Retropancreatic Extension of Teratomas: Case Report
Received: 01-Aug-2022, Manuscript No. ijav-22-5262; Editor assigned: 04-Aug-2022, Pre QC No. ijav-22-5262 (PQ); Accepted Date: Aug 22, 2022; Reviewed: 18-Aug-2022 QC No. ijav-22-5262; Revised: 22-Aug-2022, Manuscript No. ijav-22-5262 (R); Published: 29-Aug-2022, DOI: 10.37532/1308-4038.15(8).212
Citation: Karl M. Retropancreatic Extension of Teratomas: Case Report. Int J Anat Var. 2022;15(8):209-209.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The conferred paper focuses on surgical anatomy of this terribly rare sort of growth. Teratomas were settled in the main inside the higher bodily cavity, and each tumor displaced the duct gland in an anterior position. The anatomical options that were ascertained area unit displacement of encompassing organs, and deformation and elongation of enormous retroperitoneal vessels.
Keywords
Surgical Anatomy; Teratomas; Infants; Report
INTRODUCTION
Teratoma is Associate in nursing embryonic growth derived from tot potential cells that contain tissue from a minimum of 2 or a lot of typically 3 germ layers in variable proportions. It should contain mature and immature tissue parts furthermore as malignant parts. Retroperitoneal tumor is extremely rare, and it happens in barely 3%–5% of teratomas. Despite the supply of advanced imaging techniques the medical specialty doctor ought to have in mind the expected anatomy of this kind of tumour. In an exceedingly pioneer study retroperitoneal teratomas beside different sorts of tumors were represented as “unattached retroperitoneal tumors”. The aim of our study was to elaborate data regarding the expansion pattern and surgical anatomy of this kind of growth. Moreover, anatomical relationship to the duct gland was noted.
CASE REPORT
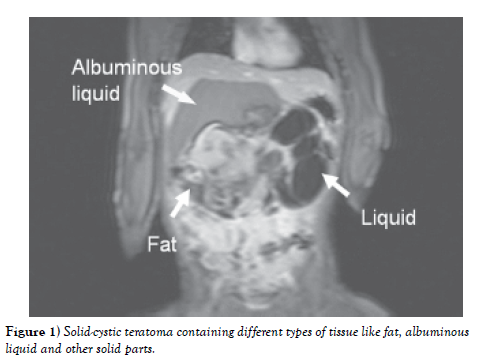
The twelve-month-old woman was brought up our hospital with an outsized abdominal protrusion. There was neither any craving loss nor expulsion. On physical examination a mass of twenty cm in diameter was palpable among the full higher abdomen. Liquid body substance alpha fetoprotein level (22ng/ml) was at the higher border of the age connected confidence interval. Ultrasound confirmed the presence of an outsized heterogeneous abdominal mass. Magnet Resonance Imaging (MRI) unconcealed a fat containing, solid and cystic retroperitoneal tumour with broad contact to the massive vessels (Figure 1).
right suprarenal region. As a consequence, the exocrine gland was found before of the tumour of each case. Retro pancreatic extension could be a well-known feature of adrenal malignant neoplasm and left sided sarcoma. In concern with tumour it’s been delineated often in previous papers. For medical diagnosis mature tumour of exocrine gland and also the endocrine gland has been rumored. However, there have been clear surgical plains between the exocrine gland and also the tumour. Moreover, adrenal tissue wasn’t found in any of each tumors delineated during this paper. The retropancreatic extension of tumour will be explained by the sex cell theory. Throughout early embryonic development totipotential germ cells migrate from their traditional origin within the nutrient sac on the posterior peritoneum of the viscus to the endocrine gland ridge then to the endocrine gland.
CONCLUSION
Incomplete or inaccurate embryonic reproductive cell migration may occur and may be the origin of the neoplasm. The outline of retroperitoneal neoplasm as “unattached retroperitoneal tumor” anatomical relationships of high complexness has got to been taken into consideration if surgery is performed.
ACKNOWLEDGEMENT: None.
CONFLICTS OF INTEREST: None.
REFERENCES
- Gobel U, Calaminus G, Blohm M. Extracranial non-testicular teratoma in childhood and adolescence: introduction of a risk score for stratification of therapy. Klin Pädiatr. 1997; 209(4):228-234.
- Bruneton JN, Diard F, Drouillard JP. Primary retroperitoneal teratoma in adults: Presentation of two cases and review of literature. Radiology. 1980; 134(3):613-616.
- Gatcombe HG, Assikis V, Kooby D. Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol. 2004; 86(2):107-113.
- Hansmann GH, Budd JW. Massive Unattached Retroperitoneal Tumors: An Explanation of Unattached Retroperitonel Tumors Based on Remnants of the Embryonic Urogenital Apparatus. Am J Pathol. 1931; 7(6):631-674.
- Davidson AJ, Hartman DS, Goldman SM. Mature teratoma of the retroperitoneum: radiologic, pathologic, and clinical correlation. Radiology. 1989; 172(2):421-425.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref