Side effects of hyperbaric oxygen therapy in children with special needs: A cross-sectional study
Received: 01-Aug-2022, Manuscript No. PULJMC-22-5214; Editor assigned: 03-Aug-2022, Pre QC No. PULJMC-22-5214 (PQ); Reviewed: 17-Aug-2022 QC No. PULJMC-22-5214; Revised: 23-Dec-2022, Manuscript No. PULJMC-22-5214 (R); Published: 03-Jan-2023
Citation: Zayed KM. Side effects of hyperbaric oxygen therapy in children with special needs: A cross-sectional study. J Mol Cancer 2023;6(1):1-8.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Hyperbaric Oxygen Therapy (HBO2 ) is a treatment modality in which a subject breathes 100% O2 under increased atmospheric pressure. It is an important advanced therapy in the treatment of at least fourteen documented ailments. The typically mild and self-limited MEB and ETD are the most common side effects identified in the peer-reviewed literature. Claustrophobia or confinement anxiety in monoplace chambers is another side effect of HBO2 therapy but it is generally mild and anxiety is easily controlled with sedation before treatments so that individuals may continue to receive daily HBO2 therapy. O2 toxicity seizure and temporarily blurred vision due to swelling of the lens and advancing cataracts are other rare complications.
Objective: To identify and study some side effects of hyperbaric oxygen in a group of children with special needs.
Methodology: Data for this study were collected from a sample of purposefully selected 100 (69 male+31 female) patients with special needs (age range: 72-120 months) in a center in Cairo by the use of cases’ parents’ interview form; full medical history, examination, and investigations; some clinical tests such as tympanometry, modified-Teed, and HAM-A scores to quantify MEB, ETD, and anxiety side effects of HBO2 therapy; data analysis and suggestions for future improvement of identification and management of HBO2 therapy side effects.
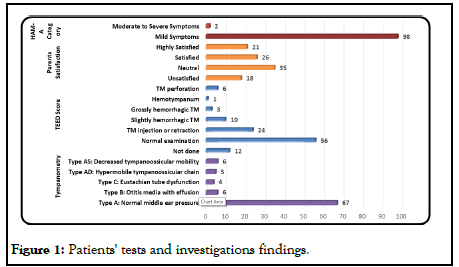
Results: Patients had been treated for 24 months with 2203 sessions of HBO2 therapy and other therapies for LD (38%), CP (36%), ASD (20%), ADHD (4%), and Wounds (2%). For middle ear conditions, tympanometry showed that 78 patients had type A (5 Type AD and 6 Type AS), 6 Type B and 4 Type C. M-Teed score showed that 56% had grade 0, 24% grade 1, 10% grade 2, 3% grade 3, 1% grade 4, and 6% grade 5. For claustrophobia, the Anxiety Severity HAM-A score showed that only 2% had moderate to severe symptoms. None showed any O2 toxicity, pulmonary complications, relevant ophthalmological side effects or complications, or dental complaints.
Conclusion: Even though there are a few contraindications and side effects associated with it, HBO2 therapy remains among the safest therapies used today; especially, in the pediatric population with special needs. It is both its primary and secondary effects that result in its benefits as well as side effects. Despite being infrequent and mild, providers need to be able to identify, understand, and quantify potential side effects such as MEB, ETD, and claustrophobia for prevention, management, and informed consent. Patient instruction on middle ear clearing, daily monitoring with an otoscopic examination, and appropriate compression rates are important to MEB and ETD prevention. Preventive measures with adequate patient history, patient education, reassurance, and coaching are the most effective means of anticipating episodes of claustrophobia and treating them effectively before HBO2 therapy
Keywords
Hyperbaric oxygen therapy; HBO2 therapy; Pediatrics; Side effects; Special needs; Middle ear barotrauma Eustachian tube dysfunction; Tympanometry; Modified teed score; Hamilton anxiety score
Introduction
Hyperbaric Oxygen(HBO2) therapy is a treatment modality in which a subject breathes 100% O2 under increased atmospheric pressure, typically 2-3 Atmospheres Absolute (ATA) (i.e. the sum of the atmospheric pressure (1 ATA) plus extra hydrostatic pressure equal to one or two atmospheres). Treatments are done in either a mono (single person) or multiplace (usually 2 to 14 patients) chamber [1]. Its primary and secondary effects can cause beneficial, as well as side effects. Although HBO2 therapy was not studied in medical school curricula and had no pharmaceutical companies to support it, HBO2 is now commonly and promptly gaining acceptance due to numerous reasons including its safety as a remedy with rare and minor documented side effects, its addition obviates the need for several surgical procedures and promotes healing and early mobility of patients, reduction of hospitalization length, treatment, and costs of rehabilitation, being the only treatment available in some situations and it has an emergent role in indications for permanent disabilities [2].
According to indication, HBO2 treatments may last 1.5 to 8 hours and may be performed 1-3 times a day. The monoplace chambers are customarily compressed with pure O2, while multiplace chambers are pressurized with air where subjects can breathe pure O2 through a tight-fitting face mask, a head tent, or an endotracheal tube. During treatment, the arterial O2 tension frequently exceeds 2000 mmHg and tissue levels of 200 mmHg-400 mmHg can result [1]. At normal atmospheric pressure, O2 transport is limited by the O2 binding capacity to the RBCs’ hemoglobin while a little O2 is transported by blood plasma. Hypoxia is a substantial component of the pathology of stroke, cancer, heart disease, and chronic lung disease accounting for almost 60% of the total number of deaths because hypoxia leads to metabolic acidosis, organ dysfunction, and death through a series of adverse problems, such as localized vasodilation, pulmonary vasoconstriction, metabolic acidosis, tissue necrosis, an increased risk of kernicterus, brain injury, and impairment of surfactant production, especially in the pediatric population [3,4].
The healing principle of HBO2 therapy lies in its capacity to significantly increase the partial pressure of O2 in the body tissues; O2 transport by plasma significantly increases using HBO2 therapy because of O2’s higher solubility with increasing pressure following Henry’s law rather than the RBCs’ hemoglobin where the route of transport cannot be utilized any further being almost saturated with O2 at 1 atmospheric pressure [5]. HBO2 therapy curative effects are dependent on both hydrostatic pressure and the partial pressure of O2 as an elevation of the hydrostatic pressure causes a reduction in the gas volume according to Boyle's law [6]. This action directly relates to pathologic conditions in which gas bubbles are present in the body like arterial gas embolism and decompression sickness [7].
The results of HBO2 therapy include both primary and secondary effects. The primary effects cause increased pressure and hyperoxia while the secondary effects (resulting from controlled oxidative stress) include antimicrobial ischemia-reperfusion injuries blunting, and wound healing a result of both local and systemic effects. Again, the local effects include a steepened O2 gradient, macrophage pooling, and multiple growth factors release while the systemic effects result in progenitor stem cell mobilization and release from bone marrow in addition to enhanced homing to the injury’s site by these cells, by a nitrous oxide (•NO) dependent mechanism.
These effects can result in neovasculogenesis and collagen formation that promote wound healing [8]. Recommendations for HBO2 use are given by The Undersea and Hyperbaric Medical Society (UHMS) and the UHMS hyperbaric oxygen therapy committee lists approvals for reimbursement for certain diagnoses in hospitals and clinics [9]. The FDA approved HBO2 therapy for the treatment of many conditions one of which is autism (Table 1).
| A. Universally accepted: These indications are supported with peer-reviewed proof of efficacy. | |
| Primary line of treatment | Air or gas embolism |
| Decompression sickness | |
| CO poisoning, smoke inhalation | |
| CO poisoning complicated by cyanide poisoning | |
| Wounds | Enhancement of healing in selected problem wounds, and ulcers (diabetic, venous, etc) |
| Diabetic disease as in short-term relief of diabetic foot, diabetic retinopathy, diabetic nephropathy , and mucormycosis, e.g. rhinocerebral disease | |
| Infective wounds: Clostridial myositis and myonecrosis (gas gangrene), refractory osteomyelitis necrotizing soft tissue infections (necrotizing fasciitis) | |
| ÃÂ? Acute traumatic ischemias, crush injury, and compartment syndrome | |
| Compromised skin grafts and flaps | |
| Thermal burns | |
| ÃÂ? Exceptional blood loss (anemia) | |
| Occlusion of the central retinal artery | |
| Oncology | Delayed radiation-induced tissue damage and complications due to endarteritis (soft tissue and bony necrosis) |
| Prophylactically adjunctive to therapeutic radiation and for preparation of surgery or implant procedures in previously irradiated fields | |
| Other Indications | Idiopathic acute sensorineural hearing loss (SNHL) |
| Intracranial abscess | |
| Bell’s palsy | |
| B. Research indications: The role of HBO2 therapy in these indications is being studied in international trials. | |
| • HBO2 therapy in neurological illnesses: cerebral palsy, stroke, head injury | |
| • HBO2 therapy as a radiosensitizer in glioblastoma mutiforme and re-irradiation of squamous cell carcinoma. | |
Table 1: Indications for Hyperbaric Oxygen Therapy.
The only absolute contraindication to HBO2 therapy is untreated pneumothorax [10]. The reason is the concern of progression to tension pneumothorax, especially during the therapy decompression phase, although treatment on O2 based tables can prevent this progression [11]. A COPD patient with a large bleb represents a relative contraindication for similar reasons [12]. Also, the treatment may raise the issue of Occupational Health and Safety (OHS) hazards encountered by the therapists [13]. The side effects of HBO2 therapy are based on the physiologic response to a high O2 pressure environment, and the psychological reaction patients experience in the closed treatment chamber. Despite being one of the safest therapies, there are side effects associated with HBO2 therapy as with all medical treatments. The same mechanisms that result in HBO2 therapy’s beneficial effects can also cause known side effects in some patients [14]. Typically, most of HBO2 therapy’s side effects are mild and self-limited, but, there are risks associated with HBO2 therapy that are similar to some diving disorders. Lowering the ambient pressure causes increased gas volume while the opposite is also true [15]. These pressure effects are experienced within physiologic and pathologic air cavities and in the tissues surrounding trapped air inside the body. Of these are several barotraumas in the skull (behind the or inside paranasal sinuses, chest Pulmonary Barotrauma (PBT) or emphysematous bullae, teeth (trapped underneath dental fillings, etc. Middle Ear Barotrauma (MEB) is commonly recognized in the peer-reviewed literature where patient education on middle ear clearing, daily monitoring with otoscopy, and proper compression rates are important for prevention [16-19]. Discomfort inside the ears, as a pressure difference develops between the middle ear and the chamber’s atmosphere, may be noticed by patients inside the HBO2 therapy chamber, which can be readily relieved by ear clearing using the Valsalva maneuver or other techniques. Continued pressure increase without equalization may cause tympanic membrane rupture, resulting in severe pain. Also, as the pressure in the chamber increases further, the air may become warmer. Conversely, to reduce the pressure by opening a valve, the pressure falls, which may cause the patient's ears to squeak while the pressure inside the ear equalizes with the chamber with a concurrent fall in chamber temperature. This can be prevented by adjusting the speed of pressurization and depressurization to each patient's needs. In addition, even though an uncommon and selflimiting side effect, O2 toxicity seizure is one of the most dreaded side effects of HBO2 therapy. Fortunately, it has no long-term complications and usually resolves with the withdrawal of 100% O2. In such cases, continued HBO2 therapy is permissible with maximum allowed pressure adjustment and air breaks. Other HBO2 therapy side effects occurring especially in children include claustrophobia and confinement anxiety [19]. Temporarily blurred vision can be caused by swelling of the lens, which usually resolves in two to four weeks. There are also reports that cataracts may advance with HBO2 therapy.
Materials and Methods
Study design
This study is conducted using a cross-sectional survey design to study some side effects of HBO2 therapy in children with special needs aged 6 to 10 years (72-120 months).
Time and place of study
The study was conducted during the period from Oct 2018 through Feb 2021 in a Center for Children with Special Needs (a medical affiliation of a University in Cairo, Egypt).
Target population
The target population of the present study was all the children who visited the study center to receive treatments with HBO2 therapy, with other modalities, for any indication.
Inclusion criteria
Included in the study were all children with special needs who met the age range without the exclusion conditions.
Exclusion criteria
Excluded from the study were those with:
• Long-term drug therapy regimens.
• Ear problems (conductive deafness, eardrum problems).
• Children with upper or lower respiratory tract infections.
• Chromosomal or genetic syndromes.
• Abnormal brain MRI.
• Depression.
• Epilepsy.
Sampling technique
The target population yielded 100 respondents who constituted nearly 50% of the target population. The stratified purposive sampling technique was adopted to illustrate the characteristics of particular subgroups of interest.
Subject and method
This study was completed in a certain sequence to achieve the objectives of the study. It investigated the prevalence of some indications and common side effects of hyperbaric oxygen therapy (HBO2 therapy) in the sample. The final interview sheet and medical examination cum investigations form were designed to cover the following:
• General patients’ characteristics (demographics, socioeconomics, and anthropometrics).
• Prescribed medical indications of HBO2 therapy.
• Side effects and complications of HBO2 therapy.
• Medical examination and investigations.
Data collection tools
Interviews: The structured interview sheet was designed to accumulate enough information on the following points:
Sociodemographic characteristics: Parents’ education level, parents’ profession, Crowding Index calculation and parents’ and/or patients’ satisfaction with the treatment progress. In this study, the Household Crowding Index (HCI) was defined as the total number of co-residents per household, excluding the newborn infant, divided by the total number of rooms, excluding the kitchen and bathrooms. The continuous variable was re-grouped into four distinct categories: 1, 2, 3, and >3.
Hyperbaric oxygen therapy (HBO2 therapy) related variables: Through asking the following questions to the parents:
• How many sessions has the child taken?
• When was the first session?
• Did they do follow-up during HBO2 therapy?
• Did they notice any improvement in their child’s health problem?
• Did they notice any side effects of HBO2 therapy on their child?
• Was there any doctor or person in the child health center who discussed the importance of HBO2 therapy with them?
• Was there any doctor or person in the child health center who discussed the side effects of HBO2 therapy with them?
• Did the child take any medications before or during HBO2 therapy?
• Did the child take physiotherapy or any other form of therapy before or during HBO2 therapy?
Medical examination and investigations sheet
Anthropometric measurements: Patient’s age, gender, weight at birth and at time of visit, height, and head circumference.
General examination: Assessment of general appearance, final diagnosis, therapy modalities, and therapy frequency.
Investigations: Relevant labs, Chest X-ray.
Local examination: These clinical examinations were done by the researcher to assess the skin, upper limbs, lower limbs, chest, heart, abdomen, nervous system, ENT, and the eyes. In this examination, two major tests were performed and quantified:
ENT examination
Tympanometry: In our study, we used the tympanometry grading system below
Type A: Normal middle ear pressure
Type B: Otitis media with effusion
Type C: Eustachian tube dysfunction
Type AD: Hypermobile tympano-ossicuiar chain
Type AS: Decreased tympano-ossicular mobility
Modified teed score
Eustachian Tube Dysfunction (ETD) was classified and quantified using the modified Teed score Teed’s original classification included 5 grades, but it was modified to include another TM grade totaling 6 possible teed results:
Grade 0: Symptoms with no ontological signs of trauma
Grade 1: Diffuse redness and retraction of the TM
Grade 2: Grade 1 plus slight hemorrhage within the tympanic membrane
Grade 3: Grade 1 plus gross hemorrhage within the TM
Grade 4: Dark and slightly bulging TM due to free blood in the middle ear (a fluid level may also be present)
Grade 5: Free hemorrhage into the middle ear, TM perforation with blood visible in the external auditory canal
Hamilton Anxiety Rating Scale (HAM-A): It is essentially a clinician-rated psychological evaluation questionnaire used by clinicians to rate the severity of a patient's anxiety for individuals that are already diagnosed with anxiety neurosis. Composed of fourteen items, each item is presented in a specific format with some symptoms.
Statistical analysis
Data were collected, coded, and then analyzed using the Statistical Package for Social Science (SPSS version 25; IBM Inc.). The collected data were statistically managed by calculating the descriptive statistics, test of independence or pearson chi-square (χ2), and Analysis of Variance (ANOVA) followed, in some instances, by a Tukey’s post hoc test for the presence and/ or absence of statistically significant differences among the studied variables. The accepted level of significance, p-value, was set at ≤ 0.05. Finally, the results were represented in tabular and diagrammatic forms.
Results
Demographic, anthropometric and socioeconomic characteristics
The ages of the study participants ranged from 72 to 120 months (6-10 years) with a mean ± SD of 89.2 ± 16.7 months. Most of them were in the 6-7 years category (n=56), followed by 7-8 years (n=12), 8-9 years (n=14), and 9-10 years (n=18). As for participants’ gender, most of the children (n=69; 69.0%) were males, and (n=31; 31.0%) were females. Most children (n=59; 59%) were underweight while (n=33; 33%) were normal and only (n=8; 8%) were overweight. In addition, stunted children constituted (n=61; 61%), and normal (n=39; 39%). Those with microcephaly (n=58; 58%) and normal (n=42; 42%) without any macrocephaly cases. Studying the socioeconomic characteristics of the participants’ families included the parents’ education level, occupation, and the family housing crowding index (Table 2). None of these characteristics demonstrated statistically significant relationships with the other variables of the study.
| Category | Subcat. | Freq. | % |
|---|---|---|---|
| Father education | Illiterate | 25 | 25% |
| Low education | 30 | 30% | |
| Average education | 19 | 19% | |
| High education | 26 | 26% | |
| Mother education | Illiterate | 26 | 26% |
| Low education | 36 | 36% | |
| Average education | 13 | 13% | |
| High education | 25 | 25% | |
| Father occupation | High-scale profession | 45 | 45% |
| Merchant | 16 | 16% | |
| Clerical job | 19 | 19% | |
| Manual labor | 8 | 8% | |
| Farmer | 12 | 12% | |
| Mother occupation | Working | 40 | 40% |
| Housewife | 60 | 60% | |
| Crowding index | 2 | 41 | 41% |
| 3 | 49 | 49% | |
| 4 | 10 | 10% |
Table 2: Patients' socioeconomic characteristics.
Clinical attributes, tests and investigations
Results showed that for the final diagnosis, the highest frequency was with LDs (n=38; 38%), followed by CP (n=36; 36%). As regards receiving treatment, the number of therapy sessions ranged from 3 to 57 with a mean± SD of 22 ± 13.3 sessions (Table 3). Medical examinations and investigations revealed that on performing tympanometry most children (67%) had normal middle ear pressure, and with the modified teed score, more than one-half of children (56%) showed normal ear pressure (Figure 1). As regards tympanometry, there were statistically significant relationships between grades of tympanometry and Teed Score (p-value=0.00); a post hoc test showed that between groups the significant relationship escalated from one item of teed score to the other with tympanometry as follows: Type B>type AD>test not done>type AS>type C>type A.
| Cat | Subcat. | Freq. | % |
|---|---|---|---|
| Diagnosis | LD | 38 | 38% |
| CP | 36 | 36% | |
| ASD | 20 | 20% | |
| ADHDÂ | 4 | 4% | |
| Wound | 2 | 2% | |
| Therapy mode | Physiotherapy | 32 | 32% |
| Developmental therapy | 29 | 29% | |
| Conversation therapy | 23 | 23% | |
| Pharmaceutical | 16 | 16% | |
| Sessions number range | 1:10 total sessions | 26 | 26% |
| 11:20 total sessions | 36 | 36% | |
| 21:30 total sessions | 13 | 13% | |
| 31:40 total sessions | 15 | 15% | |
| 41:50 total sessions | 6 | 6% | |
| >50 total sessions | 4 | 4% | |
| Tympanometry | Type A: Normal middle ear pressure | 67 | 67% |
| Type AD: Hypermobile tympanoossicuiar chain | 5 | 5% | |
| Type AS: Decreased tympanoossicular mobility | 6 | 6% | |
| Type B: Otitis media with effusion | 6 | 6% | |
| Type C: Eustachian tube dysfunction | 4 | 4% | |
| Not done | 12 | 12% | |
| Modified teed score | Grade 0: Normal examination | 56 | 56% |
| Grade 1: TM injection or retraction | 24 | 24% | |
| Grade 2: Slightly hemorrhagic TM | 10 | 10% | |
| Grade 3: Grossly hemorrhagic TM | 3 | 3% | |
| Grade 4: Hemotympanum | 1 | 1% | |
| Grade 5: TM perforation | 6 | 6% | |
| HAM-A score | Mild symptoms | 98 | 98% |
| Moderate to severe symptoms | 2 | 2% | |
| Parents satisfaction | Highly satisfied | 21 | 21% |
| Satisfied | 26 | 26% | |
| Neutral | 35 | 35% | |
| Unsatisfied | 18 | 18% |
Table 3: Participants' clinical attributes, tests and investigations findings.
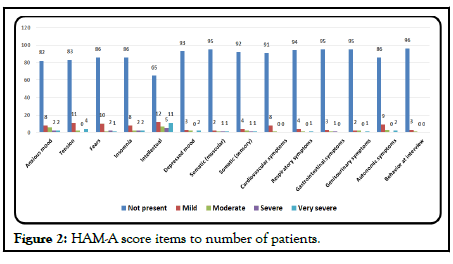
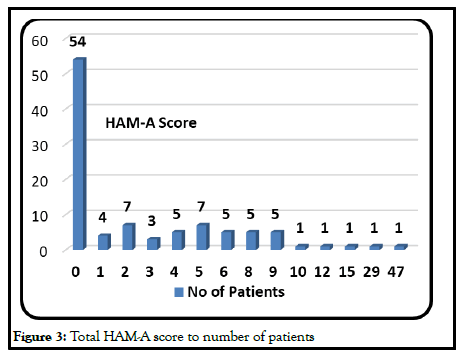
According to the HAM-A score, the majority of children had mild anxiety (98%) while only 2% had moderate to severe anxiety. Even though the scores fell within the range of (0-46), the Mean ± SD of the HAM-A score was 3.1 ± 6.1 (Table 3). A more detailed study of each of the HAM-A 14 items showed that, in general, most patients did not show any symptoms of anxiety and that more than one-half did not show any at all (Figures 2 and 3).
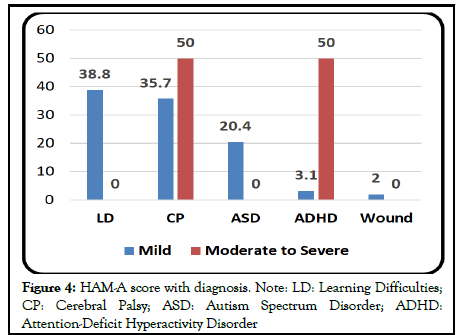
Also, there was a statistically significant relationship between HAM-A Score and diagnosis. The two cases of the moderate-severe form of anxiety were CP and ADHD (p=0.02) (Figure 4).
With the other tests and investigations (tympanometry, teed score, and parents’ satisfaction), a statistically significant relationship was found only between HAM-A score and tympanometry (p=0.00); the relationship escalated as follows: Type AD>type B>type A>test not done>type C>type AS.
As to parents’ satisfaction levels, 47% were satisfied; but, more than onethird (35%) were neutral and 18% were not satisfied (Table 3).
There were statistically significant relationships between grades of satisfaction and the age of patients, diagnoses, and the number of therapeutic sessions where (χ2) p-values=0.011, 0.019, and 0.000 respectively.
Dependent variables relationships
In the detailed analysis of all variables scrutinized in the study; especially, between the investigative tests done to measure side effects and the elements affecting them, several interrelationships of statistical significance were found among variables denoted by the p-values (Table 4).
| Variables | Tympanometry | Teed score | HAM-A score | Parents satisfaction | Diagnosis | No of sessions | Age |
|---|---|---|---|---|---|---|---|
| Tympanometry | - | 0 | 0 | 0.549 | 0.094 | 0.014 | 0.282 |
| Teed score | 0 | 0.393 | 0.522 | 0.029 | 0.111 | 0.194 | |
| HAM-A score | 0 | 0.393 | 0.522 | 0.016 | 0.003 | 0.218 | |
| Parents’ satisfaction | 0.549 | 0.522 | 0.522 | 0.019 | 0 | 0.011 | |
| Diagnosis | 0.094 | 0.029 | 0.016 | 0.019 | 0.821 | 0.001 | |
| No. of sessions | 0.098 | 0.82 | 0.003 | 0 | 0.821 | 0.276 | |
| Age | 0.282 | 0.194 | 0.218 | 0.011 | 0.001 | 0.276 |
Table 4: Detailed p-values of study variables’ relationships.
Discussion
For the pediatric population, the most common HBO2 therapy indications besides decompression sickness are acute ischemia, acute severe infection, air embolism, CO poisoning, chronic wounds, and osteomyelitis. Due to the immunomodulatory properties of HBO2, efforts are also made to use HBO2 therapy in atopic dermatitis or inflammatory bowel disease treatment. Optimum HBO2 therapy results can be achieved only with close cooperation between pediatricians and hyperbaric medicine teams. In treating a child with one of the disorders that can benefit from HBO2 therapy, all pediatric medicine branches should be involved including the general pediatrician, the Neonatal (NICU), and the Pediatric (PICU) Intensive Care Units’ consultants as well as the pediatric and orthopedic surgeons.
This study targeted 100 legible children (nearly 50% of the population) with special needs of all patients population visiting the study center for HBO2 therapy at the time of the study. Based on the study inclusion and exclusion criteria with a cross-sectional survey design, the included participants were the patients of mixed genders in the age range of 72 to 120 months, and their respondent parents/guardians. The study sample was withdrawn from the population using the stratified purposeful sampling technique, hence a lack of homogeneity in the distribution of age range and gender but we could only withdraw from the available legible patients. The response rate to the study interview form was 100%. To start with, we established a profile of the study patients, describing their demographic characteristics and their presentations. The analysis involved the examination of the portfolios of the 100 pediatric patients who completed a total of 2203 therapeutic sessions of different modalities including HBO2 therapy during the period from Jan 2019 through Dec 2020 (min=3 sessions, max=57 sessions, range=54 sessions; mean ± standard deviation=22.03 ± 13.26 sessions) for several indications related to special needs disorders.
The study sought to gather information on various aspects of the respondents’ background in terms of socioeconomic, and their level of satisfaction with the progress of their child therapy. Then, the respondents were asked to indicate the various diseases their child was being treated for and with which modalities in conjunction with HBO2 therapy. The most important tools used were the main interview form, which included the parents’ questionnaire as well as the medical examination/investigations sheet to record the demographic attributes and anthropometric measurements and to evaluate the patients’ general health status. Moreover, the patients’ general appearance, final case diagnosis, and therapy modalities/frequency were noted. In addition, the researcher systematically examined the patients’ skin, upper limbs, lower limbs, chest, heart, abdomen, nervous system, and eyes. In the special local examination, two major tests were performed and quantified: A thorough ear, nose, and throat examination, which included tympanometry and modified teed score evaluation as well as the hamilton anxiety score. For some patients, some labs and chest X-ray examinations were performed but not included in this study analysis.
Demographically, there were more boys than girls in the 6-7 years category. Being of a specific population with certain special needs, we noted the patients’ anthropometric measurements to classify them clinically. Results showed that the majority were in the underweight range (n=59; 59%), stunted (n=61; 61%), and with microcephaly (n=58; 58%). Understandably, these prevalent off-normal anthropometrics are commensurate with children with special needs that visit this particular center for treatments and do not represent the normal pediatric population in Cairo. Socioeconomically, the parents’ education level indicated the highest frequency of low education but father’s high-scale profession and mother’s occupation as a housewife. The housing crowding index was high in all instances with the highest incidence in the 3 category conforming to previous research.
Being of a particular university research nature, many of the indications for HBO2 therapy in this center are for research purposes some of which may not yet be confirmed by literature. Since we withdrew our sample from a population of children with special needs, the highest propensities among patients to be prescribed HBO2 therapy, as adjunctive therapy, were for Learning Disabilities LD (n=38; 38%) followed by Cerebral Palsy CP (n=36; 36%), and at third rank, Autism Spectrum Disorders ASD (n=20; 20%). The remaining few cases were divided between ADHD (n=4; 4%), and Wounds (n=2; 2%). In conjunction with HBO2 treatments, almost one third were treated with physiotherapy (n=32; 32%) followed by developmental therapy (n=29; 29%), conversation speech therapy (n=23; 23%) and lastly pharmaceutical therapy (n=16; 16%). In addition, during the study duration, the highest frequency of patients had 11-20 total sessions (n=36) followed by those who had 1-10 total sessions (n=26), 31-40 total sessions (n=15), 21-30 total sessions (n=13), 41-50 total sessions (n=6), and lastly, those who had more than 50 total sessions (n=4).
In our search to quantify the side effects of HBO2 therapy in our sample and to investigate their significant relationships with the study variables, we resorted to local ENT examination and patients’ anxiety severity measurement. Because MEB and ETD are the most common of HBO2 therapy side effects, the tympanometry test was a test in place here to evaluate the middle ear condition in the patients receiving HBO2 therapy. In our sample, the test could not be performed for 12 patients but of the 88 left, 78 were diagnosed with type A of which 5 were of type AD and 6 with type AS. Only 6 cases presented with type B, and 4 with type C. Similarly, based on the middle ear examination for ETD, the modified Teed score demonstrated suffering from a few side effects. Of the 100 cases, more than half (n=56; 56%) presented with grade 0, about one quarter (n=24; 24%) showed grade 1 while the rest were distributed among those with grade 2 (n=10; 10%), grade 3 (n=3; 3%), grade 4 (n=1; 1%) and grade 5 (n=6; 6%). Therefore, the findings corroborated other findings by previous studies, which postulated that MEB is usually mild, can be avoided, and its incidence can be reduced with adequate patient education, training, and assistance through active coaching during compression topical medications, and (in less common circumstances) relatively benign surgical intervention [19].
In addition, as claustrophobia appears to be present in about 2% of the general patient population and may cause some degree of confinement anxiety even in a multiplace chamber, we employed Hamilton Anxiety Score (HAM-A Score) to study anxiety symptoms severity in our study’s patients. The findings against all 14 axes of the score were very interesting. Almost all patients showed no anxiety symptoms (score range=82-96); in total, only two patients expressed moderate to severe symptoms (25 to 30) and the remaining 98 fell within grade 1: Mild prevalence of the feeling in the patient. This can be easily understood when we mention that the monoplace chambers in the center were made of glass where the partially-sedated child can see outside the chamber while the parent sits nearby, a factor that is highly reassuring for the child. The results agree with the literature where the incidence of confinement anxiety in monoplace chambers is reported at 8 events per 10,000 treatments and that mild confinement anxiety is easily controlled with sedation before treatments so that individuals may continue to receive daily HBO2 therapy. Preventive measures with adequate patient history, patient education, reassurance, and coaching are also among the most effective means of anticipating episodes of claustrophobia or anxiety and treating them effectively before HBO2 therapy [19]. To complete the analytical investigations, we resorted to analyzing parents’ satisfaction with the progress of their children’s treatment with HBO2 therapy (as adjunctive therapy) both qualitatively and quantitatively. Almost one-half were satisfied with the progress, of which 21 were highly satisfied and 26 satisfied. The neutral responses of slightly more than one-third (n=35; 35%) may have been biased due to parents’ emotional status of apprehension or worry at the time of the interview, their intelligence background, or their lack of education. However, the unsatisfied group constituted n=18 (18%) but this unsatisfaction included also the whole treatment regimen; i.e. HBO2 therapy and the main therapeutic modality.
It was beneficial for our study to investigate the relations between some responses and/or test outcomes and patients’ attributes such as their demographic, socioeconomic, anthropometric, and clinical characteristics. The analysis showed several significant relationships between some variables. For example, the HAM-A score had statistically significant relationships with tympanometry (p=0.000<0.05), Diagnoses (p=0.016<0.05), and Number of sessions (p=0.003<0.05). Parents’ satisfaction had statistically significant relationships with the age of Patients, diagnoses and number of therapeutic sessions on the other side where (χ2) p-values were 0.011, 0.019, and 0.000, respectively. The age of patients was statistically significant with diagnoses (p=0.001<0.05), and parents’ satisfaction (p=0.011<0.05). In the study, patients never complained of O2 toxicity after treatments. Reviewing chest Xrays of the patients did not reveal any pulmonary complications apart from the normal seasonal or infectious inflammations. In the same setting, history and perfunctory eye examination showed no relevant ophthalmological side effects or complications, or dental complaints.
Conclusion
HBO2 therapy is one of the safest curative modalities used today, even though its primary and secondary effects result in its benefits as well as its side effects. One of its most common side effects is MEB and subsequent ETD, which are typically mild and self-limited and can be prevented by patient instruction on middle ear clearing, daily monitoring with an otoscopic examination, and appropriate compression rates. Claustrophobia or confinement anxiety in monoplace chambers is another side effect of HBO2 therapy, but, it is generally mild and anxiety is easily controlled with sedation before treatments so that individuals may continue to receive daily HBO2 therapy. Preventive measures with adequate patient history, patient education, reassurance, and coaching are the most effective means of anticipating episodes of claustrophobia and treating them effectively before HBO2 therapy.
Ethical Consideration
Patients and their parents were educated on the purpose of the study. Any patient/guardian whose information was recorded had been notified and agreed to participate by written consent or a verbal assent before enrolling in the study that their medical information can be used and disclosed for scientific purposes.
Recommendations
Further research can explore ways of effectively identifying appropriate HBO2 therapy indications and unfavorable side effects beyond the scope of this study. MEB can be prevented by ongoing teaching of middle ear clearing techniques and appropriate compression rates. Claustrophobia may be managed with coaching and anxiolytic medications. Intolerance of a monoplace chamber may warrant referral to the closest multiplace chamber facility. PBT is unlikely and can be avoided with appropriate pretreatment screening. Providers should monitor the degree of change during treatment to assure safety and instruct patients to avoid a new permanent prescription until at least 8 weeks after treatment is completed. Certain precautions should be taken, and the involvement of multidisciplinary pediatric specialists and/or consultants in the prescription of HBO2 therapy is important when treating children, especially those with special needs.
References
- Thom SR. Hyperbaric oxygen: Its mechanisms and efficacy. Plastic Reconstruct Surg. 2011;127(1):131S-41S. [crossreff] [Googlescholar][Indexed]
- Sahni T, Hukku S, Jain M, et al. Rescent advances in hyperbaric oxygen therapy. Med Update. 2004;14:632-9. [Googlescholar]
- Virani SS. Heart disease and stroke statistics 2020 Update: A report from the american heart association. Circulation. 2020; 141:139-596.
- Schreiner RL, Kisling JA, Practical neonatal respiratory care. Raven Press, New York, 1982, pp. 469.
- US. Navy Supervisor of Diving, "U.S. Navy Diving Manual. SS521-AG-PRO-010, revision 6.", 20 ed., 5, U.S. Naval Sea Systems Command. 2008.
- Boyle R. A defence of the doctrine touching the spring and weight of the air, Thomas Robinson, London, 1662, pp. 57-68.
- Thom SR. Antidotes in depth: hyperbaric oxygen. Goldfrank’s Toxicologic Emergencies, 7th edition, McGraw-Hill, New York, 2002, pp. 1492-7.
- Thom S, Bhopale V, Velazquez O, et al. Stem cell mobilization by hyperbaric oxygen. Am J Physiol Heart Circ Physiol. 2006;290: 1378-86. [Googlescholar]
- Undersea and Hyperbaric Medical Society. Indications for hyperbaric oxygen therapy, 2020.
- Jain K. Indications, contraindications, and complications of HBO therapy. Textbook of Hyperbaric Medicine, Cham, Springer, Switzerland, 2017, pp. 75-80.
- Broome J, Smith D. Pneumothorax as a complication of recompression therapy for cerebral arterial gas embolism. Undersea Biomedical Research. 1992;19(6):447-55. [Googlescholar][Indexed]
- Marx J. Concepts and Clinical Practice. Rosen's Emergency Medicine, 5th edition, Elsevier Health Sciences, 2013.
- Liu YH, Hsia TC, Liu JC, et al. Fracture of the maxillary bone during hyperbaric oxygen therapy. CMAJ. 2008;179(12):1351. [Crossreff] [Googlescholar][Indexed]
- Liu ZJ, Velazquez OC. Hyperoxia, endothelial progenitor cell mobilization, and diabetic wound healing. Antioxidants Redox Signal. 2008;10(11):1869-82. [crossref] [Googlescholar][Indexed]
- Levine I. Physical Chemistry. McGraw-Hill, 1978.
- Fiesseler FW, Silverman ME, Riggs RL, et al. Indication for hyperbaric oxygen treatment as a predictor of tympanostomy tube placement. Undersea Hyperb Med. 2006;33(4):231-5. [Googlescholar][Indexed]
- Fitzpatrick DT, Franck BA, Mason KT, et al. Risk factors for symptomatic otic and sinus barotrauma in a multiplace hyperbaric chamber. Undersea Hyperbaric Med. 1999;26(4):243. [Googlescholar][Indexed]
- Broome JR, Smith DJ. Pneumothorax as a complication of recompression therapy for cerebral arterial gas embolism. Undersea Biomed Res. 1992;19(6):447-55. [Googlescholar][Indexed]
- Heyboer III M, Sharma D, Santiago W, et al. Hyperbaric oxygen therapy: Side effects defined and quantified. Adv Wound Care. 2017; 6(6):210-24. [crossref] [Googlescholar][Indexed]
- Stein L. Dental distress. The'diving dentist'addresses the problem of a diving-related toothache. Alert Diver. 2000, pp. 45-8.