Significance of keratinized tissue assessment in implant therapy
2 Department of Public Health, The Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA, Email: dentist123@gmail.com
3 Department of Endodontics, Rutgers School of Dental Medicine, Newark, NJ, USA, Email: dentist123@gmail.com
Received: 28-Aug-2017 Accepted Date: Jan 02, 2018; Published: 09-Jan-2018
Citation: Gharpure AS, Gharpure AS, Patankar NM. Significance of keratinized tissue assessment in implant therapy. Dentist Case Rep 2018;1(1):5-7.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The success of implant therapy is reliant on the precise, restoratively driven placement of dental implants in the oral cavity. Often, the native sites for implant placement demonstrate inadequate hard and soft tissue. Although bone augmentation techniques and materials have been extensively studied in the literature to obtain adequate hard tissue at proposed implant sites, only few publications have focused on the importance of soft tissue assessment and development. In the last few years, there has been a growing body of evidence suggesting the importance of keratinized tissue around dental implants. This paper reviewed the available literature on the importance of keratinized tissue assessment for implant based treatment. Several systematic reviews demonstrated that keratinized tissues may play a role in maintaining implant health and ensure a better prognosis for the final prosthesis. Soft tissue assessment at proposed implant sites needs to be prioritized at the time of clinical assessment and treatment planning. Such an approach would improve the predictability of implant restorations in terms of long-term maintenance.
Keywords
Keratin; Gingiva; Dental implantation; Dental implants; Humans
The predictably and success of implant based therapy rests on surgical implant placement in predetermined, restoratively driven locations of the jaws after adequate consideration is given to the native soft tissue, hard tissue and occlusion. It is important that implants are placed, keeping in mind the ideal three dimensional position, to optimize the prosthetic outcome [1]. However, before an implant can be placed in its correct restorative position, the assessment of local hard, soft tissue is important. In the absence of sufficient hard and soft tissue contours, augmentation procedures may be required to improve implant sites.
Literature Review
Although there have been several studies which have discussed hard tissue and soft tissue augmentation techniques for implant based treatment [2-6], the traditional emphasis has always been on the assessment of hard tissue profile and its development prior to soft tissue assessment [7]. Various bone grafting techniques and materials have been studied to augment the horizontal and vertical dimension of the alveolar ridge such as guided bone regeneration (GBR), onlay/veneer grafting, combinations of on lay, veneer, interpositional inlay grafting, distraction osteogenesis, ridge splitting, free and vascularized autografts for discontinuity defects, mandibular interpositional grafting, and socket preservation [6,8-10]. Satisfactory results in terms of implant survival have been demonstrated in systematic reviews comparing these techniques and no technique has been demonstrated to be superior as compared to others [6,8-11]. Thus, the current evidence indicates that any of the grafting procedures, after giving due consideration to their advantages and disadvantages, can successfully be used for ridge augmentation.
Unlike hard tissue augmentation, soft tissue assessment prior to implant placement has not been studied as extensively. However, in the last few years, there is growing evidence demonstrating the importance of the presence of keratinized tissue around implants and its role in maintaining lower plaque accumulation and tissue inflammation [12-16]. This paper looks at the available literature on the importance of keratinized tissue around dental implants in terms of maintaining optimal implant health. Aside from medical consultations and quit-lines, an efficient nicotine dependence treatment may include medication in the form of skin patches, lozenges, nicotine gums or nasal inhaler. Nicotine replacement drugs can easily be purchased over the counter and do not require a prescription. Medication decreases the signs and symptoms of nicotine withdrawal syndrome and somehow replaces the nicotine received from smoking [11,12].
Importance of keratinized tissue around dental implants
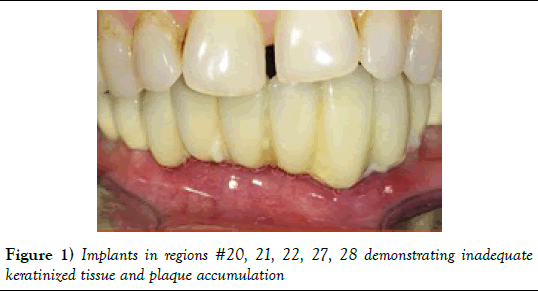
The traditional literature on grafting procedures has always been focused on development of alveolar hard tissue dimensions to allow implant placement in restoratively driven positions, without adequate stress on the available keratinized tissue around implants. There have been cases where implants have been placed in regions without sufficient keratinized tissue (Figures 1 and 2). The anatomy and histology of the mucosal attachment around dental implants is considerably different from that around natural teeth [17,18]. A direct anchorage of the connective tissue to the implant surface is not possible due the absence of periodontal ligament and cementum as seen in natural teeth. Instead, collagen fibers run parallel to the implant surface and the mechanical quality of this attachment is low [17,18]. On a biologic level, it would be favorable to have a zone of keratinized tissue around dental implants. However, the need for keratinized tissue around implants is highly debated. There have been several studies which have documented positive associations between the presence of adequate keratinized mucosa around implants and improved soft tissue health [19-21]. Further, lack of keratinized mucosa around implants has been demonstrated to make the peri-implant region more susceptible to plaque-induced tissue destruction [22]. Painful oral hygiene has been reported due to the absence of the keratinized tissue surrounding implants, and this has been attributed to the mechanical irritation caused by the mobility of the non-keratinized tissue under function [21,23]. Conversely, limited need for keratinized tissues around implants to maintain health and tissue stability has also been shown [24]. However, it must be noted that the majority of systematic reviews have indicated a positive relation between presence of keratinized tissue around implants and clinical parameters such inflammation and plaque accumulation [13-16]. Thus, the present literature indicates that keratinized mucosa around implants would improve the predictability of implant based treatment for long-term maintenance.
Discussion
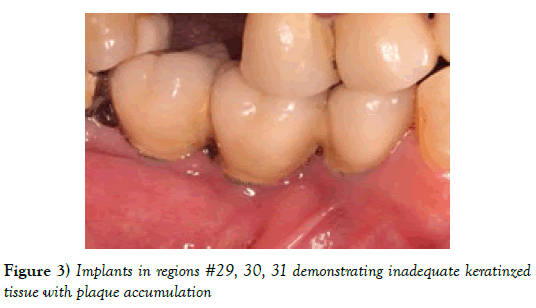
Guidelines to assess and develop keratinized tissue around implants
Although the need for keratinized mucosa around dental implants for success is controversial, as discussed earlier, several systematic reviews have shown that its presence is essential to maintain optimal implant health (Table 1) [13-16]. For those implants placed without any keratinized tissue as seen in Figure 3, studies have shown a higher buccal crestal resorption and a more apical soft tissue position when compared to those implants which have a 2 mm band [25]. A better prognosis has been demonstrated in implants having a band of 2 mm keratinized tissue in terms of plaque accumulation, tissue inflammation, mucosal recession and attachment loss [12,13]. Additionally, a significantly lower crestal bone change in bone-level implants placed in an initial keratinized tissue thicknesses of 2 mm or less has been shown in previous studies [26].
| Author, Year and Citation | Conclusion |
|---|---|
| Meffert et al. [14] | With no predictable epithelial attachment and less-than-optimum home care procedures, the soft tissue/implant interface is a very vulnerable area and at risk to gingival pathology. Keratinized tissue should be created with mucogingival surgical techniques prior to implant placement, if not present in adequate amounts. |
| Lin et al. [13] | A lack of adequate keratinized mucosa around endosseous dental implants is associated with more plaque accumulation, tissue inflammation, mucosal recession, and attachment Loss. |
| Gobbato et al. [15] | Reduced keratinized mucosal width around implants appears to be associated with clinical parameters indicative of inflammation and poor oral hygiene |
| Brito et al. [16] | Presence of an adequate zone of keratinized tissue may be necessary because it was shown to be related to better peri-implant tissue health |
Table 1: Systematic reviews and their conclusions on the importance of keratinized tissue around dental implants for maintenance
Other than maintaining adequate implant health, a good soft tissue profile may be necessary in the esthetic zone to establish a satisfactory restorative outcome. A vertical or horizontal soft tissue reconstruction would be necessary in case of a defect to improve the ridge morphology and the contour. Retaining and developing a minimum of 2 mm (1 mm on buccal and lingual aspect each) of keratinized tissue around implants would be advantageous not only in the long-term maintenance, but would also provide an esthetic profile.
Although there have been numerous publications on the importance of keratinized tissue around dental implants, and described techniques to augment this tissue [5,27,28] the timing and sequencing of soft-tissue grafts has not been sufficiently addressed. After a thorough clinical assessment, if a major correction of soft tissue is necessary (more than 2 mm of keratinized mucosa needs to be augmented at the proposed implant site), a soft tissue augmentation procedure needs to be performed first which may be carried out at the time of implant placement. Several systematic reviews have compared available soft tissue augmentation procedures [5,27,28], and all the compared techniques have provided adequate results, with no technique indicating substantial superiority over others. Free gingival grafts as well as connective tissue grafts in combination with an apically positioned flap/ vestibuloplasty have established reliable results to increase the width of the keratinized gingiva [7,29], and they may be used when a soft tissue correction of more than 1 mm is required. For minor soft tissue corrections (in which a total of less than 1 mm of the soft tissue needs to be augmented), a second stage approach may be used at the time of implant uncovery. Techniques such as roll flap can also be successfully used at second stage implant surgery for minor corrections [29].
Conclusion
There is a need for a well-organized protocol for assessing and planning soft tissue augmentation for implant site management with strong emphasis on soft tissue augmentation, prior to hard tissue assessment and grafting. The current evidence indicates that this would improve the prognosis of the treatment in terms of long-term implant health and maintenance. Thus, at the time of clinical examination for implant placement, it is critical to identify whether adequate keratinized tissue is available at the implant site and treatment plan the necessary soft tissue augmentation procedure if it is insufficient.
Conflict of Interest and Source of Funding
There was no support in the form of funding for this study; the authors declare that there was no conflict of interest.
Contributions
GH had the original idea, designed the study and outlined the first draft of the manuscript. MR, MA and BA contributed to revision of the article for important intellectual content, English editing and final approval.
REFERENCES
- Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19: 43-61.
- Bahat O, Fontanesi RV, Preston J. Reconstruction of the hard and soft tissues for optimal placement of osseointegrated implants. Int J Periodontics Restorative Dent. 1993;13: 255-75.
- Fagan MC, Owens H, Smaha J, et al. Simultaneous hard and soft tissue augmentation for implants in the esthetic zone: Report of 37 consecutive cases. J Periodontol. 2008;79: 1782-8.
- Salama H, Garber DA, Salama MA, et al. Fifty years of interdisciplinary site development: Lessons and guidelines from periodontal prosthesis. J Esthet Dent. 1998;10: 149-56.
- Wu Q, Qu Y, Gong P, et al. Evaluation of the efficacy of keratinized mucosa augmentation techniques around dental implants: A systematic review. J Prosthet Dent. 2015;113: 383-90.
- Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007;22: 49-70.
- Ioannou AL, Kotsakis GA, McHale MG, et al. Soft tissue surgical procedures for optimizing anterior implant esthetics. Int J Dent. 2015;2015: 740-64.
- Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants. 2009;24: 237-59.
- Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006;17: 136-59.
- Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: Clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants. 2009;24: 218-36.
- Rocchietta I, Fontana F, Simion M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: A systematic review. J Clin Periodontol. 2008;35: 203-15.
- Chung DM, Oh TJ, Shotwell JL, Misch CE, Wang HL. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006;77: 1410-20.
- Lin GH, Chan HL, Wang HL. The significance of keratinized mucosa on implant health: A systematic review. J Periodontol. 2013;84: 1755-67.
- Meffert RM, Langer B, Fritz ME. Dental implants: A review. J Periodontol. 1992;63: 859-70.
- Gobbato L, Avila-Ortiz G, Sohrabi K, Wang CW, Karimbux N. The effect of keratinized mucosa width on peri-implant health: A systematic review. Int J Oral Maxillofac Implants. 2013;28: 1536-45.
- Brito C, Tenenbaum HC, Wong BK, Schmitt C, Nogueira-Filho G. Is keratinized mucosa indispensable to maintain peri-implant health? A systematic review of the literature. J Biomed Mater Res Part B, Applied Biomaterials. 2014;102: 643-50.
- Abrahamsson I, Berglundh T, Wennstrom J, et al. The peri-implant hard and soft tissues at different implant systems. A comparative study in the dog. Clin Oral Implants Res. 1996;7: 212-9.
- Lindhe J, Berglundh T. The interface between the mucosa and the implant. Periodontol 2000. 1998;17: 47-54.
- Bouri A Jr., Bissada N, Al-Zahrani MS, et al. Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants. 2008;23: 323-6.
- Schrott AR, Jimenez M, Hwang JW, et al. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009;20: 1170-7.
- Adibrad M, Shahabuei M, Sahabi M. Significance of the width of keratinized mucosa on the health status of the supporting tissue around implants supporting overdentures. J Oral Implantol. 2009;35: 232-7.
- Warrer K, Buser D, Lang NP, et al. Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res. 1995;6: 131-8.
- Kaptein MLA, De Lange GL, Blijdorp PA. Peri-implant tissue health in reconstructed atrophic maxillae-report of 88 patients and 470 implants. J Oral Rehabil. 1999;26: 464-74.
- Wennstrom JL, Derks J. Is there a need for keratinized mucosa around implants to maintain health and tissue stability? Clin Oral Implants Res. 2012;23: 136-46.
- Bengazi F, Botticelli D, Favero V, et al. Influence of presence or absence of keratinized mucosa on the alveolar bony crest level as it relates to different buccal marginal bone thicknesses. An experimental study in dogs. Clin Oral Implants Res. 2014;25: 1065-71.
- Van Eekeren P, Van Elsas P, Tahmaseb A, et al. The influence of initial mucosal thickness on crestal bone change in similar macrogeometrical implants: A prospective randomized clinical trial. Clin Oral Implants Res. 2017;28: 214-8.
- Thoma DS, Buranawat B, Hammerle CH, et al. Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: a systematic review. J Clin Periodontol. 2014;41: S77-91.
- Esposito M, Maghaireh H, Grusovin MG, et al. Soft tissue management for dental implants: What are the most effective techniques? A Cochrane systematic review. Eur J Oral Implantol. 2012;5: 221-38.
- Bassetti RG, Stahli A, Bassetti MA, et al. Soft tissue augmentation procedures at second-stage surgery: A systematic review. Clin Oral Investig.2016;20: 1369-87.