Rare variations in vascular pattern of thyroid gland
Veena Kulakarni*, Sunkeswari Sreepadma and S.K.Deshpande
Department of Anatomy, SDM Medical College, Sattur, Dharwad, Karnataka, INDIA.
- *Corresponding Author:
- Dr. Veena Kulkarni
Associate Professor Department of Anatomy SDM Medical College Sattur, Dharwad Karnataka, India.
Tel: +91 (836) 2448244
E-mail: dr.veenapuranik@gmail.com
Date of Received: August 6th, 2012
Date of Accepted: October 2nd, 2013
Published Online: May 6th, 2014
© Int J Anat Var (IJAV). 2014; 7: 4–6.
[ft_below_content] =>Keywords
thyroid gland,superior thyroid artery,inferior thyroid vein,anatomical variations
Introduction
The thyroid gland, is placed anteriorly in the lower neck, level with the fifth cervical to the first thoracic vertebrae. Ensheathed by the pretracheal fascia, the gland consists of two lateral conical lobes connected by a narrow median isthmus. Each lobe measures 5 cm long, its greatest transverse and anteroposterior extents being 3 cm and 2 cm, respectively. The isthmus connects the lobe’s lower parts; it measures 1.25 cm transversely and vertically, and is usually anterior to the second and third tracheal cartilages, though often higher or sometimes lower because its site and size vary greatly. Occasionally, the isthmus may be absent [1]. The superior thyroid arteries anastomose along its upper border; at the lower border the inferior thyroid veins leave the gland.
The superior thyroid artery (STA) is a branch arising from front of external carotid artery, gives glandular branches which on reaching the superior pole of the gland divide into anterior and posterior branches. The anterior branch accompanies the medial border of lateral lobe and anastomoses with its fellow of opposite side along the upper border of the isthmus of the gland. The posterior branch passes downward along the posterior border of lateral lobe and anastomoses with the ascending branch of inferior thyroid artery. The superior thyroid artery supplies the capsule and the connective tissue of the gland.
The inferior thyroid artery a branch from thyrocervical trunk penetrates the deep surface of the gland and supplies the parenchyma of the gland. The gland is also supplied by numerous accessory thyroid arteries and occasionally by arteria thyroidea ima.
Case Report
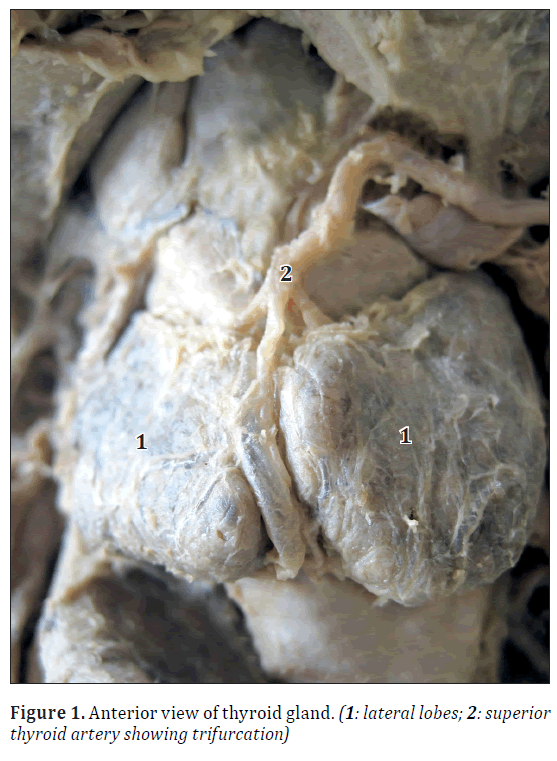
During routine dissection of a 57-year-old male cadaver, on the right side, superior thyroid artery, arising from external carotid artery, showed trifurcation on reaching the gland, in the midline of the neck (Figure 1). One branch was supplying to the right lobe, the second was supplying to the left lobe and the middle branch ran in the midline along with the inferior thyroid vein in the median groove, then pierced the gland along the lower edge of the groove.
The lobes were quadrilateral in shape in contrast to the normal conical shape and there was a prominent median groove wherein the branches of superior thyroid artery and the tributary of the inferior thyroid veins were lodged. The lobes were measuring 3.1 x 4.2 x 2.1 cm along their length, transversely and anteroposteriorly.
There was no reference to any surgical intervention in the neck region in patient’s clinical history and neither were any scars found in the cervical region. The STA on the left side was as usual, dividing into anterior and posterior branches supplying the anterior, medial and lateral surfaces.
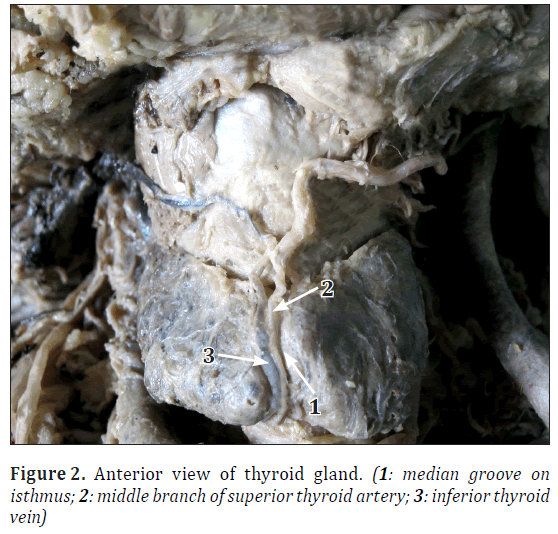
The isthmus could not be distinguished from the lobes as it was very much reduced and it appeared as the lobes have fused along their anterior borders with a prominent median groove lodging the vessels, and its lower border had a prominent notch from where the inferior thyroid veins were emerging.
No ectopic thyroid tissue was observed.
The inferior thyroid artery on both sides was arising from the thyrocervical trunk. On left side, the artery on reaching the lower pole of the gland, divided into ascending and descending branches which pierced the posterior and inferior surfaces of the gland to supply it. On right side, the artery and its branches coursed in usual pattern.
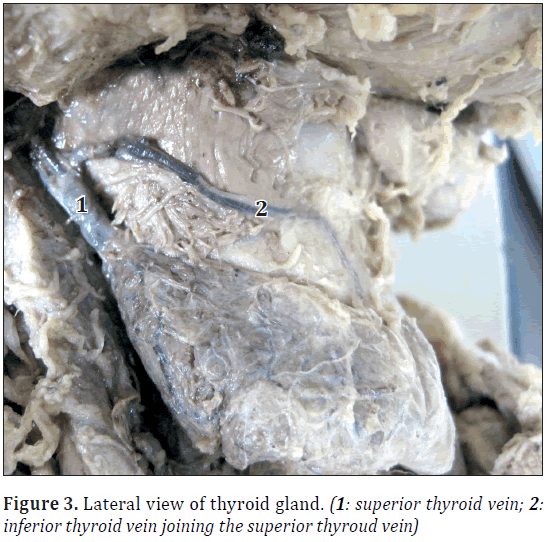
The inferior thyroid vein emerged from the lower border of the isthmus and ascended upwards in the median groove to join the superior thyroid vein and finally drained into the internal jugular vein on left side (Figures 2, 3).
Discussion
The anomalies of the development of the thyroid gland distort the morphology of the gland, and may cause clinical functional disorders and various thyroid illnesses [2]. The thyroid gland is a midline derivative of pharynx. It develops from an endodermal diverticulum, the thyroglossal duct. The tip of the duct bifurcates and the tissue mass subsequently divides into a series of double cellular plates, from which the isthmus and lateral lobes are developed.
The STA is the main source of artery to the thyroid gland, upper part of the larynx and neck region. It is the branch of external carotid artery, and arises just below the level of greater horn of the hyoid bone. The STA is the primitive artery to the gland and is a more constant vessel and is rarely absent.
It is important to know the possible variations of origin and course of STA and its branching pattern. Lack of knowledge regarding the possible variations could lead to fatal errors if one blood vessel is mistaken for another. Knowledge of surgical anatomy of the STA ensures maintaining a bloodless surgical field during major radical neck dissection surgeries to minimize postoperative complications [3].
Bergman et al., reported that STA is generally considered to be present in 100% of cases and its absence has only been reported once. An unusually large STA may replace the contralateral vessels or the inferior thyroid artery [4]. The superior thyroid artery was more frequently present as compared to the inferior thyroid artery and the variability of the superior thyroid artery may be influenced by the anthropological factors. The lowest incidence arterial variants of the thyroid gland have been recorded in the Swiss population with the highest in the Americans. However, there is paucity of literature with regard to unusual STAs in the Asian subcontinent especially in India [5]. Variations in the origin of STA are important in preoperative selective arterial angiograms to map out the vascularity and the true extent of the tumors of the head, neck and face. It is also important in cases of selective arterial embolization to reduce the vascularity of the tumors of the head, neck and face and in selective intraarterial chemotherapy [6]. Head and neck surgeons must be familiar with anatomical variations of the STA in order to achieve a better surgical outcome.
Similarly, knowledge of the anatomy of the veins in the anterolateral cervical region, particularly the thyroid veins, is important because of its application in thyroid, parathyroid and laryngeal surgery, in the transposition of myocutaneous flaps for reconstructions and, particularly, in tracheostomies [7].
High tracheostomy is performed between the cricoid cartilage and the isthmus of the thyroid gland. In operation of low tracheostomy the trachea is opened below the isthmus of the thyroid gland. The frequency of indications for tracheostomy in emergency rooms and intensive care units is increasing and thus the occurrence of hemorrhagic events is increasing likewise. Krausen reports that many surgeons have been dismayed at the occurrence of massive hemorrhages caused by accidental section of the inferior thyroid vein during emergency or even routine tracheostomies [8]. Buguet-Brown et al. reported a case of catastrophic acute hemorrhage caused by lesion of the inferior thyroid vein in percutaneous tracheostomy [9]. Muhammad et al. report 4.8% unsuccessful tracheostomies where hemorrhages were caused by vascular lesions and recommend the use of ultrasonography to assess anatomical variations of these vessels [10].
Conclusion
Disruption of the vessels supplying the thyroid gland by trauma or malignant invasion of the vessel wall can result in death by bleeding. Each surgical technique has its risks and complications, and it is important to know the anatomy of the vasculature of thyroid gland and its possible variations for a safe and effective surgery.
References
- Standring S, ed. Gray’s Anatomy. 40th Ed., Edinburgh, Churchill Livingstone. 2008: 462–464.
- Ranade AV, Rai R, Pai MM, Nayak SR, Prakash, Krisnamurthy A, Narayana S. Anatomical variations of the thyroid gland: possible surgical implications. Singapore Med J. 2008; 49: 831–834.
- Anitha T, Dombe D, Asha K, Kalbande S. Clinically relevant variations of the superior thyroid artery: An anatomic guide for neck surgeries. Int J Pharm Biomed Sci. 2011; 2: 51–54.
- Rao TR, Balakrishnan R, Prakashchandra S, Suresh R. Ectopic thyroid tissue with a rare vascular variation. Int J Morphol. 2007; 25: 121–124.
- Mehta V, Suri RK, Arora J, Rath G, Das S. Anomalous superior thyroid artery. Kathmandu Univ Med J (KUMJ). 2010; 8: 429–431.
- Shintani S, Terakado N, Alcalde RE, Tomizawa K, Nakayama S, Ueyema Y, Ichikawa H, Sugimoto K, Matsumura T. An anatomical study of the arteries for intraarterial chemotherapy of head and neck cancer. Int J Clin Oncol.1999; 4: 327–330.
- Wafae N, Hirose K, Franco C, Wafae GC, Ruiz CR, Daher L, Person OC. The anatomy of the human thyroid veins and its surgical application. Folia Morphol (Warsz). 2008; 67: 221–225.
- Krausen AS. The inferior thyroid veins. The ultimate guardians of the trachea. Laryngoscope. 1976; 86: 1849–1855.
- Buguet-Brown ML, Favier JC, Da Conceiçao M, Pitti R. Acute severe hemorrhage by a wound of the inferior thyroid vein during percutaneous tracheostomy. Ann Fr Anesth Reanim. 2001; 20: 304–305. (French)
- Muhammad JK, Patton DW, Evans RM, Major E. Percutaneous dilatational tracheostomy under ultrasound guidance. Br J Oral Maxillofac Surg. 1999; 37: 309–311.
Veena Kulakarni*, Sunkeswari Sreepadma and S.K.Deshpande
Department of Anatomy, SDM Medical College, Sattur, Dharwad, Karnataka, INDIA.
- *Corresponding Author:
- Dr. Veena Kulkarni
Associate Professor Department of Anatomy SDM Medical College Sattur, Dharwad Karnataka, India.
Tel: +91 (836) 2448244
E-mail: dr.veenapuranik@gmail.com
Date of Received: August 6th, 2012
Date of Accepted: October 2nd, 2013
Published Online: May 6th, 2014
© Int J Anat Var (IJAV). 2014; 7: 4–6.
Abstract
The thyroid gland is the most vascular endocrine gland. Knowledge of anatomical variations of the vessels supplying the thyroid gland is of utmost importance to surgeons operating in that region to avoid any catastrophic outcomes. During routine dissection of neck region, anatomy of thyroid gland in a cadaver caught our attention as it had multiple variations. The lateral lobes were quadrilateral in shape. The branching pattern of superior thyroid artery on left side showed trifurcation along the midline of superior border of isthmus. The inferior thyroid vein took a longer course and joined with the superior thyroid vein to drain into the left internal jugular vein instead of left brachiocephalic vein. The implications of such variations in relation to the anatomy of the thyroid gland is relevant for academic and clinical purposes.
-Keywords
thyroid gland,superior thyroid artery,inferior thyroid vein,anatomical variations
Introduction
The thyroid gland, is placed anteriorly in the lower neck, level with the fifth cervical to the first thoracic vertebrae. Ensheathed by the pretracheal fascia, the gland consists of two lateral conical lobes connected by a narrow median isthmus. Each lobe measures 5 cm long, its greatest transverse and anteroposterior extents being 3 cm and 2 cm, respectively. The isthmus connects the lobe’s lower parts; it measures 1.25 cm transversely and vertically, and is usually anterior to the second and third tracheal cartilages, though often higher or sometimes lower because its site and size vary greatly. Occasionally, the isthmus may be absent [1]. The superior thyroid arteries anastomose along its upper border; at the lower border the inferior thyroid veins leave the gland.
The superior thyroid artery (STA) is a branch arising from front of external carotid artery, gives glandular branches which on reaching the superior pole of the gland divide into anterior and posterior branches. The anterior branch accompanies the medial border of lateral lobe and anastomoses with its fellow of opposite side along the upper border of the isthmus of the gland. The posterior branch passes downward along the posterior border of lateral lobe and anastomoses with the ascending branch of inferior thyroid artery. The superior thyroid artery supplies the capsule and the connective tissue of the gland.
The inferior thyroid artery a branch from thyrocervical trunk penetrates the deep surface of the gland and supplies the parenchyma of the gland. The gland is also supplied by numerous accessory thyroid arteries and occasionally by arteria thyroidea ima.
Case Report
During routine dissection of a 57-year-old male cadaver, on the right side, superior thyroid artery, arising from external carotid artery, showed trifurcation on reaching the gland, in the midline of the neck (Figure 1). One branch was supplying to the right lobe, the second was supplying to the left lobe and the middle branch ran in the midline along with the inferior thyroid vein in the median groove, then pierced the gland along the lower edge of the groove.
The lobes were quadrilateral in shape in contrast to the normal conical shape and there was a prominent median groove wherein the branches of superior thyroid artery and the tributary of the inferior thyroid veins were lodged. The lobes were measuring 3.1 x 4.2 x 2.1 cm along their length, transversely and anteroposteriorly.
There was no reference to any surgical intervention in the neck region in patient’s clinical history and neither were any scars found in the cervical region. The STA on the left side was as usual, dividing into anterior and posterior branches supplying the anterior, medial and lateral surfaces.
The isthmus could not be distinguished from the lobes as it was very much reduced and it appeared as the lobes have fused along their anterior borders with a prominent median groove lodging the vessels, and its lower border had a prominent notch from where the inferior thyroid veins were emerging.
No ectopic thyroid tissue was observed.
The inferior thyroid artery on both sides was arising from the thyrocervical trunk. On left side, the artery on reaching the lower pole of the gland, divided into ascending and descending branches which pierced the posterior and inferior surfaces of the gland to supply it. On right side, the artery and its branches coursed in usual pattern.
The inferior thyroid vein emerged from the lower border of the isthmus and ascended upwards in the median groove to join the superior thyroid vein and finally drained into the internal jugular vein on left side (Figures 2, 3).
Discussion
The anomalies of the development of the thyroid gland distort the morphology of the gland, and may cause clinical functional disorders and various thyroid illnesses [2]. The thyroid gland is a midline derivative of pharynx. It develops from an endodermal diverticulum, the thyroglossal duct. The tip of the duct bifurcates and the tissue mass subsequently divides into a series of double cellular plates, from which the isthmus and lateral lobes are developed.
The STA is the main source of artery to the thyroid gland, upper part of the larynx and neck region. It is the branch of external carotid artery, and arises just below the level of greater horn of the hyoid bone. The STA is the primitive artery to the gland and is a more constant vessel and is rarely absent.
It is important to know the possible variations of origin and course of STA and its branching pattern. Lack of knowledge regarding the possible variations could lead to fatal errors if one blood vessel is mistaken for another. Knowledge of surgical anatomy of the STA ensures maintaining a bloodless surgical field during major radical neck dissection surgeries to minimize postoperative complications [3].
Bergman et al., reported that STA is generally considered to be present in 100% of cases and its absence has only been reported once. An unusually large STA may replace the contralateral vessels or the inferior thyroid artery [4]. The superior thyroid artery was more frequently present as compared to the inferior thyroid artery and the variability of the superior thyroid artery may be influenced by the anthropological factors. The lowest incidence arterial variants of the thyroid gland have been recorded in the Swiss population with the highest in the Americans. However, there is paucity of literature with regard to unusual STAs in the Asian subcontinent especially in India [5]. Variations in the origin of STA are important in preoperative selective arterial angiograms to map out the vascularity and the true extent of the tumors of the head, neck and face. It is also important in cases of selective arterial embolization to reduce the vascularity of the tumors of the head, neck and face and in selective intraarterial chemotherapy [6]. Head and neck surgeons must be familiar with anatomical variations of the STA in order to achieve a better surgical outcome.
Similarly, knowledge of the anatomy of the veins in the anterolateral cervical region, particularly the thyroid veins, is important because of its application in thyroid, parathyroid and laryngeal surgery, in the transposition of myocutaneous flaps for reconstructions and, particularly, in tracheostomies [7].
High tracheostomy is performed between the cricoid cartilage and the isthmus of the thyroid gland. In operation of low tracheostomy the trachea is opened below the isthmus of the thyroid gland. The frequency of indications for tracheostomy in emergency rooms and intensive care units is increasing and thus the occurrence of hemorrhagic events is increasing likewise. Krausen reports that many surgeons have been dismayed at the occurrence of massive hemorrhages caused by accidental section of the inferior thyroid vein during emergency or even routine tracheostomies [8]. Buguet-Brown et al. reported a case of catastrophic acute hemorrhage caused by lesion of the inferior thyroid vein in percutaneous tracheostomy [9]. Muhammad et al. report 4.8% unsuccessful tracheostomies where hemorrhages were caused by vascular lesions and recommend the use of ultrasonography to assess anatomical variations of these vessels [10].
Conclusion
Disruption of the vessels supplying the thyroid gland by trauma or malignant invasion of the vessel wall can result in death by bleeding. Each surgical technique has its risks and complications, and it is important to know the anatomy of the vasculature of thyroid gland and its possible variations for a safe and effective surgery.
References
- Standring S, ed. Gray’s Anatomy. 40th Ed., Edinburgh, Churchill Livingstone. 2008: 462–464.
- Ranade AV, Rai R, Pai MM, Nayak SR, Prakash, Krisnamurthy A, Narayana S. Anatomical variations of the thyroid gland: possible surgical implications. Singapore Med J. 2008; 49: 831–834.
- Anitha T, Dombe D, Asha K, Kalbande S. Clinically relevant variations of the superior thyroid artery: An anatomic guide for neck surgeries. Int J Pharm Biomed Sci. 2011; 2: 51–54.
- Rao TR, Balakrishnan R, Prakashchandra S, Suresh R. Ectopic thyroid tissue with a rare vascular variation. Int J Morphol. 2007; 25: 121–124.
- Mehta V, Suri RK, Arora J, Rath G, Das S. Anomalous superior thyroid artery. Kathmandu Univ Med J (KUMJ). 2010; 8: 429–431.
- Shintani S, Terakado N, Alcalde RE, Tomizawa K, Nakayama S, Ueyema Y, Ichikawa H, Sugimoto K, Matsumura T. An anatomical study of the arteries for intraarterial chemotherapy of head and neck cancer. Int J Clin Oncol.1999; 4: 327–330.
- Wafae N, Hirose K, Franco C, Wafae GC, Ruiz CR, Daher L, Person OC. The anatomy of the human thyroid veins and its surgical application. Folia Morphol (Warsz). 2008; 67: 221–225.
- Krausen AS. The inferior thyroid veins. The ultimate guardians of the trachea. Laryngoscope. 1976; 86: 1849–1855.
- Buguet-Brown ML, Favier JC, Da Conceiçao M, Pitti R. Acute severe hemorrhage by a wound of the inferior thyroid vein during percutaneous tracheostomy. Ann Fr Anesth Reanim. 2001; 20: 304–305. (French)
- Muhammad JK, Patton DW, Evans RM, Major E. Percutaneous dilatational tracheostomy under ultrasound guidance. Br J Oral Maxillofac Surg. 1999; 37: 309–311.