Reversed palmaris profundus muscle variation
Björn-Ole Bast, Merle Winkler, Bodo Kurz*
Anatomisches Institut, Christian-Albrechts-Universität, Kiel, Germany.
- *Corresponding Author:
- Prof. Dr. Bodo Kurz
Anatomisches Institut, CAU zu Kiel, Olshausenstrasse 40-60, 24098 Kiel, Germany.
Tel: +49 (431) 880-3080
E-mail: sujan.ganapathy@gmail.com
Date of Received: March 18th, 2015
Date of Accepted: September 22nd, 2015
Published Online: August 8th, 2016
© Int J Anat Var (IJAV). 2016; 9: 21–24.
[ft_below_content] =>Keywords
palmaris profundus, reversed, carpal tunnel syndrome, muscles of the forearm, anatomical variation
Introduction
Anatomical variations are very common, especially the ones of the muscles in the forearm. Thereby the palmaris longus muscle is probably the most variable muscle in the human body [1]. The palmaris profundus muscle is a rare, but also known variation which originally has been described as a special type of variation of the palmaris longus muscle. However, several reports indicate that the palmaris profundus can coexist with a palmaris longus [2–4] and it is now seen as an independent or “accessory” muscle [5], generally inserting into the palmar aponeurosis, which leads to the term “palmaris”. Furthermore it is not located as superficial as the palmaris longus muscle, which reveals the byname “profundus”. So in general the palmaris profundus muscle is a deep located accessory muscle of the forearm inserting into the palmar aponeurosis, which usually coexists with the palmaris longus muscle.
The palmaris profundus in man has first been described by Frohse and Fränkel [6] and is found in one of 530 cadaveric limbs [7] or in one of 526 carpal tunnel syndrome surgeries [8]. Pirola et al. [5] suggested that palmaris profundus-related compression at the wrist can be directly attributed to the trajectory of the palmaris profundus tendon rather than to the resultant decreased available space for the median nerve due to an additional tendon within the carpal tunnel, generally thought to be the mechanism of compression. However, a reduced space alone should also increase the risk of carpal tunnel syndrome formation.
In the course of this paper we picture a case of a reverse palmaris profundus muscle with a fleshy muscle belly in the distal forearm and a long proximal tendon, which has been reported only once so far, but with a different origin and insertion [9]. This muscle does not match any of the already described subtypes based on the cases found in the literature.
Case Report
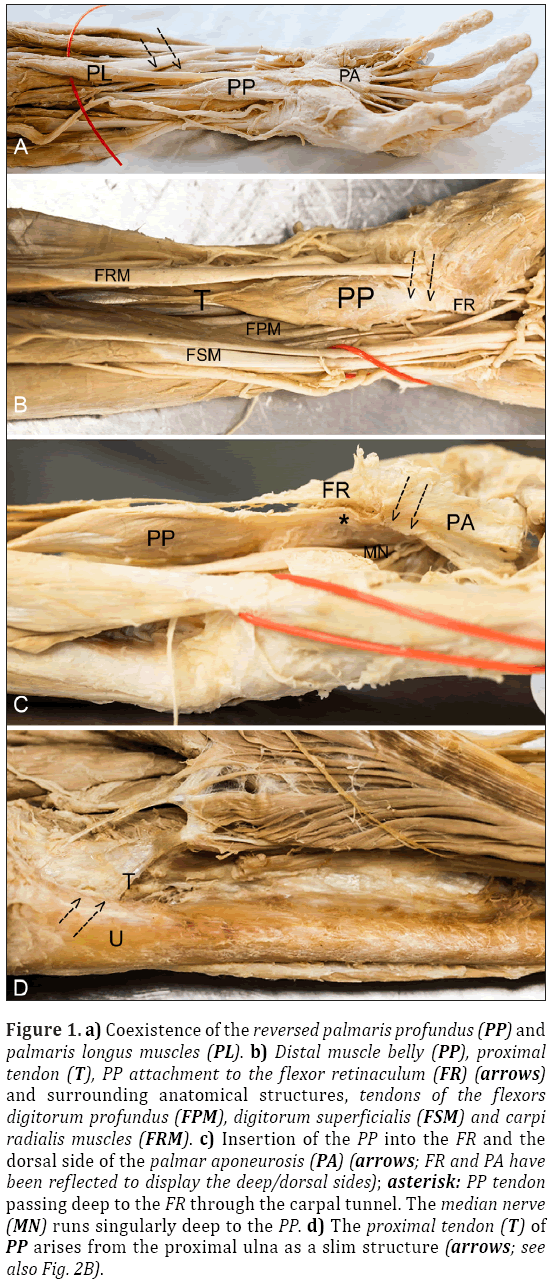
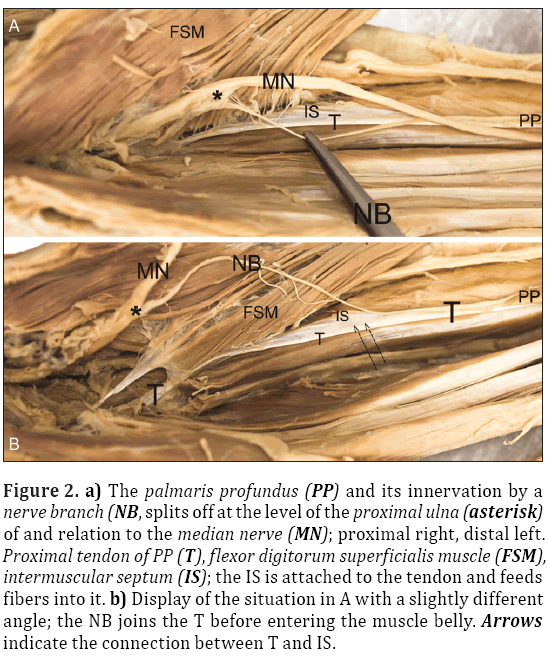
During the regular dissection course for medical students, which comes into existence in cooperation with the voluntary and non-profit body donation program of the University of Kiel, a new muscle variation was found in the left forearm of an adult, Caucasian, male cadaver, aged 89 years. Examination of the upper extremities showed a typical flexor digitorum superficialis and profundus, flexor carpi radialis and ulnaris, pronator teres and palmaris longus muscle on both sides. On the left side, however, an additional muscle was detected, with a fleshy muscle belly in the distal portion of the forearm, near to the flexor retinaculum, which measured 7.5 cm in length, 2 cm in width and was 0.6 cm thick. It was located between the tendons of the flexor digitorum superficialis and flexor digitorum profundus muscle and showed a long proximal tendon running down from the origin of the muscle at the ulna (Figure 1). The tendon measured 13.5 cm in length and originated at the proximal volar side of the ulna shaft and received additional collagen fibers from the intermuscular septum during its course (Figure 2). Distally the muscle belly formed a sliver that fed a part of its fibers to the flexor retinaculum on the radial side of the forearm. However, the main portion of its fibers passed through the carpal tunnel and inserted into the palmar aponeurosis from the deep side (Figure 1).
Figure 1: a) Coexistence of the reversed palmaris profundus (PP) and palmaris longus muscles (PL). b) Distal muscle belly (PP), proximal tendon (T), PP attachment to the flexor retinaculum (FR) (arrows) and surrounding anatomical structures, tendons of the flexors digitorum profundus (FPM), digitorum superficialis (FSM) and carpi radialis muscles (FRM). c) Insertion of the PP into the FR and the dorsal side of the palmar aponeurosis (PA) (arrows; FR and PA have been reflected to display the deep/dorsal sides); asterisk: PP tendon passing deep to the FR through the carpal tunnel. The median nerve (MN) runs singularly deep to the PP. d) The proximal tendon (T) of PP arises from the proximal ulna as a slim structure (arrows; see also Fig. 2B).
Figure 2: a) The palmaris profundus (PP) and its innervation by a nerve branch (NB, splits off at the level of the proximal ulna (asterisk) of and relation to the median nerve (MN); proximal right, distal left. Proximal tendon of PP (T), flexor digitorum superficialis muscle (FSM), intermuscular septum (IS); the IS is attached to the tendon and feeds fibers into it. b) Display of the situation in A with a slightly different angle; the NB joins the T before entering the muscle belly. Arrows indicate the connection between T and IS.
The median nerve was running separately and did not share a fascial sheath with the tendon, as previously reported by Sahinoglu et al. [9]. A thick nerve branch split off the median nerve instead, at the level of the elbow, and innervated the muscle (Figure 2). The median nerve itself followed its normal anatomical course, while the additional nerve branch joined the proximal tendon, running with it enclosed in a single fascial sheath until it inserted proximally into the muscle belly.
Discussion
The palmaris profundus is a very rare muscle, which is variable in its insertion, but especially variable in its origin. The muscle can either insert into the palmar aponeurosis, the flexor retinaculum or both with singular or multiple attachments, as the literature shows [5,9–11]. Most of the case reports describe a palmaris profundus muscle with a proximal muscle belly and a distal tendon or a centered muscle belly in between a proximal and distal tendon [5,6,10,11]. The muscle belly in our case was located distally close to the carpal tunnel, which classifies the muscle as a reversed version, which has been mentioned only once so far by Sahinoglu et al. [9]. The authors described a muscle with a belly arising from beneath the transverse carpal ligament and a reversed insertion into the common flexor tendon. Because of the fact, that the muscle was inversed they defined the carpal ligament as origin and the common flexor tendon as insertion. However, in this case report we decided to define the proximal muscle attachment as origin and the distal attachments as insertion. Our new muscle finding indicates that a reversed version of the palmaris profundus is not a unique pattern and might therefore be considered as another feature for the existing classification of palmaris profundus subtypes and might lead to a refinement of the said by Yoshida et al. [10].
As mentioned above there have been several reports showing a common course of the median nerve and the palmaris profundus tendon and several studies even demonstrated that this rare muscle variation can be encased in a common fascial sheath with the median nerve. An existence of a common sheath results in closer relationship of the two different structures and therefore increases the risk of median nerve irritation even more. In our case the palmaris profundus did not share a common sheath with the median nerve. Especially its long proximal tendon was separated from it, but in close relation to the median nerve (Figure 1). Due to the unknown medical history of the body donor it is impossible to tell if the person suffered from median nerve compression.
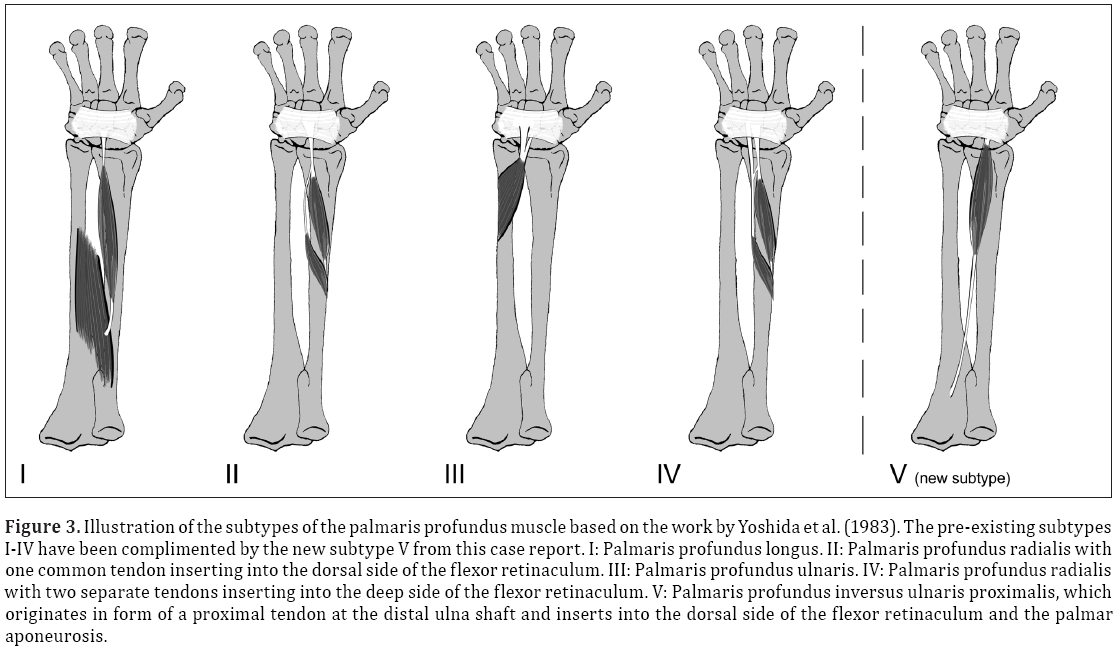
The reversed structure of the muscle and its attachment to the proximal ulnar shaft shows that there are more variants in origin, insertion, course, and relation to the median nerve than there are described so far (Figure 3). Furthermore it shows that there are still undiscovered variations of the palmaris profundus muscle a surgeon may come across during surgery of the forearm.
Figure 3: Illustration of the subtypes of the palmaris profundus muscle based on the work by Yoshida et al. (1983). The pre-existing subtypes I-IV have been complimented by the new subtype V from this case report. I: Palmaris profundus longus. II: Palmaris profundus radialis with one common tendon inserting into the dorsal side of the flexor retinaculum. III: Palmaris profundus ulnaris. IV: Palmaris profundus radialis with two separate tendons inserting into the deep side of the flexor retinaculum. V: Palmaris profundus inversus ulnaris proximalis, which originates in form of a proximal tendon at the distal ulna shaft and inserts into the dorsal side of the flexor retinaculum and the palmar aponeurosis.
Acknowledgement
Our thanks to the body donors of the voluntary and nonprofit body donation program at CAU Kiel for their invaluable contribution and to Stefanie Gundlach, Thomas Benecke and Arndt Gundlach for their excellent technical assistance in the gross anatomy lab.
References
- Bergman RA, Thompson SA, Afifi AK. Catalog of Human Variation. Baltimore & Munich: Urban & Schwarzenberg. 1984; 31–33.
- Dyreby JR, Engber WD. Palmaris profundus – rare anomalous muscle. J Hand Surg Am. 1982; 7: 513–514.
- Fatah MF. Palmaris profundus of Frohse and Fränkel in association with carpal tunnel syndrome. J Hand Surg Br. 1982; 9: 142–144.
- Floyd T, Burger RS, Sciaroni CA. Bilateral palmaris profundus causing bilateral carpal tunnel syndrome. J Hand Surg Am. 1990; 15: 364–366.
- Pirola E, Hébert-Blouin MN, Amador N, Amrami KK, Spinner RJ. Palmaris profundus: one name, several subtypes, and a shared potential for nerve compression. Clin Anat. 2009; 22: 643–648.
- Frohse F, Fränkel M. Die Muskeln des Menschlichen Armes, Handbuch der Anatomie des Menschen. Munich & Jena, Gustav Fischer. 1908; 115–118. (German)
- Reimann AF, Daseler EH, Anson BJ, Beaton LE. The palmaris longus muscle and tendon: A study of 1600 extremities. Anat Rec. 1944; 89: 495–505.
- Lindley SG, Kleinert JM. Prevalence of anatomic variations encountered in elective carpal tunnel release. J Hand Surg Am. 2003; 28: 849–855.
- Sahinoglu K, Cassell MD, Miyauchi R, Bergman RA. Musculus comitans nervi mediani (M. Palmaris profundus). Ann Anat. 1994; 176: 229–232.
- Yoshida Y, Yasutaka S, Seki Y. Flexor radialis profundus and palmaris profundus muscles in man. Kaibogaku Zasshi. 1983; 58: 59–67. (Japanese)
- Wisco JJ, Dell MM, Stark ME. A variation of the palmaris profundus muscle. Int J Anat Var (IJAV). 2010; 3: 36–38.
Björn-Ole Bast, Merle Winkler, Bodo Kurz*
Anatomisches Institut, Christian-Albrechts-Universität, Kiel, Germany.
- *Corresponding Author:
- Prof. Dr. Bodo Kurz
Anatomisches Institut, CAU zu Kiel, Olshausenstrasse 40-60, 24098 Kiel, Germany.
Tel: +49 (431) 880-3080
E-mail: sujan.ganapathy@gmail.com
Date of Received: March 18th, 2015
Date of Accepted: September 22nd, 2015
Published Online: August 8th, 2016
© Int J Anat Var (IJAV). 2016; 9: 21–24.
Abstract
The palmaris profundus is a variant muscle in the forearm which might lead to carpal tunnel syndrome. Due to its variable origins, courses and insertions, it has been classified into subtypes previously, and its often very close relation to the median nerve has been highlighted. Dissection of a male cadaver now uncovered a new reversed variant of this muscle which does not match any of the already described subtypes because of its unique origin from the proximal ulnar shaft and its less pronounced spatial relation to the median nerve. This case shows that there are still unknown variations, which a surgeon may come across during carpal tunnel surgery or any other surgery of the forearm and which may lead to median nerve compression.
-Keywords
palmaris profundus, reversed, carpal tunnel syndrome, muscles of the forearm, anatomical variation
Introduction
Anatomical variations are very common, especially the ones of the muscles in the forearm. Thereby the palmaris longus muscle is probably the most variable muscle in the human body [1]. The palmaris profundus muscle is a rare, but also known variation which originally has been described as a special type of variation of the palmaris longus muscle. However, several reports indicate that the palmaris profundus can coexist with a palmaris longus [2–4] and it is now seen as an independent or “accessory” muscle [5], generally inserting into the palmar aponeurosis, which leads to the term “palmaris”. Furthermore it is not located as superficial as the palmaris longus muscle, which reveals the byname “profundus”. So in general the palmaris profundus muscle is a deep located accessory muscle of the forearm inserting into the palmar aponeurosis, which usually coexists with the palmaris longus muscle.
The palmaris profundus in man has first been described by Frohse and Fränkel [6] and is found in one of 530 cadaveric limbs [7] or in one of 526 carpal tunnel syndrome surgeries [8]. Pirola et al. [5] suggested that palmaris profundus-related compression at the wrist can be directly attributed to the trajectory of the palmaris profundus tendon rather than to the resultant decreased available space for the median nerve due to an additional tendon within the carpal tunnel, generally thought to be the mechanism of compression. However, a reduced space alone should also increase the risk of carpal tunnel syndrome formation.
In the course of this paper we picture a case of a reverse palmaris profundus muscle with a fleshy muscle belly in the distal forearm and a long proximal tendon, which has been reported only once so far, but with a different origin and insertion [9]. This muscle does not match any of the already described subtypes based on the cases found in the literature.
Case Report
During the regular dissection course for medical students, which comes into existence in cooperation with the voluntary and non-profit body donation program of the University of Kiel, a new muscle variation was found in the left forearm of an adult, Caucasian, male cadaver, aged 89 years. Examination of the upper extremities showed a typical flexor digitorum superficialis and profundus, flexor carpi radialis and ulnaris, pronator teres and palmaris longus muscle on both sides. On the left side, however, an additional muscle was detected, with a fleshy muscle belly in the distal portion of the forearm, near to the flexor retinaculum, which measured 7.5 cm in length, 2 cm in width and was 0.6 cm thick. It was located between the tendons of the flexor digitorum superficialis and flexor digitorum profundus muscle and showed a long proximal tendon running down from the origin of the muscle at the ulna (Figure 1). The tendon measured 13.5 cm in length and originated at the proximal volar side of the ulna shaft and received additional collagen fibers from the intermuscular septum during its course (Figure 2). Distally the muscle belly formed a sliver that fed a part of its fibers to the flexor retinaculum on the radial side of the forearm. However, the main portion of its fibers passed through the carpal tunnel and inserted into the palmar aponeurosis from the deep side (Figure 1).
Figure 1: a) Coexistence of the reversed palmaris profundus (PP) and palmaris longus muscles (PL). b) Distal muscle belly (PP), proximal tendon (T), PP attachment to the flexor retinaculum (FR) (arrows) and surrounding anatomical structures, tendons of the flexors digitorum profundus (FPM), digitorum superficialis (FSM) and carpi radialis muscles (FRM). c) Insertion of the PP into the FR and the dorsal side of the palmar aponeurosis (PA) (arrows; FR and PA have been reflected to display the deep/dorsal sides); asterisk: PP tendon passing deep to the FR through the carpal tunnel. The median nerve (MN) runs singularly deep to the PP. d) The proximal tendon (T) of PP arises from the proximal ulna as a slim structure (arrows; see also Fig. 2B).
Figure 2: a) The palmaris profundus (PP) and its innervation by a nerve branch (NB, splits off at the level of the proximal ulna (asterisk) of and relation to the median nerve (MN); proximal right, distal left. Proximal tendon of PP (T), flexor digitorum superficialis muscle (FSM), intermuscular septum (IS); the IS is attached to the tendon and feeds fibers into it. b) Display of the situation in A with a slightly different angle; the NB joins the T before entering the muscle belly. Arrows indicate the connection between T and IS.
The median nerve was running separately and did not share a fascial sheath with the tendon, as previously reported by Sahinoglu et al. [9]. A thick nerve branch split off the median nerve instead, at the level of the elbow, and innervated the muscle (Figure 2). The median nerve itself followed its normal anatomical course, while the additional nerve branch joined the proximal tendon, running with it enclosed in a single fascial sheath until it inserted proximally into the muscle belly.
Discussion
The palmaris profundus is a very rare muscle, which is variable in its insertion, but especially variable in its origin. The muscle can either insert into the palmar aponeurosis, the flexor retinaculum or both with singular or multiple attachments, as the literature shows [5,9–11]. Most of the case reports describe a palmaris profundus muscle with a proximal muscle belly and a distal tendon or a centered muscle belly in between a proximal and distal tendon [5,6,10,11]. The muscle belly in our case was located distally close to the carpal tunnel, which classifies the muscle as a reversed version, which has been mentioned only once so far by Sahinoglu et al. [9]. The authors described a muscle with a belly arising from beneath the transverse carpal ligament and a reversed insertion into the common flexor tendon. Because of the fact, that the muscle was inversed they defined the carpal ligament as origin and the common flexor tendon as insertion. However, in this case report we decided to define the proximal muscle attachment as origin and the distal attachments as insertion. Our new muscle finding indicates that a reversed version of the palmaris profundus is not a unique pattern and might therefore be considered as another feature for the existing classification of palmaris profundus subtypes and might lead to a refinement of the said by Yoshida et al. [10].
As mentioned above there have been several reports showing a common course of the median nerve and the palmaris profundus tendon and several studies even demonstrated that this rare muscle variation can be encased in a common fascial sheath with the median nerve. An existence of a common sheath results in closer relationship of the two different structures and therefore increases the risk of median nerve irritation even more. In our case the palmaris profundus did not share a common sheath with the median nerve. Especially its long proximal tendon was separated from it, but in close relation to the median nerve (Figure 1). Due to the unknown medical history of the body donor it is impossible to tell if the person suffered from median nerve compression.
The reversed structure of the muscle and its attachment to the proximal ulnar shaft shows that there are more variants in origin, insertion, course, and relation to the median nerve than there are described so far (Figure 3). Furthermore it shows that there are still undiscovered variations of the palmaris profundus muscle a surgeon may come across during surgery of the forearm.
Figure 3: Illustration of the subtypes of the palmaris profundus muscle based on the work by Yoshida et al. (1983). The pre-existing subtypes I-IV have been complimented by the new subtype V from this case report. I: Palmaris profundus longus. II: Palmaris profundus radialis with one common tendon inserting into the dorsal side of the flexor retinaculum. III: Palmaris profundus ulnaris. IV: Palmaris profundus radialis with two separate tendons inserting into the deep side of the flexor retinaculum. V: Palmaris profundus inversus ulnaris proximalis, which originates in form of a proximal tendon at the distal ulna shaft and inserts into the dorsal side of the flexor retinaculum and the palmar aponeurosis.
Acknowledgement
Our thanks to the body donors of the voluntary and nonprofit body donation program at CAU Kiel for their invaluable contribution and to Stefanie Gundlach, Thomas Benecke and Arndt Gundlach for their excellent technical assistance in the gross anatomy lab.
References
- Bergman RA, Thompson SA, Afifi AK. Catalog of Human Variation. Baltimore & Munich: Urban & Schwarzenberg. 1984; 31–33.
- Dyreby JR, Engber WD. Palmaris profundus – rare anomalous muscle. J Hand Surg Am. 1982; 7: 513–514.
- Fatah MF. Palmaris profundus of Frohse and Fränkel in association with carpal tunnel syndrome. J Hand Surg Br. 1982; 9: 142–144.
- Floyd T, Burger RS, Sciaroni CA. Bilateral palmaris profundus causing bilateral carpal tunnel syndrome. J Hand Surg Am. 1990; 15: 364–366.
- Pirola E, Hébert-Blouin MN, Amador N, Amrami KK, Spinner RJ. Palmaris profundus: one name, several subtypes, and a shared potential for nerve compression. Clin Anat. 2009; 22: 643–648.
- Frohse F, Fränkel M. Die Muskeln des Menschlichen Armes, Handbuch der Anatomie des Menschen. Munich & Jena, Gustav Fischer. 1908; 115–118. (German)
- Reimann AF, Daseler EH, Anson BJ, Beaton LE. The palmaris longus muscle and tendon: A study of 1600 extremities. Anat Rec. 1944; 89: 495–505.
- Lindley SG, Kleinert JM. Prevalence of anatomic variations encountered in elective carpal tunnel release. J Hand Surg Am. 2003; 28: 849–855.
- Sahinoglu K, Cassell MD, Miyauchi R, Bergman RA. Musculus comitans nervi mediani (M. Palmaris profundus). Ann Anat. 1994; 176: 229–232.
- Yoshida Y, Yasutaka S, Seki Y. Flexor radialis profundus and palmaris profundus muscles in man. Kaibogaku Zasshi. 1983; 58: 59–67. (Japanese)
- Wisco JJ, Dell MM, Stark ME. A variation of the palmaris profundus muscle. Int J Anat Var (IJAV). 2010; 3: 36–38.