Quality of life of children with sickle cell disease and impaired pulmonary functions
2 Department of Pathology, Slamanyia Medical Complex, Manama, Bahrain
Received: 19-Mar-2021 Accepted Date: Apr 05, 2021; Published: 12-Apr-2021
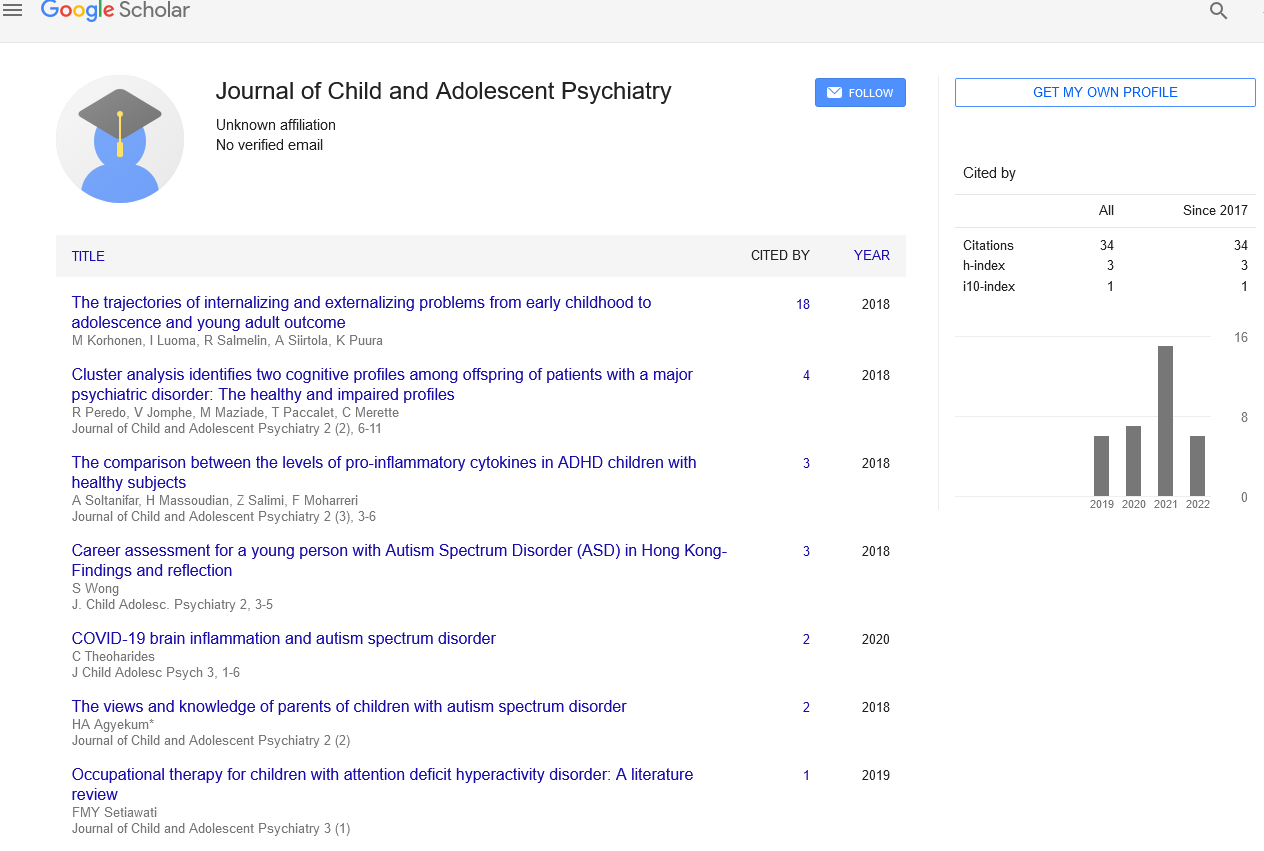
Citation: Al-Biltagi M, Bediwy AS, Saeed NK. Quality of life of children with sickle cell disease and impaired pulmonary functions. J Child Adolesc Psych.5(S1):3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Sickle Cell Disease (SCD) affects all the domains of quality of life in the affected children, including the physical, psychosocial, and cognitive and morbidity domains. This effect will be augmented in the presence of an impaired pulmonary function test. There are no studies that correlated the degree of impaired pulmonary function in children with SCD with the degree of impairment of their quality of life. Besides, it is very challenging to segregate the effect of SCD on the child’s quality of life from impaired pulmonary function. Hence more studies are needed.
Keywords
Sickle cell disease; Pulmonary function; Quality of life
INTRODUCTION
It seems that the concept of quality of life appeared to the public with the announcement by US President Nixon in 1964 when he said, “the great society is concerned not with how much, but with how good-not with the quantity of goods but with the quality of [its members’] lives” [1]. In the beginning, the aim of quality of life for a sick child was to improve survival. However, with the significant increases in survival for children with chronic conditions using advanced treatment strategies, the domain of quality of life changed to decrease the negative consequences of the disease and the impact of its treatment coupled with improving the self-esteem, and the sense of physical, psychological, economic, and social well-being, considering the developmental stage of the child [2]. Quality of life is defined as “the subjective reported well-being regarding the child’s physical and mental health, self-esteem and perception of own activities (playing/having hobbies), perceived relationship to friends and family as well as to school” [3].
LChildren with chronic diseases have a markedly impaired quality of their lives. Chronic conditions affect the physical and functional status, emotional balance, their self-esteem. Chronic diseases’ impacts on the different domains of the quality of life vary from one disease to another. Sickle Cell Disease (SCD) affects all the domains of quality of life in the affected children, including the physical, psychosocial, and cognitive and morbidity domains [4]. It affects the quality of life of the child through different mechanisms. The disease’s recurrent or chronic nature with the need for frequent hospital admissions and recurrent blood transfusions or periodic visits affects child playing and mobility, limiting his daily activities and impairing school attendance, vocational achievement perception, entertainment, and cultural participation activities. The painful and the other intermittent crises increase post-traumatic stress disorder incidence due to poor sleep quality, high incidence of anxiousness and exhaustion and negative fitness and energetic feeling trends. The need for regular investigations, medications, and follow up added to the occasional need for blood transfusion also are crucial factors compromising the child quality of life. Besides, the enormous financial and emotional burdens that face the caregivers further impair the affected children’s quality of life [5,6]. A study in Saudi Arabia showed that poor education, fever, skin redness, swelling, and history of blood transfusion in children with SCD are associated with more inferior quality of life, whereas regular exercise tended to improve it [7].
SCD can provoke both acute and chronic pulmonary disorders. In our previous study, we found significant worsening of the pulmonary function, including obstructive and/or restrictive abnormalities, correlated with the disease progression, older age, and repeated occurrence of acute chest syndrome [8]. Many healthcare providers underappreciated the presence of impairment of the pulmonary function, despite being a crucial respiratory complication with genuine threats to patients’ health and life with SCD. Many studies also showed that impaired pulmonary function test impairs the quality of life in children with different chronic diseases [9].
Impaired pulmonary function negatively impairs exercise performance and increases hospitalization frequency, which compromises school and emotional functioning and diminishes the quality of life [10]. When coupled with a load of sickle cell disease, the quality of life markedly diminishes in children who have SCD complicated with impaired pulmonary function. Hence, the pulmonary function should be monitored early in life, from childhood, in children with SCD, as a part of a program to improve the quality of life. There are no studies that correlated the degree of impaired pulmonary function in children with SCD with the degree of impairment of their quality of life. Also, it is challenging to segregate the effect of SCD on the child’s quality of life from impaired pulmonary function. Hence more studies are needed.
REFERENCES
- Rapley M Quality of Life Research: a Critical Introduction. Quality of Life Research. 2004;13:1021-24.
- Spieth LE: Generic health related quality of life measures for children and adolescent. In Quality of Life in Child and Adolescent Illness. 2001;49-88.
- Jozefiak T, Larsson B Wichstrøm L. et al. Quality of Life as reported by school children and their parents: A cross-sectional survey. Health Qual Life Outcomes. 2008;19:1-11.
- Patel AB, Pathan HG, Quality of life in children with sickle cell hemoglobinopathy. Indian J Pediatr. 2005;72:567-71.
- Madani BM, Al Raddadi R, Al Jaouni S, et al. Quality of life among caregivers of sickle cell disease patients: a cross sectional study. Health Qual Life Outcomes2018;10:1-9.
- Stegenga KA, Ward-Smith P Hinds PS, et al Quality of life among children with sickle cell disease receiving chronic transfusion therapy. J Pediatr Oncol Nurs. 2004;21:207-13.
- Ahmed AE, Alaskar AS, Al-Suliman AM, et al. Health-related quality of life in patients with sickle cell disease in Saudi Arabia. Health Qual Life Outcomes. 2015;13:1-9.
- Al Biltagi M, Bediwy AS, Toema O, et al. Pulmonary functions in children and adolescents with sickle cell disease. Pediatr Pulmonol. 2020;55:2055-63.
- Abassi H, Gavotto A, Picot MC, et al. Impaired pulmonary function and its association with clinical outcomes, exercise capacity and quality of life in children with congenital heart disease. Int J Cardiol. 2019;15:86-92.
- Vandekerckhove K, Keyzer M, Cornette J, et al. Exercise performance and quality of life in children with cystic fibrosis and mildly impaired lung function: relation with antibiotic treatments and hospitalization. Eur J Pediatr. 2017;176:1689-96.