Pterygomaxillary junction: morphometric analysis and clinical aspect
2 Department of Anatomy, Faculty of Medicine, Akdeniz University, Turkey
Citation: Sindel A, Aytaç G, Öğüt E, et al. Pterygomaxillary junction: morphometric analysis and clinical aspect. Int J Anat Var. 2017;10(S1):62-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The pterygomaxillary fissure is formed by the divergence of the maxilla from the pterygoid process of the sphenoid bone. It connects the infratemporal fossa with the pterygopalatine fossa. During the osteotomies this area couldn’t visualise and osteotomy is performed tactually. Osteotomy is performed by an osteotome or pterygoid chisel. Pterygomaxillary area is an important component of the orthognatic surgeries because during the Le Fort I osteotomies down fracture of maxilla are required. We studied 80 human dried skulls. We investigated the structure of the pterygomaxillary junction and differences between the right and left sides. The length and width of pterygomaxillary junction is measured in sagittal plane. Mean values and standard deviations are calculated and right and left sides are compared. The mean length, and width of the pterygomaxillary junction was 15.3 mm and 7.18 mm, respectively. There was no statistically significant difference between right and left sides of the skulls, but there was significant difference when the skulls compared with each other. The last step of the Le Fort I osteotomies is the separation of the maxilla from the pterygoid plates. For this process, the pterygomaxillary junction should be separated with curved osteotomes. By placing a finger inside the mouth and feeling the hamulus, the medial extent of the osteotome can be palpated to ensure the proper position. Once the osteotomies are completed, the down fracture is performed with digital pressure. Knowledge of the structure, mean values and distinctions of the pterygomaxillary junction is important to prevent possible complications during the orthognatic surgeries.
Keywords
Le fort I; Maxilla; Osteotomies; Pterygomaxillary area; Pterygomaxillary junction
Introduction
The pterygomaxillary fissure is a perpendicular fissure that descends at right angles from the medial end of the inferior orbital fissure and it’s formed by the divergence of the maxilla from the pterygoid process of the sphenoid. It connects the infratemporal fossa with the pterygopalatine fossa. The maxillary artery passes through the pterygomaxillary fissure from the infratemporal fossa to the pterygopalatine fossa, where it terminates as the third part of the maxillary artery. The posterior superior alveolar nerve goes from the pterygopalatine fossa to the infratemporal region through this fissure [1].
The pterygomaxillary region is one of the most difficult territories because of the close relations with the vascular and nervous structures [2]. Pterygopalatine fossa communicated with infratemporal fossa through pterygomaxillary fissure, which the maxillary artery entered in pterygopalatine fossa. The demarcation between pterygopalatine fossa and the greater palatine canal could be differentiated by the pterygomaxillary fissure and pterygomaxillary suture [3].
Le Fort I is the standard procedure for several dentofacial deformities. It is an important procedure to separate the pterygoid plate of sphenoid bone from maxilla precisely [4]. The pterygomaxillary disjunction is one of the most important step during the Le Fort I osteotomies. The separation of maxilla from the skull in the Le Fort I osteotomy without a pterygomaxillary osteotome does not always induced an accurate pterygomaxillary separation. Because of this pterygomaxillary osteotome is appropriate for a safe pterygomaxillary disjunction [5]. Besides surgeons should know the anatomy of this region and the main complications of this step of the surgery that associated with down fracture of the maxilla. This step has greatest potential for accidents and complications [6]. In Le Fort I osteotomy, the junction of the bony tuberosity of the maxilla and the anterior part of the pterygoid plates represents the site of least certain separation. Pterygomaxillary disjunction and maxillary down fractures become even more dangerous if these are traumatic in nature. Anatomical variations can occur at the base of skull such as bony defects or incomplete ossifications [7,8]. There are many complications associated with separation of pterygomaxillary junction such as hemorrhage, infection, nerve injury, oronasal fistula formation, relapse, dental injury airway obstruction, hypomobility after intermaxillary fixation [4,9]. The purpose of this study is to increase the knowledge about the pterygomaxillary junction and to measure the width and length of the junction in the each side of the skull.
Methods
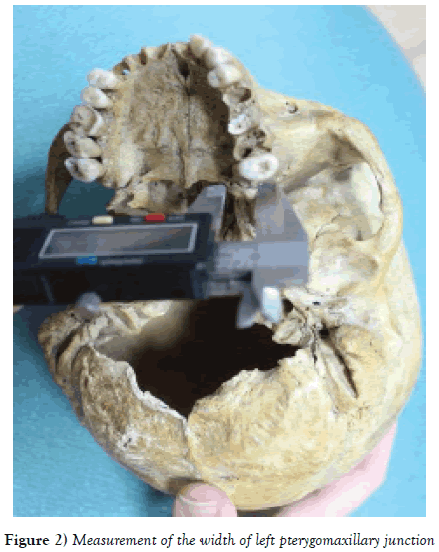
A total number 80 adult dried skull of unknown age and sex were studied for the morphometric measurements of pterygomaxillary junction. For this study calvaria’s intact human skulls obtained from the Akdeniz University Medical Faculty Department of Anatomy. Damaged skulls, new-borns, infant skulls and very old skulls with obliterated sutures were excluded from the study. The length (Figure 1) and the width (Figure 2) of pterygomaxillary junction on both right and left sides were measured using a digital caliper, and the results were compared with paired t-test.
Results
The mean length of the pterygomaxillary junction on the right side was measured 15.01 mm (6.97-24.1 mm) and 15.59 mm (10.04-21.69 mm) on the left sides. Width of the pterygomaxillary junction was measured 6.79 mm (1.61-10.9 mm) on the right, and, 7.58 mm (2.12-10.69 mm) on the left side. Length of the pterygomaxillary junction was measured 15.3 mm (6.97-21.69 mm) in total. Width of the pterygomaxillary junction was measured 7.18 mm (1.61-10.9 mm) in total. There was no statistically significant difference between right and left sides of the skulls, but there was significant difference when the skulls compared with each other (p<0.05).
Discussion and Conclusion
A few studies have been conducted to investigate the anatomical relationships around pterygomaxillary junction. The literature that correlates surgical techniques and anatomical basis of pterygomaxillary region in orthognathic surgeries is limited. The knowledge of this anatomic region for correct disjunction of pterygomaxillary junction during the surgeries is essential. The vascular and nervous structures (maxillary artery, maxillary vein, pterygoid plexus and pterygopalatine ganglion) which locate in this region are important during placement of the instruments that used for pterygomaxillary disjunction (1,10-12). Recent reports highlighted that the pterygomaxillary junction is a critical area for important clinical complications [13].
Le Fort I osteotomy is a widely used maxillary surgical intervention for the correction of dentofacial deformities [14]. Le Fort I osteotomy usually considered a safe, reliable and predictable procedure [15]. The incidence of complications that result from Le Fort I osteotomy is low. But in some patients who have an atypical maxillary morphology this procedure could be much more difficult. Because of this the preoperative identification of potentially difficult cases, is might be crucial in order to prevent or minimize possible complications [16]. Although Le Fort I is a safe method besides frequently occurring complications such as intraoperative and postoperative hemorrhage, infection, nerve injury, oronasal fistula formation, relapse, dental injury, there may be uncommon complications such as visual function, respiratory function, and unusual vascular injury [4]. During this procedure, pterygomaxillary disjunction via an osteotome is required for the complete mobilization of the maxilla. Several authors have indicated that understanding the anatomy of the pterygomaxillary junction region could help preventing blood loss in Le Fort I osteotomies. According to Ueki et al, anatomic variants of the skull base such as bony defects or incomplete ossifications, abnormally thick posterior walls of the maxilla and pterygoid plates could increase the risk of the above mentioned complications [5]. Dolanmaz et al have suggested that the incidence of reported complications less for pterygomaxillary disjunction which carried out with curved osteotomes [9]. In addition, proper positioning of the curved osteotome in the pterygomaxillary fissure could help to avoid damaging the pterygoid plates and adjacent structures. In the Le Fort I osteotomy during orthognathic surgery, some unfavorable fractures have been reported, mainly in the moment of pterygomaxillary disjunction, associated with damage to the descending palatine artery. Also Kang et al have emphasized the importance avoidance of the internal carotid artery injury. The angulation of the curved osteotome plays a key role in avoidance of possible complications secondary to unfavorable fractures of the pterygoid plates. Kim et al measured length and width of pterygomaxillary junction in cone beam computed tomogram and they found 13.22 mm, 8.01 mm respectively [4]. In the present study the length and width of the pterygomaxillary junction are measured 15.3 mm, 7.18 mm without statistically significant difference between the right and left sides of the skulls. We suggested directly usage of curved osteotome for pterygomaxillary disjunction and according to our results osteotomy may need to extend maximum 7-8 mm in horizontal plane and maximum 14-15 mm in the vertical plane. In conclusion, anatomical knowledge of the pterygomaxillary region is important during the pterygomaxillary disjunctions. The pterygomaxillary disjunction is a critical surgical step of Le Fort I osteotomy in orthognathic surgery. Le Fort I osteotomy is related to the pterygomaxillary disjunction so morphometric analyses could help the professionals during execution of the maxillary osteotomy. Using a curved osteotome would provide a safe pterygomaxillary disjunction. Several techniques have been described for the pterygomaxillary disjunction. There are large number of surgical complications exist in this procedure, especially the neurovascular complications. The main reasons of these injuries are poor positioning of chisels and the lack of knowledge of regional anatomy. Present study emphasized that surgeons should be aware of the importance of pterygomaxillary junction anatomy in addition to imaging techniques while performing a complete pterygomaxillary separation during Le Fort I osteotomies.
REFERENCES
- Gray H. Gray's Anatomy. Edinburgh: Longman. 1973.
- Mohor CI. Pterygomaxillary Regıon. Anatomotopographic Particularities. Acta Medica Transilvanica J. 2014;II:220.
- Chen CC, Chen ZX, Yang XD, et al. Comparative research of the thin transverse sectional anatomy and the multislice spiral CT on Pterygopalatine Fossa. Turk Neurosurg. 2010;20:151-8.
- Dong-Yul K, Yeong-Cheol C, Iel-Yong S, et al. Anatomic Study of Pterygomaxillary Junctions in Koreans. J Korean Assoc Maxillofac Plast Reconstr Surg. 2013;35:368-75.
- Ueki K, Hashiba Y, Marukawa K, et al. Assessment of Pterygomaxillary Separation in Le Fort I Osteotomy in Class III Patients. J Oral Maxillofac Surg. 2009;67:833-9.
- Bouloux GF, Bays RA. Neurosensory recovery after ligation of the descending palatine neurovascular bundle during Le Fort I osteotomy. J Oral Maxillofac Surg. 2000;58:841-5.
- Feuerman TF, Hieshima GB, Bentson JR, et al. Carotid-Cavernous Fistula Following Nasopharyngeal Biopsy. Arch Otolaryngol Head Neck Surg. 1984; 110: 412-414.
- Renn WH, Rhoton jr AL. Microsurgical anatomy of the sellar region. J Neurosurg. 1975;43:288-98.
- Dolanmaz D, Esen A, Emlik D, et al. Comparison of two different approaches to the pterygomaxillary junction in Le Fort I osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e1-5.
- Fonseca RJ, Walker RV. Oral and maxillofacial trauma, vol. 1. Philadelphia: Ed. Saunders Co. 1991.
- Gray H. Gray's Anatomy. London: Churchill Livingstone. 1995.
- Methathrathip D, Apinhasmit W, Chompoopong S, et al. Anatomy of greater palatine foramen and canal and pterygopalatine fossa in Thais: considerations for maxillary nerve block. Surg Radiol Anat 2005;27:511-6.
- Betts NJ, Ziccardi VB. Oral and maxillofacial surgery. Philadelphia: W.B. Saunders. 2000.
- Buchanan EP, Hyman CH. LeFort I Osteotomy. Semin Plast Surg. 2013;27:149-54.
- Hernandez-Alfaro F, Guijarro-Martinez R. "Twist technique" for pterygomaxillary dysjunction in minimally invasive Le Fort I osteotomy. J Oral Maxillofac Surg. 2013;71:389-92.
- Hoffman GR, Islam S. The difficult Le Fort I osteotomy and downfracture: a review with consideration given to an atypical maxillary morphology. J Plast Reconstr Aesthet Surg. 2008;61:1029-33.