Primary hyperaldosteronism: A very rare etiology of coronary artery ectasia
2 Laboratory of Epidemiology, Clinical Research and Public Health, Faculty of Medicine and Pharmacy, Mohammed the First University of Oujda, Morocco, Email: n.elouafi@ump.ac.ma
Received: 07-Feb-2021 Accepted Date: Mar 11, 2021; Published: 18-Mar-2021
Citation: Rasras H, Kacimi A, El-Ouafi N, et al. Primary hyperaldosteronism: very rare etiology of coronary artery ectasia. Clin Cardiol J. 2021;5(2):8-9.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Primary hyperaldosteronism as a cause of coronary artery ectasia has only been reported one time in the literature, and here we report the second presentation of this very rare association.
Case Summary: A 67-year-old man, with a history of treatment-resistant hypertension, was admitted to intensive care unit of cardiology for N-STEMI. His coronary angiography revealed an ectasia of all three major coronary arteries without significant luminal obstruction (TIMI III); and he was put on Dual antiplatelet therapy. Etiological assessment found an Idiopathic primary hyperaldosteronism, and our patient is actually on spironolactone with good blood pressure controls.
Conclusion: Early treatment of primary hyperaldosteronism and a good therapeutic approach for coronary ectasia are important to prevent any lifethreatening complications.
Keywords
Coronary artery ectasia; Primary hyperaldosteronism, Aneurysm, Acute coronary syndrome; Case report
Abbreviations
CAE: Coronary Artery Ectasia; PH: Primary Hyperaldosteronism; ACS: Acute Coronary Syndrome; TTE: Transthoracic Echocardiogram; LAD: Left Anterior Descending; ACAD: Aneurysmal Coronary Artery Disease; CAA: Coronary Artery Aneurysms; PCI: Percutaneous Coronary Intervention; PTFE: Polytetrafluoroethylene; MI: Myocardial Infarction.
Introduction
Coronary artery ectasia (CAE) is defined as a diffuse dilation of coronary artery with a diameter 1.5 times greater than a normal adjacent artery, with a prevalence of 1% – 5%, that dominates in male population (ratio of 4:1) [1]. Atherosclerosis is the most common etiology, while primary hyperaldosteronism (PH) is rarely mentioned. Coronary angiography remains the gold standard for its diagnosis [2]. Therapeutic strategies involve medical with percutaneous or surgical revascularization if necessary and treatment of PH. The prognosis of CAE depends directly on the severity of the concomitant coronary artery disease [2] via an exceptional case of PH discovered during an etiological assessment of CAE in the context of an acute coronary syndrome (ACS) and after a literature review; we aim to explain its possible pathogenesis, clinical presentation, therapeutic management and prognosis.
Clinical Presentation
Patient information
A 67-year-old man, with a past history of treatment-resistant hypertension, was admitted for N-STEMI.
Physical exam
Blood pressure was 195/95 mmHg in both arms. Respiratory, neurological and abdominal examinations were without abnormalities.
Diagnostic assessment
Biological analysis showed an elevated rate of troponin-US (1st: 266 ng/ ml, 2nd: 1650 ng/ml) and hypokalaemia (2.8 mmol/L). A transthoracic echocardiogram (TTE) showed a left ventricle hypertrophy, hypokinesia of the inferior, inferoseptal and lateral wall, with a moderate LV systolic dysfunction (EF at 46%) and alteration of global strain at -10%.
Interventions
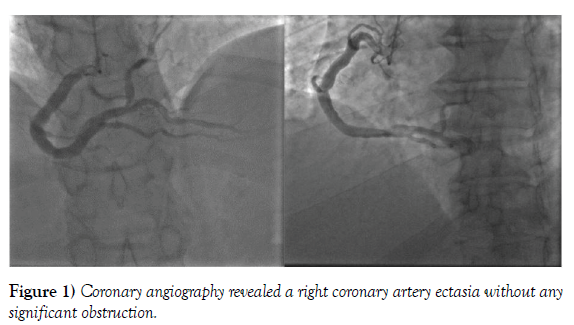
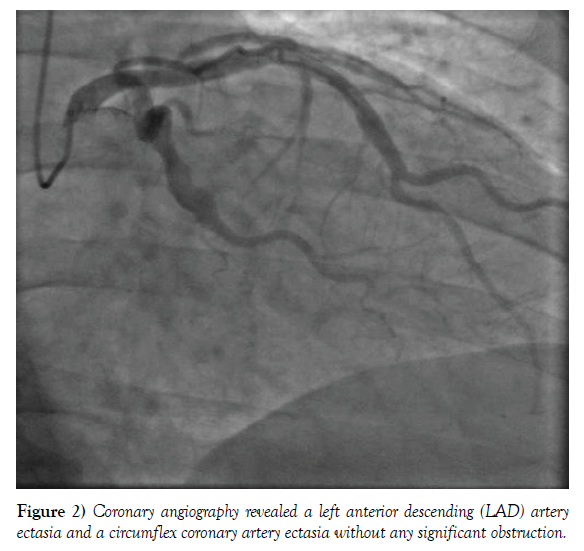
Coronary angiography revealed an ectasia of all three major coronary arteries without significant luminal obstruction, with TIMI flow at III. (Figures 1 and 2). The patient had received a Dual antiplatelet therapy (Aspirin and Clopidogrel), then was evaluated for secondary causes of hypertension (PH was suspected because of treatment-resistant hypertension and persistent hypokalaemia). Plasma aldosterone was 1,080.3 pmol/L; plasma renin activity was 6 mUI/L, with a high ratio of Aldosterone/Renin that was respectively in lying and standing position (103, 96). An abdominal CT scan had showed no masses on adrenal glands. After that, Idiopathic PH was considered as the behind etiology of CAE, and our patient is actually on spironolactone.
Figure 1: Coronary angiography revealed a right coronary artery ectasia without any significant obstruction.
Figure 2: Coronary angiography revealed a left anterior descending (LAD) artery ectasia and a circumflex coronary artery ectasia without any significant obstruction.
Follow-up and Outcomes
The patient has good blood pressure controls, without recidive of pectoris angina.
Discussion
Aneurysmal coronary artery disease (ACAD) includes both coronary artery aneurysms (CAA) and coronary artery ectasia (CAE) [3]. CAA is defined as a localized irreversible dilatation of coronary arterial segment, at least 1.5 times of an adjacent normal coronary artery, while that CAE signifies a diffuse dilatation of more than 50% of coronary artery [1]. The incidence of CAE varies from study to another and that perhaps because of the absence of a uniform definition of CAE, but with the widespread use of coronary CT, magnetic resonance and coronary angiography, the rate of recognition may increase [4].
Atherosclerosis is the most common cause of CAE with an incidence of 50%, especially in western countries, while that Kawasaki disease is more frequent in the Far East; about 17% of cases of CAE are congenital in which coronary artery stenosis frequently exists. 10-20% of them are associated with inflammatory or connective tissue disease. Other etiologies, as hereditary collagen defects, percutaneous coronary intervention (PCI) and PH are rarely mentioned [1].
PH as a behind cause of CAE was described for the first time in 1999 by Arshad et al., it was a triple association of PH, CAE and aortic dissection [5]. And in returning to the literature, we are reporting the second presentation of this rare association.
Hypothetical mechanisms explaining the impact of PH on cardiovascular structures can be summarized in few mechanisms; inappropriate volume retention, endothelial dysfunction, inflammation and fibrosis in these organs. By detailing, chronic excess of aldosterone is capable to affect the normal immune response by activating pro-inflammatory mediators that induces an exaggerated expansive remodelling, which caused by an enzymatic degradation of the extracellular matrix, then thinning of the vessel media [6]. CAE is also related to apical hypertrophic cardiomyopathy with high wall tension. [2]
Ectatic segment with its slow flow phenomenon is an appropriate environment anatomically and biologically for thrombi’s formation with a high risk of vasospasm, immigration of embolisms or more severely wall rupture, especially if it is aneurysmal [7], and that may be asymptomatic or appears by unstable angina or ACS.
Coronary angiography remains the “gold standard” for diagnosis and evaluation of CAE. Further, it has a very important role in the description of lesions by detailing its size, location, the presence or not of stenosis or thrombus and its degree if it exists [2].
CAE treatment includes two parts; the first is etiological – Treatment of PH – by surgical eradication or medical therapy depending on the case [8], in our study, the patient has an idiopathic PH and follows a medical therapy based of anti-aldosterone. The other is the treatment of CAE itself and that consists a medical part and an interventional or surgical part. However, the adequate treatment still always controversial because of the rarity of CAE, it depends on the coexistence or not of CAD. The objective of treatment is to prevent myocardial ischemia and to minimize the risk of thrombosis due to the inflammation and slow flow.
Medical treatment is based on the introduction of antiplatelet agents and anticoagulants depending on intra-coronary flow [3]; statins always have their place in the presence of atheroma and in combination with corticosteroids may be beneficial in inhibiting the cytokines. Trimetazidine has a beneficial effect in ameliorating the coronary flow by multiplying adenosine levels. On the other hand, nitroglycerin and nitrate derivatives have a deleterious effect because of their impact in coronary dilatation, which is already dilated, and consequently; angina pectoris, so they have to be prevented [9].
ACS associated with CAE may require thrombolysis, heparin, and primary PCI with thrombus aspiration. If angina persists despite maximal medical therapy, PCI with polytetrafluoroethylene (PTFE)-covered stents may be indicated, it has currently an important place due to its ability in limiting the development of coronary dilation [10].
Surgical revascularization by ligation of the proximal and distal segment of ectatic segment then replacing it with a bypass graft is rarely indicated, especially in patients with recurring complications [2].
Prognosis of CAE remains often controversial, it could be immediately correlated to the severity of concomitant obstructive coronary artery disease, but it depends essentially on the behind etiology. CAE has an increased risk of myocardial infarction (MI) due to vasospasm, slow flow and thrombosis, especially in extended segments [2]. However, CASS register had not showed a difference in survival patients with or without CAE [6].
Conclusion
CAE is a rare discovery, but with the development of non-invasive imaging techniques, these lesions will be more frequently confronted. Atherosclerosis seems to be the most common cause in adults and Kawasaki disease in children. The presentation of PH as a behind agent of CAE is exceptional. CAE may cause recurrent ACS with an obstructive or non-obstructive lesion. The treatment is medical, interventional or surgical, depending on clinical and radiological situations.
Conflict of Interest
The authors declare that they have no conflict of interest.
REFERENCES
- Kobrossi S, Costantini O, Ahmad U. Coronary artery ectasia presenting as a STEMI. J Am Col Cardiol. 2020;75::3211-3.
- Mansoor A, Sudhir M. Coronary Ectasia. University of Illinois Peoria. 2020 Sep, 18.
- El-Guindy MS, El-Guindy AM. Aneurysmal coronary artery disease: An overview. Global Cardiol Sci Pract. 2017;2017(3).
- Díaz-Zamudio M, Bacilio-Pérez U, Herrera-Zarza M, et al. Coronary artery aneurysms and ectasia: Role of coronary CT angiography. Radiographics 2009;29(7):1939-54.
- Safi AM, Kwan T, Afflu E, et al. Coronary artery aneurysms, aortic dissection, and hypertension secondary to primary aldosteronism: A rare triad: A case report. Angiology. 1999;50(6):503-8.
- Devabhaktuni S, Mercedes A, Diep J, Ahsan C. Coronary artery ectasia-A review of current literature. Current Cardiol Rev. 2016;12(4):318-23.
- Kühl M, Varma C. A case of acute coronary thrombosis in diffuse coronary artery ectasia. J Invas Cardiol. 2008;20(1):23-5.
- Lin TP, Chiu AW, Chen M, et al. Adrenal computed tomography and NP-59 usefulness for diagnosing aldosterone-producing adenomas and idiopathic hyperaldosteronism in primary hyperaldosteronism. Urol Sci. 2016;27(4):269-73.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Journal of the American College of Cardiology. 2011;58(24):44-122.
- Cohen P, O'Gara PT. Coronary artery aneurysms: A review of the natural history, pathophysiology, and management. Cardiology in review. 2008;16(6):301-4.