Results of brain transcatheter laser revascularization in the treatment of the consequences of ischemic stroke
Received: 06-Sep-2017 Accepted Date: Sep 27, 2017; Published: 05-Oct-2017
Citation: Maksimovich IV. Results of brain transcatheter laser revascularization in the treatment of the consequences of ischemic stroke. J Vas Dis Treat. 2017;1(1):02-05.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: The research focuses on the degree of blood supply restoration in the brain by means of transcateter laser revascularization in patients after ischemic stroke.
Materials and Methods: 874 patients 29-81 years old (average age 74) after ischemic stroke were examined: 647 men (74.03%), 227 women (25.79%).
The examination included CDR, MMSE, IB, cerebral CT, MRI, MRA, scintigraphy (SG), rheoencephalography (REG), cerebral MUGA. Test Group was comprised of 533 (60.98%) patients undergoing transcatheter interventions. Control Group included 341 (39.11%) patients receiving conservative treatment. High-energy and low-energy lasers were used for cerebral revascularization.
Results:
Test Group:
• Good clinical outcome was achieved in 323 (60.60%) cases;
• Satisfactory clinical outcome was acquired in 136 (25.52%) cases;
• Relatively satisfactory clinical outcome was procured in 74 (13.88%) cases;
• Relatively positive clinical outcome was not gained in any case.
Control group:
• Good clinical outcome - 51 (21.07%) cases;
• Satisfactory clinical outcome - 72 (21.11%) cases;
• Relatively satisfactory clinical outcome - 123 (36.07%) cases;
• Relatively positive clinical outcome - 95 (27.86%) cases.
Conclusion: Transcatheter laser revascularization is much more effective in the treatment of ischemic stroke consequences than conservative methods of treatment are. When intracerebral blood flow is restored, it reduces the level of mental, cognitive, and motor disorders and helps to quickly bring patients back to their active daily life.
Keywords
Ischemic stroke; Transcatheter laser Revascularization; Cerebrovascular insufficiency; Dementia
Introduction
The number of patients who underwent ischemic stroke increases every year [1]. Ischemic stroke often leads to pronounced neurological deficit, which is accompanied by a 30% mortality rate in the acute period, with 12-15% more patients die in the following 12 months [2]. The remaining patients acquire severe disability with marked motor and speech disorders, dementia and cognitive impairment [3-5]. In the United States, about 800,000 strokes are recorded each year [6].
The leading cause of stroke is atherosclerotic lesion of the cerebral vascular system [7,8]. Atherosclerosis affects not only extracranial and intracranial arterial branches, but also the cerebral capillary bed [5,9,10]. Brain tissues greatly suffer from blood supply disorders; the progression of hypoperfusion quickly leads to ischemia and neurodegenerative lesions [8]. The more pronounced the hypoperfusion zone is and the more it spreads to various cerebral parts, the harder the stroke and its consequences are [2]. The severity of the stroke heavily depends on the development of the cerebral collateral channel [5,10]. Stroke treatment, regardless of its timing, should first be aimed at restoring cerebral blood supply [5,6,11].
Since cerebral atherosclerosis multiply affects vessels in the overwhelming majority of cases and is accompanied by severe hemodynamic disorders, conservative methods of treatment do not always allow to seriously improve the cerebral blood supply [5,12].
Reconstructive surgical interventions are well-proven on extracranial sections of brachiocephalic branches [13]. However, surgery in patients with intracranial lesions is fairly difficult [14].
Transcatheter operative interventions have also proven themselves well on extracranial vessels [15]. However, interventions on the proximal sections of intracranial vessels require the use of small-diameter stents and miniature distal protection means. Conducting such manipulations is often associated with a high risk of complications and of stent thrombosis [16]. Stenting of the distal sections of the intracerebral arterial bed is not possible yet. Consequently, there is a necessity to work out new, sparing transcatheter methods that allow working on both proximal and distal sections of the intracranial vascular bed.
The present research focuses on the degree of recovery of blood supply in the brain by means of transcatheter laser revascularization in patients after ischemic strokes. It also investigates how to reduce these patients’ mental, intellectual, and motor disorders in the near and distant future.
Materials and Methods
The Ethics Committee gave their approval of the examination and transcatheter surgery. The patients and their relatives gave their consent to all the medical procedures.
We examined 874 patients from 29 to 81 years old (average age 74) who had predominant intracerebral atherosclerosis and who underwent ischemic stroke in the period from 6 months to 6 years before the examination and treatment: 647 men (74.03%), 227 women (25.79%).
The examination included CDR, MMSE, IB assessment, as well as CT, MRI, MRA, scintigraphy (SG), rheoencephalography (REG), cerebral MUGA:
• Macrofocal strokes were found in 118 (13.50%) cases.
• Medium focal strokes were discovered in 229 (26.20%) cases.
• Microfocal strokes were revealed in 527 (60.30%) cases.
533 (60.98%) patients who went through transcatheter surgery comprised the Test Group.
High-energy pulsed lasers were used to perform transcatheter laser revascularization in the case of major intracerebral artery lesions; lowenergy continuous lasers equipped with light-guide instruments of small diameters were used to perform transcatheter revascularization in the case of distal intracerebral branches lesions [5,17,18]. If MUGA showed bilateral atherosclerotic changes, transcatheter interventions were performed not only in the area of the developed stroke, but also on the contralateral side [8]. Conservative treatment, including disaggregant, anticoagulant, vasodilating, antioxidant and nootropic therapy, was performed in 341 (39.02%) cases - Control Group.
Test group
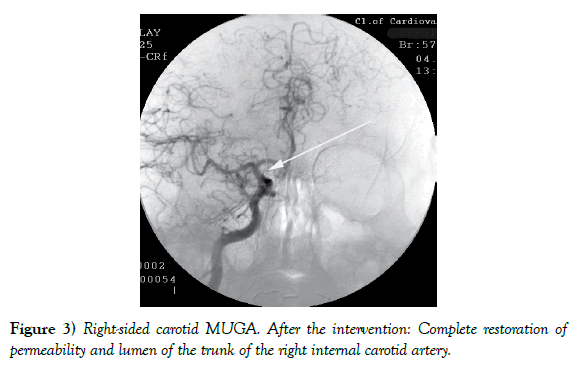
522 (97.94%) patients showed good immediate outcome after the laser surgery, the cause being the restored patency and lumen of the vessels affected, along with collateral revascularization.
12-24 months after the treatment, the results obtained depended on the size of the ischemic lesion and on when the intervention was made after the stroke:
• Good clinical outcome (total recovery of mental and motor functions - IB 90-100) - 323 (60.60%) patients (Table 1);
• Satisfactory clinical outcome (incomplete recovery of mental and motor functions - IB 75-85) - 136 (25.52%) patients (Table 1);
• Relatively satisfactory clinical outcome (partial recovery of mental and motor functions - IB 60-70) - 74 (13.88%) patients (Table 1);
• Relatively positive clinical outcome (absence of negative dynamics with insignificant restoration of mental and motor functions - IB below 60) was not achieved in any case (Table 1).
| Signs | Test Group | Control Group | P (chi-square) |
|---|---|---|---|
| Number of patients | 533 | 341 | |
| Macrofocal strokes (in total): | 81 | 37 | |
| Good clinical outcome | 17 | 0 | |
| Satisfactory clinical outcome | 31 | 0 | p<0.01 |
| Relatively satisfactory clinical outcome | 33 | 6 | |
| Relatively positive clinical outcome | 0 | 31 | |
| Medium focal strokes (in total): | 167 | 62 | |
| Good clinical outcome | 55 | 0 | |
| Satisfactory clinical outcome | 76 | 12 | p<0.01 |
| Relatively satisfactory clinical outcome | 36 | 15 | |
| Relatively positive clinical outcome | 0 | 35 | |
| Microfocal strokes (in total): | 285 | 242 | |
| Good clinical outcome | 251 | 51 | |
| Satisfactory clinical outcome | 29 | 60 | p<0.01 |
| Relatively satisfactory clinical outcome | 5 | 102 | |
| Relatively positive clinical outcome | 0 | 29 |
Using Pearson’s chi-square test, relevant contingency tables were analyzed to identify the differences between the two groups. The p-values achieved are given in the right-hand column of the table. P-value=0.05”.
Table 1: Clinical results of the treatment.
There were neither complications nor negative dynamics observed in any case after the treatment.
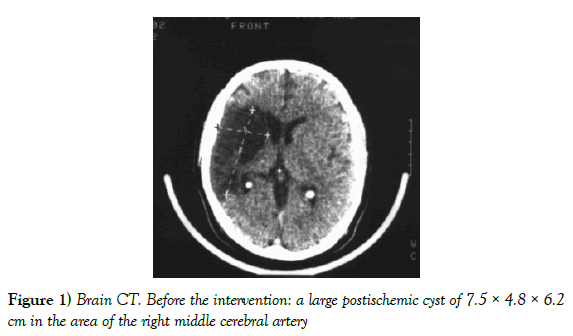
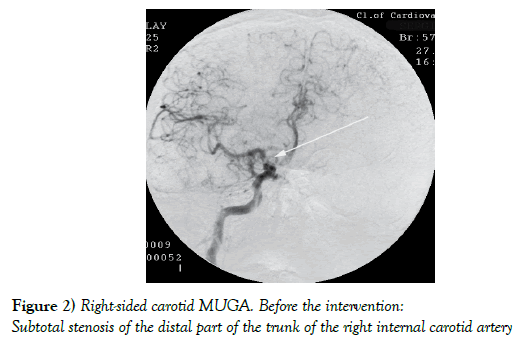
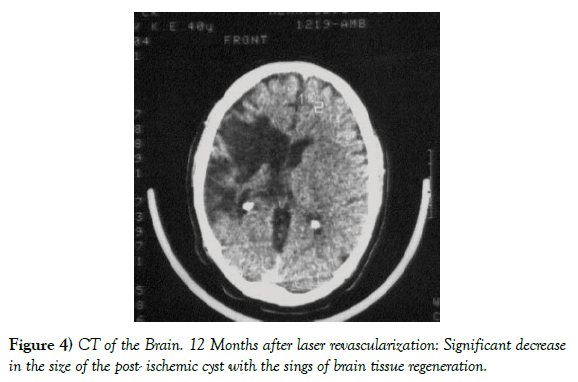
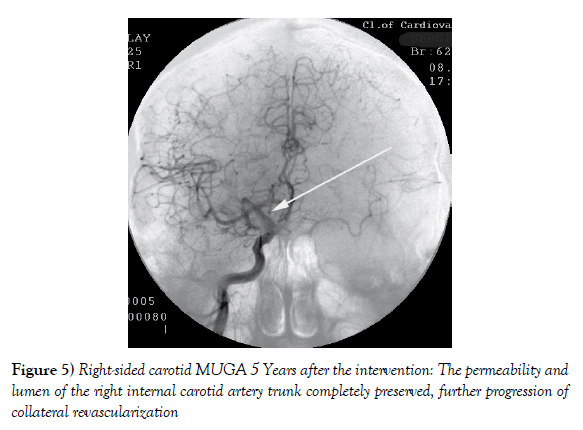
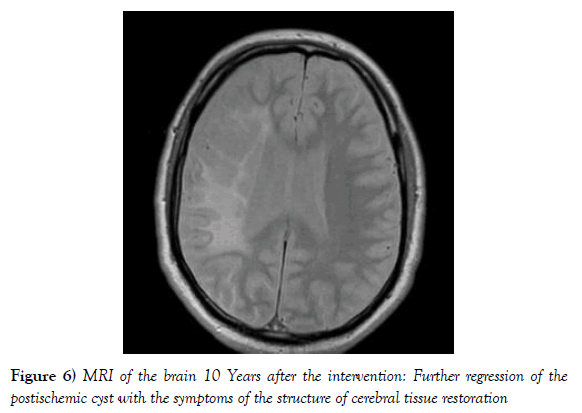
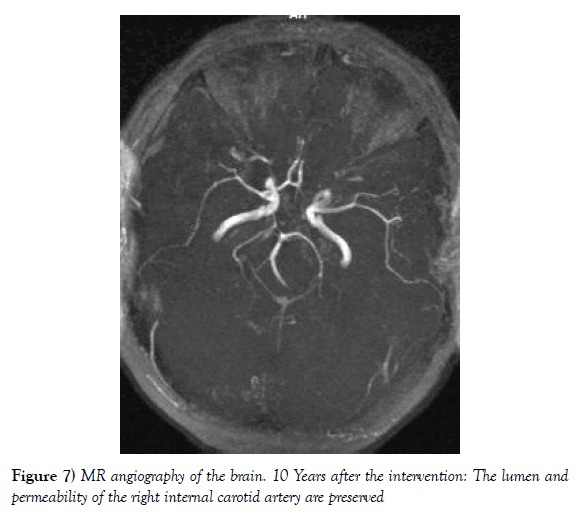
Example: Patient S., man, aged 57, massive stroke in the right hemisphere which resulted in marked left-sided hemiparesis and incomplete sensorymotor aphasia. 12 months after the stroke: dementia severity - CDR-3, daily living activities level - 40 IB points (Figures 1-7).
Figure 1) Brain CT. Before the intervention: a large postischemic cyst of 7.5 × 4.8 × 6.2 cm in the area of the right middle cerebral artery
Figure 2) Right-sided carotid MUGA. Before the intervention: Subtotal stenosis of the distal part of the trunk of the right internal carotid artery
Figure 4) CT of the Brain. 12 Months after laser revascularization: Significant decrease in the size of the post- ischemic cyst with the sings of brain tissue regeneration.
Figure 6) MRI of the brain 10 Years after the intervention: Further regression of the postischemic cyst with the symptoms of the structure of cerebral tissue restoration
Figure 7) MR angiography of the brain. 10 Years after the intervention: The lumen and permeability of the right internal carotid artery are preserved
Twelve months after transcatheter laser revascularization, there was pronounced positive dynamics, no left-sided hemiparesis and incomplete sensory-motor aphasia, no signs of dementia, MMSE-28 points, IB-100 points. In the subsequent observation period (5 and 10 years) the condition is stable, there are no signs of dementia, MMSE - 28 points, IB-100 points.
Control group
• Good clinical outcome was obtained in 51 (21.07%) patients (Table 1).
• Satisfactory clinical outcome was obtained in 72 (21.11%) patients (Table 1).
• Relatively satisfactory clinical outcome was obtained in 123 (36.07%) patients (Table 1).
• Relatively positive clinical outcome was obtained in 95 (27.86%) patients (Table 1).
Discussion
To identify the causes of the stroke, it is necessary to investigate both the extracranial and intracranial basins, as well as assess the condition of collateral and capillary beds [8,10,11]. Intracranial and mixed types of atherosclerotic lesion occur in the vast majority of cases [5].
Along with progression of microfocal or medium focal ischemic strokes, the severity of mental and motor disorders does not always depend on the size of the main ischemic focus. It is often linked to stroke localization, ischemia duration and atherosclerotic lesions extensiveness, both in the area of the stroke and in other arterial basins, which in some cases requires bilateral transcatheter intervention [5,8].
In the case of macrofocal ischemic strokes, various parts of the brain are included in the lesion zone, which leads to pronounced neurologic deficit and neurodegenerative processes [4,5,6,11]. In the situation of this kind, conservative treatment is not effective enough to restore cerebral hemodynamics. The resulting clinical effect is due to partial improvement in cerebral metabolic processes, but this is not sufficient for the functional recovery of cerebral tissue [14,17].
When deciding whether to apply this or that method of treatment, it is necessary to consider the severity of the patient’s somatic and neurological state and the effectiveness of the chosen method [4,8,13].
Transcatheter laser treatment allows the restoration of cerebral blood flow and, by stimulating natural angiogenesis, the improvement of collateral and capillary blood supply in the ischemic region and surrounding tissues [5]. Simultaneously, laser energy, penetrating into the surrounding cerebral tissues, stimulates regenerative processes in them [8,18]. It is supported by the data of plenty of authors conducting experimental and clinical research aimed at transcranial laser effects in ischemic strokes and dementia [19-21].
Conclusion
When treating the consequences of ischemic stroke with predominant intracerebral atherosclerotic lesion, transcatheter laser revascularization is much more effective than conservative treatment. The method helps to restore the cerebral blood supply; it is low-traumatic, does not require distal protection and is easily endured by patients. When intracerebral blood flow is restored and metabolic processes in neurons are stimulated, it reduces the level of mental, cognitive, and motor disorders and quickly brings patients back to their active daily life. The obtained result remains stable for a long time.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/ or publication of this article.
REFERENCES
- Gillum RF, Kwagyan J, Obisesan, et al. Ethnic and Geographic Variation in Stroke Mortality Trends. Stroke. 2011;42(2):3294-6.
- Crozier S. Withdrawing and withholding treatments in acute severe stroke patients in the elderly. Rev Prat. 2012; 62(9):1243-5.
- Pendlebury ST, Wadling S, Silver LE, et al. Transient Cognitive Impairment in TIA and Minor Stroke. Stroke. 2011;42:3116-21.
- Pasi M, Poggesi A, Salvadori E, et al. Post-stroke dementia and cognitive impairment. Front Neurol Neurosci. 2012;30:65-9.
- Maksimovich IV. Transcatheter Treatment of Atherosclerotic Lesions of the Brain Complicated by Vascular Dementia Development. World J of Neurosci. 2012;2(4):200-9.
- Abou-Chebl A. Management of acute ischemic stroke. Curr Cardiol Rep. 2013;15(4):348-54.
- Polak JF, Pencina MJ, O'Leary DH, et al. Common carotid artery intima-media thickness progression as a predictor of stroke in multi-ethnic study of atherosclerosis. Stroke. 2011;42(11):3017-21.
- Maksimovich IV. Transcatheter Cerebral Revascularization in the Treatment of Atherosclerotic Lesions of the Brain. Brain Disorders & Therapy. 2016;5(1):1-8.
- Zhulev NM, Pustozertsev VG, Zhulev SN. Cerebrovascular Diseases. Moscow, BINOM. 2002.
- Liebeskind DS. Collaterals in acute stroke: beyond the clot. Neuroimaging Clin N Am. 2005;15(3):553–73.
- Frölich AM, Psychogios NM, Klotz E, et al. Angiographic Reconstructions From Whole-Brain Perfusion CT for the Detection of Large Vessel Occlusion in Acute Stroke. Stroke. 2012;43(1):97-102.
- Liu R, Yuan H, Yuan F, et al. Neuroprotection targeting ischemic penumbra and beyond for the treatment of ischemic stroke. J Neurology Research. 2012;34:331-7.
- Takaiwa A, Kuwayama N, Akioka N, et. al. Effect of carotid endarterectomy on cognitive function in patients with asymptomatic carotid artery stenosis. Acta Neurochirurgica. 2013;155(4):627-33.
- Silver FL, Mackey A, Clark WM, et al. Safety of stenting and endarterectomy by symptomatic status in the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST). Stroke. 2011;42:675- 80.
- Papanagiotou P, Roth C, Walter S, et al. Carotid artery stenting in acute stroke. J Am Coll Cardiol. 2011;58(23):2363-9.
- Rohde S, Seckinger J, Hähnel C, et al. Stent design lowers angiographic but not clinical adverse events in stenting of symptomatic intracranial stenosis–results of a single center study with 100 consecutive patients. Int J Stroke. 2013;8(2):87-94.
- Maksimovich IV. Method for Carrying out Transluminal Laser-Induced Brain Revascularization in Atherosclerotic Injury Cases. Patent RU. 2006.
- Maksimovich IV. Method of Transluminal Laser Revascularization of Cerebral Blood Vessels Having Atherosclerotic Lesions. Patent US. 2008.
- Hashmi JT, Huang YY, Osmani BZ, et al. Role of Low-Level Laser Therapy in Neurorehabilitation. PM&R. 2010; 2(2):S292–305.
- Song S, Zhou F, Chen WR. Low-level laser therapy regulates microglial function through Src-mediated signaling pathways: implications for neurodegenerative diseases. J Neuroinflammation. 2012;18(9):219.
- Naeser MA, Hamblin MR. Potential for transcraniallaser or LED therapy to treatstroke, traumatic brain injury, and neurodegenerative disease. Photomed Laser Surg. 2011;29(7):443-46.