Pseudo-tumoral gluteal mass of tuberculous origin: A report of a case and its literature review
2 Urology B Department, University Hospital Center Ibn Sina, University Mohammed V, Rabat, Morocco
3 General and Visceral Surgery Department, University Hospital Ibn Sina, Faculty of Medicine and Pharmacy, University Mohammed V, Rabat, Morocco
Received: 02-Dec-2019 Accepted Date: Jan 06, 2020; Published: 13-Jan-2020
Citation: Slaoui A, Slaoui A, Regragui S, et al. Pseudo-tumoral gluteal mass of tuberculous origin: A report of a case and its literature review. Surg Case Rep. 2020;6(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Tuberculosis has existed for millennia and remains a major global health problem. Soft tissue tuberculosis is one of the rare forms of extrapulmonary tuberculosis, and isolated muscular localization is uncommon.
Case Presentation: We report the extremely rare case of a 56-year-old patient without any medical history who presented a pseudo-tumoral gluteal mass of tuberculous origin without other localizations of the disease. He underwent a one-piece excision of the mass measuring 18 cm. Histopathological examination was in favor of a remodeled tuberculoma and the diagnosis was confirmed with polymerase chain reaction (PCR) examination and the positive result of the quantiferon test. The patient completed his antituberculous therapy successfully and the 3-year follow-up revealed no recurrence or complications.
Conclusion: Although isolated muscle tuberculosis is a rare entity, it must always be taken into consideration as a differential diagnosis for isolated muscle swelling, especially in a country with a high TB endemic. The diagnosis is mainly bacteriological and/or pathological. Treatment uses anti-bacillary chemotherapy alone or in combination with surgery. The prognosis is often favorable when the management is early.
Keywords
Gluteal mass; Pseudotumoral; Soft tissue tuberculosis; Isolated extrapulmonary tuberculosis.
Abbreviations
TB: Tuberculosis; HIV: Human Immunodeficiency Virus; AIDS: Acquired Immunodeficiency Syndrome
Introduction
Tuberculosis has existed for millennia and remains a major global health problem. In 2016, 6.3 million new cases of TB were reported equivalent to 61% of the estimated incidence of 10.4 million and extrapulmonary TB represented 15% [1]. Soft tissue tuberculosis is one of the rare forms of extrapulmonary tuberculosis, and isolated muscular localization is uncommon [2].
Case Presentation
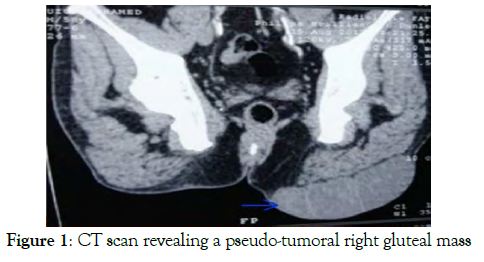
We hereby report the rare case of a 56-year-old man without any medical history, who was referred to our structure for the evaluation of a gluteal mass that progressively increased in size over a three-year period in a context of apyrexia and conservation of general state. The interrogation didn’t reveal any past history of contact with a chronically coughing individual suspected or treated for TB. Clinical examination revealed a painless left buttock mass of 25 cm long axis, well-defined, with a soft consistency and regular outlines, without any sign of inflammation or fistulization. Abdomino-pelvic Computerized tomography demonstrated a multilobed and well-limited subcutaneous lesion process in front of the left gluteal muscles with which it maintains a separation boundary (Figure 1). This gluteal mass measured 64 mm by 162 mm and has only slightly increased after the injection of iodinated contrast medium. In addition, peripheral calcifications were observed.
Biopsy was contraindicated because of the risk of dissemination in view of the high probability of the tumor origin of this well-limited mass with some calcifications. Therefore it was decided to surgically explore it by making an incision opposite the mass. A multi-lobed mass of 18 cm of major axis was found, containing caseous liquid, which was excised in monobloc. We then proceeded to the refection of the gluteal region with excision of the excess skin. The operative time was 168 minutes. Blood loss was minimal. Histopathological examination was in favor of a remodeled tuberculoma with extensive, homogeneous, eosinophilic and acellular caseous necrosis,that was bordered on the periphery by an inflammatory crown, made of epitheloid granuloma with giant cells. The diagnosis was confirmed with polymerase chain reaction (PCR) examination and the positive result of the quantiferon test. The search for concomitant pulmonary TB infection with chest x-ray and bacteriological examination of sputum was not successful. Aoui after an uneventful postoperative recovery, the patient was treated with quadruple antituberculous therapy: rifampicin, isoniazid, ethambutol and pyrazinamide for 2 months, relayed by a combination of rifampicin and isoniazid for 6 months. The patient completed his treatment successfully and the 3-year follow-up revealed no recurrence or complications.
Discussion
Tuberculosis is the ninth leading cause of death globally and the leading cause of death from an agent infectious disease, in front of HIV/AIDS [1]. It is a multisystemic disease with a myriad of presentations and manifestations; it can affect any organ or tissue, excluding only hair and nails [3]. Therefore, diagnosis is very difficult due to the atypical location and non-specific symptoms. Lymph node and pleural localizations are the most common sites of extrapulmonary tuberculosis followed by musculoskeletal and genitourinary forms [4]. Gluteal involvement is rare and the pseudotumoral form of soft tissue tuberculosis of the gluteal muscles is uncommon.
Extrapulmonary TB usually results from the reactivation of primary foci and secondary haematogenous spread. In the musculoskeletal system, organisms are ingested by mononuclear cells that melt into epithelioid cells. A tubercle is formed when the lymphocytes form a ring around a group of epithelioid cells. Caseation occurs in the center of the tuber [5]. Muscular involvement usually takes the form of a painless cystic mass, with inflammatory signs, producing a cold or firm abscess, but sometimes it can take the shape of a mobile tissue mass giving it its pseudotumoral character [6]. The pathophysiology of this location is unclear. The high concentration of lactic acid, as well as the abundant blood supply and the absence of reticuloendothelial and lymphatic tissue in the muscle, make it an unfavorable medium for the growth of mycobacterium tuberculosis [7]. This explains why the muscular involvement in tuberculosis usually comes from the extension of a bone, articular or tendonous focus, a direct inoculation or a haematogenic or lymphatic dissemination [8]. In our case, the isolated localization of the muscles as where no primitive localization has been detected and no notion of iatrogenic inoculation has been reported is extremely rare and would be secondary to a weakening of the muscles by a previously unknown trauma or affection. However, the contamination may have been made from a radiologically undetectable lung focus, particularly in a region with a high TB endemic, such as Morocco.
A review of the literature allowed us to find two cases of extrapulmonary gluteal tuberculosis without bone involvement. For the first case reported by Egin et al. [9], it was a patient followed for end stage renal disease in the hemodialysis stage who developed pyomyositis secondary to TB in the absence of osseous involvement. The diagnosis was confirmed by biopsy and the patient was medically treated. It is well known that patients with chronic renal failure are at increased risk of contracting TB because of their impaired immunity which makes our case even rarer by the immunocompetence of our patient. The second case was reported by Abdelwahab et al. [10], it was a 20-month-old toddler who presented a large swelling of soft tissues of the right gluteal region. The diagnoses mentioned were those of an acute hematoma or a cold abscess. Surgery with biopsy confirmed the presence of a soft tissue tuberculous abscess without bone involvement. The child was then treated successfully with antituberculous chemotherapy. After one year of follow-up, he remained in good health. The rarity of our case is also based on the pseudotumoral form of the gluteal region not reported so far in the literature to our knowledge [11].
With the advent of effective chemotherapeutic agents, the need for surgical treatment in TB patients has evolved considerably. Nevertheless, surgery is often required in patients with pseudotumoral tuberculosis, mainly to validate the diagnosis and as a therapeutic option under certain circumstances to treat the complications or sequelae of the disease.
Conclusion
Although isolated muscle tuberculosis is a rare entity, it must always be taken into consideration as a differential diagnosis for isolated muscle swelling, especially in a country with a high TB endemic. The diagnosis is mainly bacteriological and/or pathological. Treatment uses anti-bacillary chemotherapy alone or in combination with surgery. The prognosis is often favorable when the management is early.
REFERENCES
- World Health Organization-WHO. Global Tuberculosis Report 2017.
- Hayoun S, Ouazzani HE, Habibi B, et al. Tuméfaction du muscle pectoral révélant une tuberculose musculaire isolée. The Pan African Medical Journal. 2017;27:44.
- Kulchavenya E. Extrapulmonary tuberculosis: Are statistical reports accurate? Therapeutic Advances in Infectious Disease. 2014;2(2): 61-70.
- Peto HM, Pratt RH, Harrington TA, et al. Epidemiology of extrapulmonary tuberculosis in the USA, 1993–2006, Clinical Infectious Diseases, 2009; 2: 1350–1357.
- Kim DU, Kim SW, Ju CI. Isolated coccygeal tuberculosis. J Korean Neurosurg Soc. 2012;52(5):495–497.
- Zidane A. Tuberculose de la paroi thoracique: à propos de trois case. Rev Pneumol Clin. 2015; 71(5):290–3.
- Zeng Y, Liu Y, Xie Y, et al. Muscular tuberculosis: A new case and a review of the literature. Front Neurol. 2019;10:1031.
- Abdelwahab IF, Bianchi S, Martinoli C, et al. Atypical extraspinal musculoskeletal tuberculosis in immunocompetent patients: Part II, Tuberculous myositis, tuberculous bursitis, and tuberculous tenosynovitis. Can Assoc Radiol J. 2006; 57(5):278–86.
- Ergin F, Arslan H, Bilezikçi B, et al. Primary tuberculosis in the gluteal muscle of a patient with chronic renal failure. Nephron 2001;89:463-466.
- Abdelwahab IF, Kenan S, Hermann G, et al. Tuberculous gluteal abscess without bone involvement. Skeletal Radiol. 1998;27:36–9. 11.
- Yeon LJ. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberculosis and respiratory diseases. 2015; 78. 47-55.