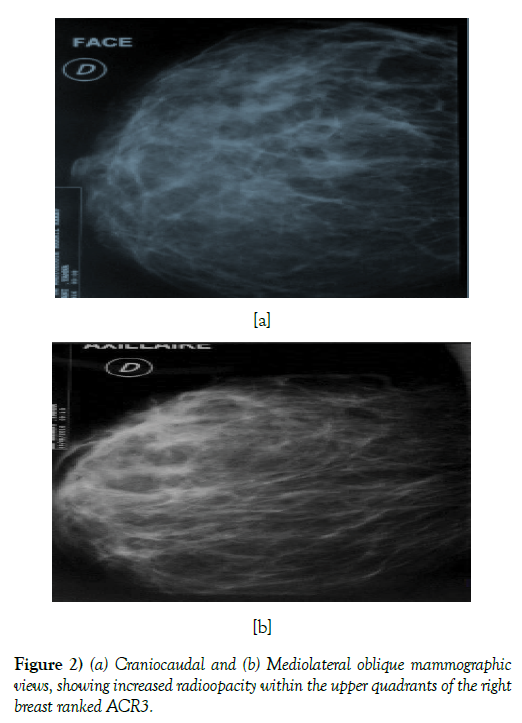
Mammography and ultrasound complement revealed the presence of a heterogeneous hypoechoic zone, fistilused at the skin and associated with diffuse skin thickening; it was rated ACR 3.
Histological analysis of biopsy at fistula pathway showed the presence of epithelio-gigan to-cellular granuloma with caseaous necrosis.
The chest X-ray is without abnormalities. The patient received anti bacillary treatment according to the national tuberculosis control program during 6 months, and was well tolerated. The evolution was marked by clinical and ultrasound improvement with a follow-up of 12 months (Figures 1 and 2).
Discussion
TB of the mammary gland is a rare disorder often mistaken for other benign and malignant lesions of the breast. The first case of mammary tuberculosis was recorded by Sir Astley Cooper in 1829 who called it “scrofulous swelling of the bosom” [4].
Breast tuberculosis is a particularly rare pathology; its frequency is estimated between 0.025% to 4.5% of all tumoral conditions; since the glandular tissue, such as spleen and skeletal muscle, offer resistance to the survival and multiplication of tubercle bacilli [5,6].
It comes in the last row of tuberculous extra-pulmonary sites, and represents 0, 06% of these [6]. Breast tuberculosis is found in countries with high tubercular endemicity. For KHAIZ, out of a study of 215 cases, Asia leads with 45.2%, followed by Black Africa 27.4%, North Africa 17.2%, Europe 16.2% and finally America 4% [7,8].
In Morocco, tuberculosis is a public health problem. 26,000 to 27,000 new cases of all forms of tuberculosis are detected annually in recent years. The cumulative incidence of all forms of tuberculosis was always greater than 100 cases per 100,000 inhabitants. It is only from year 2000 that this incidence is less than 100 cases per 100 000 inhabitants. Currently, it averages 82 new cases per 100,000 inhabitants. And mammary localization remains among the very rare localizations of extra-pulmonary tuberculosis [9].
It mainly affects young women of childbearing age [10]. It is rare before puberty and after menopause. This is explained by the physiological activity of the breast [11].
TB mastitis appears to be favored by a number of factors, like:
• Multiparity: Breast tuberculosis is more common in multiparous women [12].
• Pregnancy and breastfeeding: remain the most important factors, since the vascularization of the mammary gland is very rich during this period which explains its susceptibility to tuberculosis [13].
• During lactation, the mammary ducts are ectasized encouraging canalicular contamination [14].
• Immunosuppression: Breast tuberculosis may be revealing of an HIV infection so far unknown [15].
Before, it was thought that mammary tuberculosis was secondary to pleuropulmonary involvement in more than 50%.
Currently, it is considered that tuberculous mastitis is usually a primitive and isolated disease, or on the contrary, associated with other bacillary manifestations, especially ganglionic, pulmonary, osteoarticular or genitourinary.
Routes of contamination are diverse:
• The lymphatic way: it is the most common route of contamination. The extension is carried out by retrograde or anterograde way from intra-thoracic, cervical, supraclavicular or axillary lymphadenopathy [16].
• The hematogenous pathway: in the context of a miliary tuberculosis [17].
• Extension by contiguity from a neighborhood focus, such as costal lesion (tuberculous osteitis), the shoulder joint (tuberculous arthritis), the pleural space (tuberculous pleurisy) [18].
• Exceptionally, transcutaneous penetration of the bacillus of Koch: Penetration through a cutaneous abrasion [19].
• Penetration from the nipple by the milk ducts: expanded ducts during pregnancy and lactation are particularly susceptible to tuberculous infection [3].
Classically, there are two types of breast tuberculosis: Secondary with involvement of other organs and Primary where it is strictly localized in the breast, which is the most common.
Our patient had Primary breast tuberculosis [20]. The diagnosis is always difficult because breast tuberculosis can simulate a large number of conditions, especially in elderly women where breast cancer remains the key concern; and also because of the lack of specificity of its clinical and radiological signs. Only histological evidence can guarantee a definite diagnosis [21].
However, some clinical criteria seem useful to draw attention to a tuberculous etiology, like the existence of a recurrent abscess rebellious to antibiotics, and the existence of fistulized axillary lymphadenopathy and mammary fistula with nipple discharge [22]. Radiologically, there are no specific mammographic signs of mammary tuberculosis [23].
Mammography may show irregular heterogeneous opacities, poorly limited, sometimes with calcifications, pointing towards a malignant etiology.
Breast ultrasound is an essential supplement to mammography; it allows the exploration of inaccessible lesions and to complete mammography data, both in terms of density and location. It is indicated for lactating women, pregnant women and those with dense breasts. In case of mammary tuberculosis, it shows heterogeneity suggestive of mastitis. The most common aspect is that of a hypoechoic, heterogeneous, poorly limited image with minimal posterior reinforcement [24].
The diagnosis of certainty is through histological examination with the detection of epitheloid cell granulomas with Langhans’ giant cells and caseous necrosis [25]. The main differential diagnosis to be feared in breast tuberculosis is breast cancer; other pathologies are to be discussed, such as breast abscess, fibroadenoma, sarcoidosis and granulomatous mastitis.
In our case, in front of an inflammatory breast in an elderly and menopausal woman, the first diagnosis to be evoked is breast cancer; and only the histological examination allowed the diagnosis of mammary tuberculosis.
Due to the rarity of TM, there are no established guidelines for management. In combination with anti-tuberculosis drugs, local excision, aspiration, drainage of cold abscess, mastectomy (for a severely destroyed breast or due to lack of response to anti- tuberculosis drugs), or no surgery at all, have all been reported to be successful [22].
Success rate of medical therapy approaches 95% in most series with 6 months of antituberculous therapy (2 months of Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol/4 months of Isoniazid and Rifampicin) [26,27]. Some authors prefer the 9-month regimen (2 months of Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol/7 months of Isoniazid and Rifampicin) due to lower relapse rate in general.
Conclusion
Breast tuberculosis is rare even in endemic countries. However, it deserves to be known because of its extreme similarities with breast cancer. It occurs mainly in young women during periods of genital activity. Indeed, it is favored by multiparity, pregnancy, breastfeeding and immunodepression including HIV infection. The clinical and radiological pictures are misleading, and pose a diagnostic problem especially with breast cancer; Hence the need for bacteriological and pathological investigations to guarantee diagnosis of certainty. The disease is curable with antitubercular drugs; and surgery is rarely required.
REFERENCES
- Ben Hassouna J. Gynécologie obstétrique et fertilité. 2005; 870-876.
- Direction d’épidémiologie et la lutte contre les maladies; service des maladies respiratoires, Maroc. 2009.
- Zhiri MA, Hamdouch A, Benyahia SE. Formes anatomo-cliniques de la tuberculose mammaire. Gynécologie. 1987; 38:356-359.
- Cooper A Illustrations of the diseases of the breast. Part I. London: Longman, Rees, Orme, Brown and Green. 1829; 73.
- Agoda-Zouhal A, Outifa A, Filali A, et al. Les tumeurs pseudonéoplasiques du sein: Tuberculose Mammaire à propos de 2 cas. Médecine du Maghreb. 2000 N°82(11).
- Koussela LK, Djibril AM, Adjessou KV. Tuberculose mammaire: A propos d’un cas. J Afr Imag Méd. 2014; 6(3):73-77.
- Zandrino F, Monetti F, Gandolfo N. Primary tuberculosis of the breast. A case report. Acta Radiol. 2000; 41:61-63.
- Khaiz D, Lakhloufi A, Chehab F, et al. Tuberculose mammaire. À propos de deux cas, Sem. Hop. 1993; 69:454- 458.
- WHO. Programme national de lutte antituberculeuse; Guide de la lutte antituberculeuse. 2011.
- Pricop F, Pricop M, Dumitrache F, et al. La tuberculose mammaire: A propos de deux case. Rev. Fr Gynécol. Obstét. 1996; 91:381-382.
- Hale JA, Peters GN, Cheek JH. Tuberculosis of the breast: rare but still existent review of the literature and report of an additional case, Am. J. Surg. 1985; 150:620-624.
- Kakkar S, Kapila K, Singh MK, et al. Tuberculosis of the breast a cytomorphologic study. Acta Cytol. 2000; 44:292-6.
- Goldman KR. Tuberculosis of the breast. Tubercle. 1978; 59:41-45.
- Pricop F, Pricop M, Dumitrache F, et al. La tuberculose mammaire: à propos de deux cas. Rev. Fr Gynécol. Obstét. 1996; 91:381-382.
- Hartstein M, Leaf HL. Tuberculosis of the breast as a presenting manifestation of AIDS Clin Infect Dis. 1992; 15:692-693.
- Leleu O, Aubry P. Tuberculose mammaire, Rev. Mal. Respir. 1997; 14:401-403.
- Ei MA, Moumen M, Louahlia S. Tuberculose mammaire : à propos de trois cas, Sem. Hop. Paris. 1993; 69:1277-1279.
- Pieron R, Gessain A, Grivaux M. Un cas de tuberculose mammaire chez une africaine, Sem. Hop. Paris. 1985; 61: 2373- 2376.
- Hamit HF, Ragsdale TH. Mammary tuberculosis Jr Soc Méd. 1988; 75:764-765.
- Marinopoulos S, Lourantou D, Gatzionis T, et al. Breast tuberculosis: Diagnosis, management and treatment. Int J Surg Case Rep. 2012; 3(11):548-550.
- Gulpinar K, Ozis SE, Ozdemir S, et al. Primary breast tuberculosis: Report of a case. Surgical Science. 2013; 4:68–71.
- Hawilo A, Abdelmalek R, Mebazaa A, et al. Tuberculosis of the breast: a rare often unrecognized diagnosis, Med Sante Trop 2012; 22(3):292- 296.
- Morsad F, Ghazli M, Boumzgou K, et al. El Kerroumi et al. Tuberculose mammaire: A propos de 14 cas. J Gynecol Obstet Biol Reprod. 2000; 30(4):331–333.
- Filippou DC, Rizos S, Nissiotis A. Primary breast tuberculosis: a case report. Radiology and Oncology. 2003; 37.
- Mirsaeidi SM, Masjedi MR, Mansouri SD, et al. Tuberculosis of the breast: report of 4 clinical cases and literature review. East Mediterr Health J. 2007; 13(3):670-676.
- Jalali U, Rasul S, Khan A, et al. Tuberculous mastitis. J Coll Physicians Surg Pak. 2005; 15(4):234-237.
- Shinde SR, Chandawarkar RY, Deshmukh SP. Tuberculosis of the breast masquerading as carcinoma: A study of 100 patients. World J Surg. 1995; 19(3):379-381.