Skin Tuberculosis Among Sudanese Multi-Drug Resistance Patience at Abu-Anja Teaching Hospital, 2020.
Received: 31-Jul-2023, Manuscript No. PULJEDPM-23-6627; Editor assigned: 02-Aug-2023, Pre QC No. PULJEDPM-23-6627(PQ); Accepted Date: Aug 14, 2023; Reviewed: 08-Aug-2023 QC No. PULJEDPM-23-6627; Revised: 12-Aug-2023, Manuscript No. PULJEDPM-23-6627(R); Published: 15-Aug-2023
Citation: Murad ZA, Eltahir MS, Hamdan HM. Skin tuberculosis among Sudanese multi-drug resistance patience at Abu-Anja teaching hospital, 2020. J Emerging Dis Prev Med. 2023;6(2):1-6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: To identify cutaneous manifestations of skin tuberculosis among MDR patients at Abu-Anga hospital Khartoum-Sudan during the year 2020 and to determine the most clinical variant skin tuberculosis in addition to its main risk factors.
Methods: Prospective, cross-sectional, hospital-based study. From January- December 2020. The study sample consisted of 62 patients attending the hospital and all were diagnosed as MDR tuberculosis. Data was collected using a detailed and structured data collection sheet.
Results: Two out of total number (n=62) were diagnosed as skin tuberculosis that confirmed with skin biopsy constituting 3.2%. the age of these patients was found 29 years and 70 years and both were male with one of them had diabetes, history of contact and pulmonary tuberculosis in one patient each time.
One patient was found to have scrofuloderma type and the other had lupus vulgaris type, BCG scar was negative in both patients while it was found in 20 patients (32.3%) of total patients with MDR.
All patients of this study with MDR were screened negative for HIV, 58 patients (93.5%) is having a history of pulmonary tuberculosis and a history of contact in 33 patients (53.2%) and diabetes mellitus was encountered in 12 patients (19.4%) .
In spite that the incidence of cutaneous tuberculosis among MDR is very low in Sudan yet it should be on back of the mind when treating chronic skin lesions.
Keywords
Skin tuberculosis; Cutaneous manifestation of tuberculosis; Multidrug resistant T.B; Scrofuloderma; Lupus vulgaris
Introduction
Tuberculosis (TB) continues to draw special attention from health care professionals and society. It still meets all the criteria for prioritization of a public health disorder, i.e., large magnitude, vulnerability and transcendence [1].
Cutaneous tuberculosis is an infection caused by M. Tuberculosis complex, M. Bovis and Bacillus Calmette-Guérin (BCG), which depending on individual immunity, environmental factors and type of inoculum may present varied clinical and evolutionary aspects [1].
The association of TB with HIV infection represents an additional challenge worldwide. An increase in its incidence has been described in several countries in recent years, especially in urban centers and regions with high prevalence of Human Immunodeficiency Virus (HIV) infection [2].
Multidrug Resistant Tuberculosis (MDR-TB) defined as TB caused by organisms that are resistant to isoniazide and rifampicin. Pulmonary complications of TB can include hemoptysis pneumothorax, bronchiectasis, extensive pulmonary destruction, malignancy and chronic pulmonary aspergilloses. Complications of skin TB involve nasal or auricular destruction and disfigurement, fibrosis and scaring, BCG scaring. Scaring of soft palate and laryngeal stenosis also occur in addition to SCC complications related to immune reconstitution induced by antiretroviral therapy, known as Immune Reconstitution Inflammatory Syndrome (IRIS) may occur, including paradoxical worsening of cutaneous tuberculosis and the emergence of subclinical infections. The most common clinical presentations of infection by Mycobacterium tuberculosis associated IRIS are lymphadenitis or lymphadenopathy [3-5].
Materials and Methods
Type of the study: Descriptive, hospital based cross-sectional, prospective study.
Study period: From January 2020-December 2020.
Study area: The study was done in Abu-Anga teaching hospital. The hospital located in Omdurman in the Khartoum capital of Sudan, these hospitals provide its services for very large area in Khartoum state the capital of Sudan and receive referral from almost all over the country, and it is considered the main hospital of tuberculosis in Sudan. It work via outpatients clinic and referral clinic, admission wards, pharmacy, laboratory, minor theatre, X-ray, HIV center and asthma ward, staffed with general practitioners, trainee residents, consultant chest physicians.
Study population: All patients presented with tuberculosis skin lesions in multidrug resistant patients.
Diagnosis: Skin tuberculosis is diagnosed by genotyping (tuberculosis and conversion diagnosed by sputum in central lab).
Sample size: All patients attending ABU-ANGA hospital during the period of the study because it’s the only hospital that treat multidrug-resistant patients in whom the skin manifestation will be studied.
Inclusion criteria: All patients presented with tuberculosis skin lesions in multidrug resistant patients with follow up and agreed to participate in the study.
Exclusion criteria: Non-Sudanese patients, and those who refused to be enrolled in the study.
Data collection tool: Was collected by the researcher via a specially constructed data collecting sheet by using direct interview, patients record and investigations results.
Data analysis: The data was analyzed by computer using Statistical Program for Scientific Science (SPSS).
Study variables: Age, gender, duration of the disease, duration of previous treatment, interruption of treatment, family history of pulmonary TB, relapse of TB, diabetes, HIV, BCG scar.
Results
This study was conducted at Abu-Anga teaching hospital in period from Jan-Dec 2020, it includes 62 patients all of them were MDR patients, and two patients were diagnosed as cutaneous tuberculosis.
The age group distribution in this study shown in Table 1, revealed a peak incidence as 40 (64.5%) for the patients aged 21-40 years and 11 (17.7%) for the age group 41-60 years and 6 (9.7%) for those aged less than 20 years.
| Frequency | Percent | |
|---|---|---|
| Less than 20 | 6 | 9.70% |
| 21-40 | 40 | 64.50% |
| 41-60 | 11 | 17.70% |
| More than 61 | 5 | 8.10% |
| Total | 62 | 100% |
TABLE 1: Shows age group distribution of patients with MDR tuberculosis at Abu-Anga teaching hospital during 2020.
Regarding the cutaneous manifestation among MDR patients which was encountered in 2 patients (3.2%) their age group was distribute in 21-40 (29 yrs) and the other in the age group more than 60 (70 yrs) as shown in Table 2.
| Frequency | Percent | |
|---|---|---|
| 21-40 | 1 | 50 |
| More than 61 | 1 | 50 |
| Total | 2 | 100 |
TABLE 2: Shows age group of patients with cutaneous manifestations among MDR Patients.
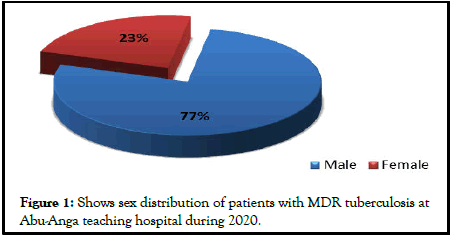
Male to female ratio was 3.4:1; males were 48 (77.4%) while females were 14 (22.6%),while in cutenous TB tow patients were male (Figure 1).
Income was found to be low in 48 (77.4%) and moderate in 14 (22.6) with no high income encountered. As shown in Table 3.
| Frequency | Percent | |
|---|---|---|
| Low | 48 | 77.40% |
| Moderate | 14 | 22.60% |
| Total | 62 | 100% |
TABLE 3: Shows risk factors income of patients with MDR tuberculosis at Abu-Anga teaching hospital during 2020.
Duration of primary treatment was of a range of less than 6 months in 55 (88.7%), 6 to 12 months in 6 (9.7%) and more than 12 months in only one case (1.6%) (Table 4).
| Frequency | Percent | |
|---|---|---|
| <6 months | 55 | 88.70% |
| <12 months | 6 | 9.70% |
| >12 months | 1 | 1.60% |
| Total | 62 | 100% |
TABLE 4: Shows duration of previous treatment among patients with MDR tuberculosis at Abu-Anga teaching hospital during 2020.
Interruption of treatment was encountered in 36 (58.1%) and not found in 26 (41.9%) as shown in Table 5.
| Frequency | Percent | |
|---|---|---|
| Yes | 36 | 58.10% |
| No | 26 | 41.90% |
| Total | 62 | 100% |
TABLE 5: Shows interruption of treatment among patients with MDR tuberculosis at Abu-Anga teaching hospital during 2020.
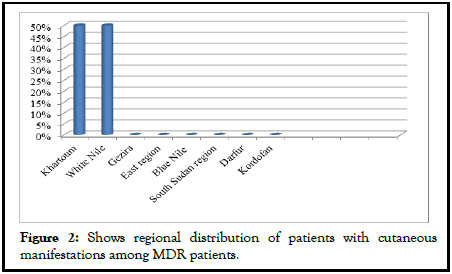
Regarding the cutaneous manifestation among MDR patients which was encountered in 2 patients their tribe was found to be Habania, although they were in different regions, Khartoum and White Nile (Figure 2). Their family members were found to be 7 and 10 members as shown in Table 6.
| Family members | Frequency |
|---|---|
| 7 | 1 |
| 10 | 1 |
| Total | 2 |
TABLE 6: Shows no of family members of patients with cutaneous manifestations among MDR patients.
Both two cases were found to be smokers as shown in Table 7, taking only two meals per day (Table 8) gene expert was done for all patients included in this study (Table 9), regarding cutaneous TB one of them is a case of relapse of pulmonary tuberculosis while relapse of pulmonary tuberculosis was found in 40 (64.5%) and not found in 22 (35.5%) in all patient with MDR as shown in Table 10.
| Frequency | Percent | |
|---|---|---|
| Smoker | 2 | 100 |
TABLE 7: Shows social habits and addiction of patients with cutaneous manifestations among MDR patients.
| Frequency | Percent | |
|---|---|---|
| 2 meals | 2 | 100 |
TABLE 8: Shows nutritional status of patients with cutaneous manifestations among MDR patients.
| Gene expert | Patients with cutaneous manifestations among MDR patients | All patients with MDR tuberculosis | ||
|---|---|---|---|---|
| Result | Positive | Negative | Positive | Negative |
| Frequency | 2 | 0 | 62 | 0 |
| Percent | 100% | 0 | 100% | 0 |
TABLE 9: Shows gene expert of patients with cutaneous manifestations among MDR patients vs. those without.
| Relapse of pulmonary tuberculosis | Patients with cutaneous manifestations among MDR patients | All patients with MDR tuberculosis | ||
|---|---|---|---|---|
| Result | Positive | Negative | Positive | Negative |
| Frequency | 1 | 1 | 40 | 22 |
| Percent | 50% | 50% | 64.50% | 35.5 |
TABLE 10: Shows relapse of pulmonary TB of patients with cutaneous manifestations among MDR patients vs. those without.
History of pulmonary tuberculosis found in both patient with cutaneous TB while in all MDR patients history of pulmonary tuberculosis was found in 58 (93.5%) and extra-pulmonary tuberculosis 4 (6.5%) (Table 11).
| History of pulmonary TB | Patients with cutaneous manifestations among MDR patients | All patients with MDR tuberculosis | ||
|---|---|---|---|---|
| Result | Positive | Negative | Positive | Negative |
| Frequency | 2 | 0 | 58 | 4 |
| Percent | 100% | 0% | 93.50% | 6.50% |
TABLE 11: Shows history of pulmonary TB of patients with cutaneous manifestations among MDR patients vs. those without.
HIV was negative in both patients with cutaneous TB and MDR patients (Table 12) diabetes was encountered in one patient with cutaneous TB while in MDR patients, diabetes mellitus was reported in only 12 (19.4%) of the patients as shown in Table 13.
| HIV | Patients with cutaneous manifestations among MDR patients | All patients with MDR tuberculosis | ||
|---|---|---|---|---|
| Result | Positive | Negative | Positive | Negative |
| Frequency | 0 | 2 | 0 | 62 |
| Percent | 0% | 100% | 0% | 100% |
TABLE 12: Shows HIV in patients with cutaneous manifestations among MDR patients vs. those without.
| Diabetes | Patients with cutaneous manifestations among MDR patients | All patients with MDR tuberculosis | ||
|---|---|---|---|---|
| Result | Positive | Negative | Positive | Negative |
| Frequency | 1 | 1 | 12 | 50 |
| Percent | 50% | 50% | 19.40% | 80.6 |
TABLE 13: Shows diabetes in patients with cutaneous manifestations among MDR patients vs. those without.
In cutaneous TB one case was found to have a history of contact with tuberculosis while the other didn’t remember while in MDR patients contact with tuberculosis patients encountered in 33 (53.2%), not encountered in 8 (12.9%), and 21 (33.9%) of patients didn’t remember any contact and as shown in Table 14.
| Contact with tuberculosis patients | Patients with cutaneous manifestations among MDR patients | All patients with MDR tuberculosis | ||
|---|---|---|---|---|
| Result | Positive | Negative | Positive | Negative |
| Frequency | 1 | 1 | 62 | 0 |
| Percent | 50% | 50% | 100% | 0 |
TABLE 14: Shows contact with tuberculosis patients of patients with cutaneous manifestations among MDR patients vs. those without.
In cutaneous TBboth of them BCG scar was not detected while in MDR patient’s presence of BCG scar was found in 20 out of the total number of the patients in this study, These represent 32.3% as shown in Table 15. According to the types of skin tuberculosis lupus vulgaris was found in one case (50%) and scrofuloderma was found in the other (50%) (Table 16).
| BCG | Patients with cutaneous manifestations among MDR patients | All patients with MDR tuberculosis | ||
|---|---|---|---|---|
| Result | Positive | Negative | Positive | Negative |
| Frequency | 0 | 2 | 20 | 42 |
| Percent | 0% | 100% | 32.30% | 67.70% |
TABLE 15: Shows BCG scar of patients with cutaneous manifestations among MDR patients vs. those without.
| Frequency | Percent | |
|---|---|---|
| Lupus valgaris | 1 | 50 |
| Scofulderma | 1 | 50 |
| Total | 2 | 100 |
TABLE 16: Shows type of skin TB in patients with cutaneous manifestations among MDR patients.
Discussion
In this study 62 patients with MDR tuberculosis were enrolled two of them had cutaneous tuberculosis. 40 patients (64.5%) of the patients aged 21-40 years similar to a study from china who found the common age to be less than 45 years [6] and similar to the data from India-Delhi tuberculosis center the common age was found to be ranging from 18-58 years, [7] males were 48 (77.4%) while females were 14 (22.6%). With a ratio of 3.4:1 similar to data the data from India-Delhi tuberculosis center who found out of 196 146 were male (74.5%) and 50 female (25.5%) and in contrast to a study from Georgia where they found it more common in female [8].
Presence of certain risk factors was found in a significant percentage of the total number of the patients in this study. These conditions include previously treated patients 55 (88.7%) similar to 96.1% of patients managed for MDR reported by Mulu from Bahirdar-Ethiopia [9]. The association between number of a previously treated and MDR tuberculosis might be due to poor adherence to treatment. History of contact was found in 33 (53.2%) while Mulu study of Ethiopian Bahirdar the percentage was 28.2% this association could be attributed to acquiring of primary drug resistant strain of bacteria. From this study the income was found low in 48 (77.4%) while in Mulu from Bahirdar-Ethiopia found percentage of 51.6%. This may explain the poor compliance to treatment poor living and housing and limited ability to access health services thus aiding in spread of infection with bacilli.
With regard to HIV as a risk factor in this study 100% of patients were negative that is similar to a study from South Africa done by Holtz et al., who showed that HIV has no significant association with MDR tuberculosis [10] and in contrast to a study in France and Ukraine being HIV positive was associated with primary MDR tuberculosis [11,12].
In this study 36 out of 62 cases (58.1%) had a history of interrupted treatment this indicate poor compliance in Sudanese patients compared to the Ethiopian population showed in Mulu study as being (14.3%) [9].
58 patients (93.5%) was found to have a history of pulmonary tuberculosis similar to Mulu study (92.2%) [9].
The two patients that had been found to have a cutaneous tuberculosis among 62 patients with MDR enrolled in this study represent a percentage of (3.2%), this is similar to a study by V. Ramesh et. al., who found 6 cases out of 303 cases with MDR studied over 4 and half years, five of this 6 patients were children and one adult in contrast to my study where both cases were adult and of male gender in contrast to V. Ramesh et al., where 5 is of female gender with one male also they found them all negative for HIV similar to my study [13].
One of the main objectives of this study is to identify the major risk factors for developing cutaneous tuberculosis and this include smoking, poverty, malnutrition, overcrowded living condition, similar to Mouded Almatori study [14].
Both of my two cases were negative for HIV similar to V. Ramesh et. al., who found all his 6 patients to be negative [13] and in contrast to a study by Joseph Barbagallo et al., done in New York-USA they concluded that cutaneous tuberculosis had a high prevalence of HIV infection and relate this to high pandemic spread of HIV infection [15]. While in a study from India by Anupam Varshney and his colleague Tarang Goyal, they found out 18720 patients studied over a period of two years the cutaneous tuberculosis is confirmed in 131 patients in a percentage of 0.7% with HIV infection to be 0.16% of total number studied [16].
The clinic-morphologic results were one case (50%) is of scrofuloderma type and the other case (50%) is lupus vulgaris similar to Indian study by Anupam Varshney and his colleague who found the most common type is scrofuloderma constituting (36%) and predominantly seen in younger with mean age 23 years and our study the patient is 29 years, and lupus vulgaris to be (30.5) [16].
Conclusion
There is annual increase in detection of cases of MDR which doesn’t reflect the magnitude of the problem because it’s only one center. Cutaneous tuberculosis among MDR still had low prevalence. Painless ulcers attending different clinic should be given attention. In spite that the risk of HIV is zero and that of diabetes mellitus is low among the patients, poverty and poor housing still considered the main risk factors.
References
- Dias MF, Bernardes Filho F, Quaresma MV, et al. Update on cutaneous tuberculosis. An Bras Dermatol. 2014;89:925-38.
[Google Scholar] [Crossref] [PubMed]
- Yates VM. Mycobacterial infections. In: Burns T, Breathnach S, Cox N, Griffiths C, Editors. Rook's Textbook of Dermatology. 8th Edition. Wiley Blackwell; 2010;1-30.
- Huiras E, Preda V, Maurer T, et al. Cutaneous manifestations of immune reconstitution inflammatory syndrome. Curr Opin HIV AIDS. 2008;3(4):453-60.
[Google Scholar] [Crossref] [PubMed]
- Robertson J, Meier M, Wall J, et al. Immune reconstitution syndrome in HIV: Validating a case definition and identifying clinical predictors in persons initiating antiretroviral therapy. Clin Infect Dis. 2006;42(11):1639-46.
[Google Scholar] [Crossref] [PubMed]
- Müller M, Wandel S, Colebunders R, et al. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: A systematic review and meta-analysis. Lancet Infect Dis. 2010;10(4):251-61.
[Google Scholar] [Crossref] [PubMed]
- Liang L, Wu Q, Gao L, et al. Factors contributing to the high prevalence of multidrug-resistant tuberculosis: A study from China. Thorax. 2012;67(7):632-8.
[Google Scholar] [Crossref] [PubMed]
- Sharma SK, Kumar S, Saha PK, et al. Prevalence of multidrug-resistant tuberculosis among category II pulmonary tuberculosis patients. Indian J Med Res. 2011;133(3):312.
[Google Scholar] [PubMed]
- Lomtadze N, Aspindzelashvili R, Janjgava M, et al. Prevalence and risk factors for multidrug-resistant tuberculosis in the republic of Georgia: A population-based study. Int J Tuberc Lung Dis. 2009;13(1):68-73.
[Google Scholar] [PubMed]
- Mulu W, Mekkonnen D, Yimer M, et al. Risk factors for multidrug resistant tuberculosis patients in Amhara national regional state. Afr Health Sci. 2015;15(2):368-77.
[Google Scholar] [Crossref] [PubMed]
- Holtz TH, Lancaster J, Laserson KF, et al. Risk factors associated with default from multidrug-resistant tuberculosis treatment, South Africa, 1999-2001. Int J Tuberc Lung Dis. 2006;10(6):649-55.
[Google Scholar] [PubMed]
- Akksilp S, Wattanaamornkiat W, Kittikraisak W, et al. Multi-drug resistant TB and HIV in Thailand: Overlapping, but not independently associated risk factors. Southeast Asian J Trop Med Public Health. 2009;40(6):1264.
[Google Scholar] [PubMed]
- Schwoebel V, Decludt B, de Benoist AC, et al. Multidrug resistant tuberculosis in France 1992-4: Two case-control studies. Bmj. 1998;317(7159):630-1.
[Google Scholar] [Crossref] [PubMed]
- Ramesh V, Sen MK, Sethuraman G, et al. Cutaneous tuberculosis due to multidrug-resistant tubercle bacilli and difficulties in clinical diagnosis. Indian J Dermatol Venereol Leprol. 2015;81:380.
[Google Scholar] [Crossref] [PubMed]
- Moudad Alamatori. Overview of cutaneous tuberculosis. Crimson J Skincare Hair Ther. 2018.1(1).
- Barbagallo J, Tager P, Ingleton R, et al. Cutaneous tuberculosis: Diagnosis and treatment. Am J Clin Dermatol. 2002;3:319-28.
[Google Scholar] [Crossref] [PubMed]
- Varshney A, Goyal T. Incidence of various clinico-morphological variants of cutaneous tuberculosis and HIV concurrence: A study from the Indian subcontinent. Ann Saudi Med. 2011;31(2):134-9.
[Google Scholar] [Crossref] [PubMed]