Radiomics: A quantitative approach to medical imaging
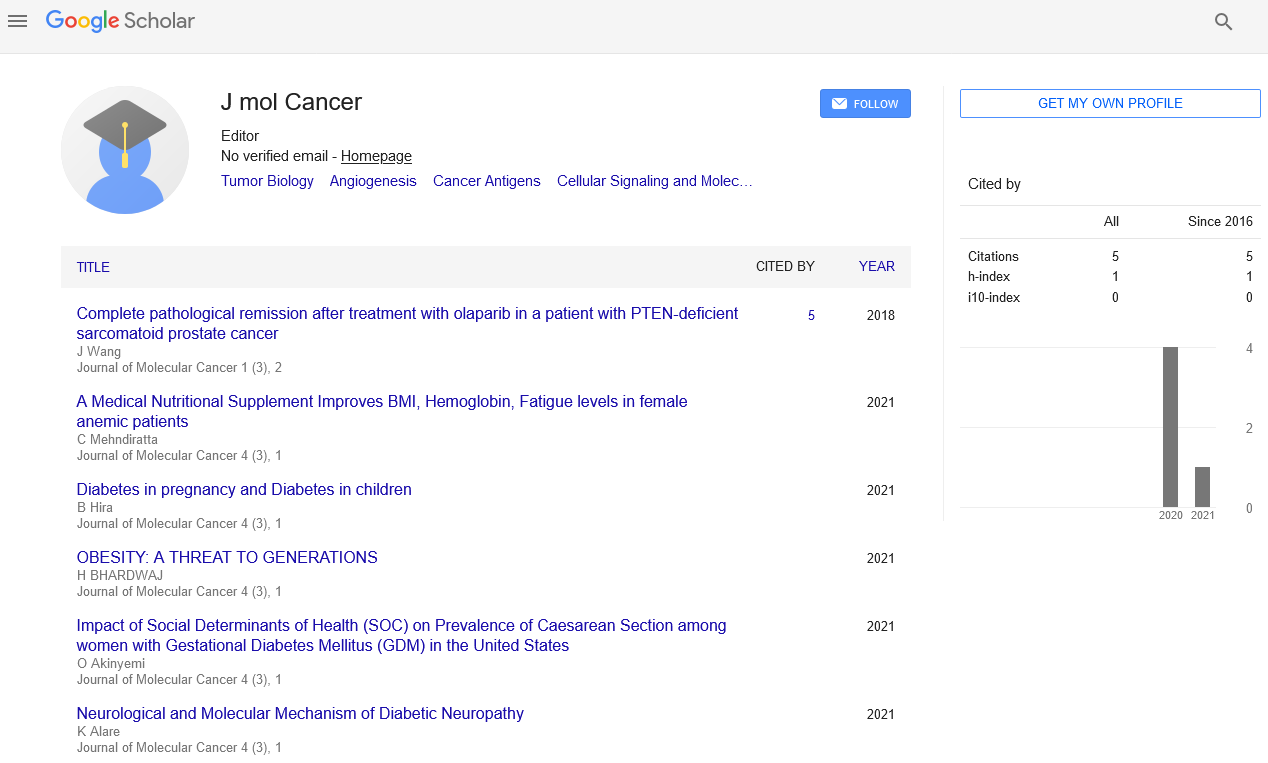
Received: 03-Jan-2022, Manuscript No. PULJMC-22-4233; Editor assigned: 05-Jan-2022, Pre QC No. PULJMC-22-4233(PQ); Accepted Date: Jan 05, 2022; Reviewed: 11-Jan-2022 QC No. PULJMC-22-4233; Revised: 16-Jan-2022, Manuscript No. PULJMC-22-4233(R); Published: 27-Jan-2022, DOI: doi:10.37532/puljmc.22.5.1.1
Citation: Ryujin K. Radiomics: A quantitative approach to medical imaging. J Mol Cancer. 2022;5(1):1.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Immunotherapies are prompting further developed results for some, malignant growths, incorporating those with destroying visualizations. As treatments like Resistant Designated Spot Inhibitors (ICI) become a backbone in treatment regimens, numerous simultaneous difficulties have emerged - for example, portraying clinical responders from non-responders. Anticipating reaction has demonstrated to be troublesome given an absence of predictable and exact biomarkers, Heterogeneity of The Growth Microenvironment (TME), and a helpless comprehension of opposition systems. Generally, imaging information have stayed an undiscovered, yet bountiful, asset to address these difficulties. As of late, quantitative picture investigations have featured the utility of clinical imaging in foreseeing growth aggregates, anticipation, and helpful reaction. These investigations have been filled by a blast of assets in high-throughput mining of picture highlights (eg; radiomics) and man-made brainpower. In this survey, we feature current advancement in radiomics to comprehend cancer invulnerable science and foresee clinical reactions to immunotherapies. We likewise examine constraints in these investigations and future bearings for the field, especially if high-layered imaging information are to assume a bigger part in accuracy medication.
Key Words
Radiogenomic; Radiomics; Myeloid inferred silencer cells
Introduction
Radiomics alludes to the method involved with evaluating patient-explicit tissue attributes from pictures to create high-layered minable highlights, or picture biomarkers. These elements can length from straightforward illustrative quantitative data, like calculation and force, to complex higher request connections like surface. Such pictures are ordinarily acquired from CT, MRI, and PET, and can be additionally handled with channels or changes (for example Gabor, wavelet) before include extraction. The hidden theory is that sure parts of growth science, like vascularization, level of irritation, spatial association and heterogeneity, characterize building highlights that can be caught by high-goal imaging and evaluated numerically. Radiomic information can be strong assets for clinical oncology for a considerable length of time. All malignant growth patients go through imaging during their analysis and treatment course, making these kinds of information all the more all-around accessible. Rather than being restricted to a small bunch of highlights, radiogenomic connections can now be performed across many picture attributes. A bigger exhibit of highlights that characterize more mind boggling growth designs might support the investigation of intricate and heterogeneous areas of cancer science, for example, the growth insusceptible microenvironment, that have escaped our seeing up to this point. Understanding the growth invulnerable microenvironment is vital given its basic job in deciding growth reaction to hostile to disease treatments like Insusceptible Designated Spot Inhibitors (ICIs). Aggravation of the growth microenvironment can be favorable to cancer or against growth relying upon the resistant setting. Persistent irritation can advance cancer development by empowering autocrine flagging circles that drive cell expansion, expanded angiogenesis, invulnerable avoidance, and metastasis. Both intrinsic and versatile resistant cells collaborate with one another and the cancer to manage aggravation, eventually directing the course of growth movement. The equilibrium of against growth insusceptible cells, like cytotoxic T cells and NK cells, with cells that smother the counter cancer safe reaction, especially administrative T cells (Tregs), Myeloid Inferred Silencer Cells (MDSCs), and cancer related macrophages, likewise oversees the degree to which tumors react to specific treatments.
Conclusion
The objective of growing more powerful expectation models from radiomics and other growth properties is to eventually give better customized care to patients. As more designated treatments and immunotherapies rise out of clinical preliminaries, the requirement for techniques to expand clinical dynamic will increment. Accuracy medication stands to benefit hugely from more precise portrayal of the 3D cancer invulnerable microenvironment, distinguishing prognostic biomarkers for immunotherapy, and giving clinical direction in the setting of immunotherapy obstruction. In light of concentrates to date, there is developing proof that cancer resistant states can be described by radiomic includes alone or in blend with other atomic and histological elements. All the more along these lines, gauge imaging highlights as well as changes in highlights seem to give another wellspring of prescient power for immunotherapy reaction. Nonetheless, current radiomic discoveries are for the most part not full grown to the point of filling in as substitute indicators of resistant science, as few radiogenomic affiliations have been entirely approved. Moreover, while studies can restate resistant relationship with low intricacy highlights, relationship with surface elements are more dubious. In general, radiogenomic displaying applied to cancer invulnerable science is at its early stages. Improvement of clinically applicable radiogenomic models should be joined by a guide for specialized and natural approval, as well as smart incorporation of other organic (“omic”) and clinical information to foster more precise, composite models.