Successful Management of an Emergent Cesarean Delivery in a Patient with History of Ross Procedure: A Case Report
Received: 22-Jan-2018 Accepted Date: Feb 06, 2018; Published: 11-Feb-2018
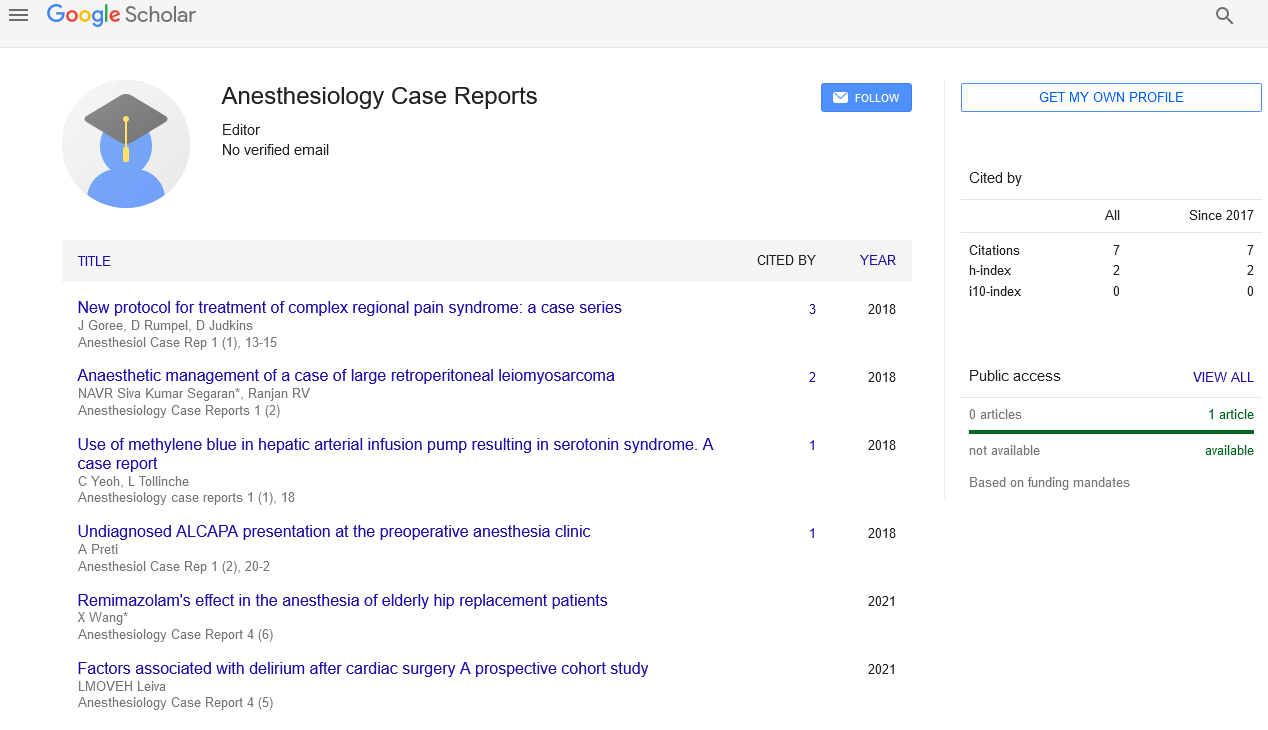
Citation: Nguyen TA, Duarte SS, Berman DJ, et al. Successful Management of an Emergent Cesarean Delivery in a Patient with History of Ross Procedure: A Case Report. Anesthesiol Case Rep. 2018;1(1):10-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Severe aortic valvular disease can be treated with valve replacement using an autologous pulmonary valve, also known as the Ross procedure. In young females who wish to bear children in the future, the Ross procedure may be a preferable option over mechanical or bioprosthetic valve replacement, as it offers long-term durability without the need for life-long anticoagulation. However, it is not without complications. Herein, we present the successful perioperative anesthesia management of a patient with history of Ross procedure and mitral valve bioprosthesis, with subsequent development of severe aortic insufficiency and moderate mitral stenosis, who delivered a preterm infant via emergent Cesarean section. This case highlights the value of early identification of high-risk parturients, the benefit of early referral to anesthesia preoperative evaluation to establish an anesthetic plan, and the multidisciplinary involvement in the perioperative period.
Keywords
Ross procedure; Perioperative management; Parturient; Congenital heart disease; Cesarean sectionIntroduction
Advances in medical and surgical treatments of congenital heart disease in conjunction with improvement in fertility interventions have led to an increase in the proportion of women with congenital cardiac disease and/or acquired heart disease that have the potential of becoming pregnant [1]. Although pregnancy in women with prosthetic heart valves continues to show increased risk of adverse outcomes as compared to the general population, rates of maternal mortality and pregnancy loss have declined over the last two decades [2]. Common treatment options for severe aortic valvular disease include mechanical and bioprosthetic (heterograft, homograft and autograft) valve replacement [3], both providing advantages and limitations for young females who desire pregnancy in the future. Mechanical heart valves offer long-term durability and superior hemodynamic profile; however they are prothrombotic requiring life-long anticoagulation with potential increase risk to mom and fetus [4].
Bioprosthetic heart valves, on the other hand, do not require anticoagulation, but are less durable and frequently require reoperation [5].
The Ross procedure, first described in 1967, involves the replacement of the aortic valve with an autologous pulmonary valve and an allograft in the pulmonary position. This procedure obviates the need for anticoagulation, and may potentially have longer durability than aortic bioprosthetic valves [3]. For these reasons, the Ross procedure is the preferred aortic valve replacement strategy for younger women who desire pregnancy in the future [6]. Here we describe a case of a patient with history of Ross procedure and mitral valve replacement, with subsequent development of aortic insufficiency and mitral stenosis, who successfully delivered a preterm infant via emergent cesarean section, with a specific focus on the peri-operative anesthesia planning and management.
Case Report
Pre-partum assessment and planning
The patient was a 38 year old gravida 1 woman who presented to antenatal anesthesia clinic for pre-evaluation at 26 weeks 1 day gestation, 6 years status post Ross procedure and mitral valve replacement for severe aortic stenosis (AS) and mitral stenosis (MS), respectively. Her long-standing history of valvular heart disease was diagnosed at the age of 19 during a medical work-up when she presented with pneumonia and a pleural effusion. Given her symptoms and valves involved, her valvulopathy was presumed to be secondary to rheumatic fever. The patient’s other comorbidities included history of asthma, anemia, obstructive sleep apnea, prior cervical fusion of C5-7, history of difficult airway and was on therapeutic anticoagulation during this pregnancy with therapeutic enoxaparin as per her cardiologist’s recommendations.
Patient reported that she had a VSD at birth that closed spontaneously by age 1. She otherwise reported having a healthy childhood prior to the diagnosis of her valvular disease. After a failed mitral valvuloplasty at 25 years old, the patient underwent a Ross procedure at age 32 for her severe aortic stenosis. Three days after her Ross procedure, patient had significant cardiac decompensation requiring intubation, developed atrial fibrillation requiring anticoagulation, was initiated on CVVH for AKI, had shock liver and developed severe pulmonary HTN requiring inhaled nitric oxide. Cardiac decompensation was considered to be as a result of mitral stenosis and thus she received a mitral valve replacement with a porcine bioprosthetic valve and tricuspid valve annuloplasty. Per operative report, they noted dense pericardial adhesions during this repeat sternotomy and reported that they did not close pericardium but left a Gore-Tex mesh anterior to her RV.
Overall her pregnancy course was uncomplicated, with the exception of intermittent worsening of lower extremity edema and dyspnea. She was followed closely by cardiology throughout her pregnancy that started her on enoxaparin given the risk of left atrial thrombosis secondary to her now moderate MS and severe Aortic Insufficiency (AI). The patient appeared to be doing well with stable NYHA II symptoms and was euvolemic on exam. TTE revealed left ventricular ejection fraction (LVEF) of 45 % with hypokinetic septum, bioprosthetic MV without significant regurgitation and mean gradient 7.8mmHg, moderate to severe AI, and tricuspid annuloplasty without significant tricuspid stenosis or regurgitation. At 20 weeks gestation, she had an ultrasound concerning for placenta previa. Repeat imaging demonstrating a succenturiate placenta with large echogenic peri-placental collection consistent with a small bleed that had remained unchanged.
It was discussed with patient that her pre-anesthesia plan during delivery was to try to remain euvolemic during the intrapartum and post-partum periods, given her cardiac history and predisposition for volume overload. Increases in afterload were to be avoided, as they could worsen regurgitation and atrial volume overload. The goal heart rate was about 70-90 bpm as bradycardia would increase time for regurgitant flow. For a vaginal delivery, early placement of an epidural catheter with slow careful titration would be preferred, provided that her anticoagulation schedule allowed us, as neuraxial anesthesia reduces afterload, sympathetic outflow, and the resultant catecholamine surges associated with labor and delivery. If a cesarean section was required, the team discussed the need for an arterial catheter for close hemodynamic monitoring and recommended an epidural again with slow titration. Spinal anesthesia was not recommended as the associated lability and potential of extreme hypotension could be difficult to manage in her complex cardiac picture.
As her anticoagulation regimen affected our anesthetic neuraxial plan, we planned on discussing the heparin anticoagulation plan in the intrapartum and postpartum periods with the patient’s obstetrician and cardiologist. In the event that the patient had a cesarean section under epidural, we recommended the use of epidural morphine in order to allow for immediate discontinuation of the catheter while still providing postoperative pain control and allowing postoperative anticoagulation to be resumed.
Based on cardiology’s recommendation for admission and delivery in the Cardiac Care Unit (CCU), if an operative delivery were to be required, the case would proceed in the cardiac operating rooms. In the event of emergent cesarean section, it was discussed with the patient that most likely General Anesthesia (GA) would be needed, in addition to the possibility of central venous access, TTE/TEE, prolonged intubation and even the need for cardiac surgery in the event of acute cardiac decompensation. With regard to her history of difficult airway, if GA would be required, the team discussed the possibility of direct laryngoscopy with glidescope versus awake fiberoptic intubation.
Peri-partum anesthesia management of emergent cesarean section
The patient presented to the labor and delivery (L&D) floor at 28 weeks 4 days with vaginal bleeding, 10 pounds weight gain and worsening bilateral lower extremity swelling. She was placed on continuous fetal monitoring and was noted to have contractions. Betamethasone was administered for fetal lung maturity and she was placed on a magnesium infusion for fetal neuroprotection and tocolysis. Cardiology was consulted at this time who recommended discontinuation of the enoxaparin in the setting of vaginal bleeding and actively diuresing the patient with a goal of 2 L/day net negative. On post-admission day 2, she had an episode of unprovoked, continuous vaginal bleeding with estimated blood loss (EBL) of 500 ml. It was decided, given her unstable status, to take the patient for emergent cesarean section and bilateral tubal ligation.
The patient was taken to the cardiac operating room (OR) as discussed in her preoperative evaluation appointment and cesarean section was done under general anesthesia. After the placement of an awake arterial line, she underwent a rapid sequence induction with 150 mg of ketamine and 100 mg of succinylcholine. The patient also received 250 mcg of carboprost and 200 mcg of methylergonovine intramuscularly after the fetus was delivered. Patient delivered a baby girl with APGARS of 2 and 9 at 1 and 5 min respectively. She received 2 units of pRBCs and 2 L of lactated ringers, and EBL was 2 L. Despite receiving 120 mg of sugammadex for the 3 mg of vecuronium that she received during the case and optimizing her position, patient was retaining CO2, so she was transferred intubated to the CVSICU. Five hours later, the patient was successfully extubated and the following day was transferred back to the regular L&D floor.
Repeat TTE post-delivery was limited, but was not remarkably different from before. Patient was successfully discharged home on POD 5, and on POD 13 at the outpatient obstetric clinic she was noted to be doing well with improving lower extremity edema. Infant was still in the Neonatal Intensive Care Unit at that time but also noted to be doing well.
Discussion
As per the CDC Pregnancy Mortality Surveillance System, the proportion of pregnancy-related deaths in the United States caused by cardiomyopathy and cardiovascular disease has increased progressively in the last 25 years from about 8% between 1987-1990 to over 26% between 2011-2013 [7,8]. This may be due in part to advances in medicine and surgical managements of congenital heart defects (CHD), leading to increasing numbers of parturients with repaired or unrepaired lesions. Indeed, a nationwide study demonstrated that the number of delivery hospitalizations with CHD in the US has significantly increased from 6.4 to 9.0 per 10,000 deliveries from 2000 to 2010 [1]. In the setting of the physiologic changes in pregnancy (increased cardiac output, blood volume, contractility and heart rate) the cardiac demand surges and can lead to worsening of such lesions and/or cardiac decompensation. In fact, the odds of cardiovascular and obstetric complications occurring are 10.5-35.5 and 1.2-2.1 times higher, respectively, among delivery hospitalizations with CHD. Also, although delivery hospitalizations with CHD made up only 0.085% of all deliveries, they accounted for 2% of in-hospital deaths [1].
For these reasons, it is strongly recommended that anesthesia be consulted and involved early in the peri-partum decision-making and planning (e.g. late second trimester). Multidisciplinary care and open communication between teams is associated with improved mortality in women with preexisting cardiac disease, and some major academic centers have even established guidelines for when to consider anesthesia consultation by the obstetrics team [9,10]. This allows the anesthesiology team to plan in advance for airway and anesthetic approaches both in the “ideal” as well as “emergent” settings, as illustrated in the case above. Moreover needs regarding fluid management, anticoagulation, hemodynamic monitoring, medication administration and post-operative monitoring unit can be better anticipated.
Among parturients with pre-existing cardiac disease, those with significant stenotic valves, pulmonary hypertension and/or severe cardiomyopathy tend to be least able tolerate labor and anesthesia, due to the potential for significant shifts in hemodynamics [10]. In recent years, tools such as CARPREG, ZAHARA, and the modified WHO system have been created to aid in risk assessment for parturient patients with cardiac conditions [11-13]. Using CARPREG, our patient had a 27% risk for cardiac complication during pregnancy, while the risk using ZAHARA was 70%. Under the modified WHO system, which seems to perform the best of the three in estimating cardiovascular risk [14] our patient was Class 2-3 or moderate-high risk.
Given her decreased ejection fraction and moderate-severe AI, our initial anesthetic plan for her delivery included maintaining euvolemia and preventing increases in afterload. For these reasons, neuraxial slow controlled epidural anesthesia is preferred over general anesthesia. Complicating the issue, however, was her anticoagulation. Because of the risk of symptomatic spinal hematoma and spinal cord injury, anticoagulation is a relative contraindication to neuraxial anesthesia. Commonly patients on low-molecular-weight heparin (e.g. lovenox) are transitioned off 24-36 h prior to delivery, after which time neuraxial anesthesia may be considered. High-risk patients may be switched to intravenous heparin until 4 h prior to delivery. Unfortunately due to the lack of rigorous data, most recommendations are based on expert opinion and consensus [15,16].
Another essential conversation to have between multidisciplinary team and the patient with significant cardiac disease is the mode of delivery. Vaginal delivery is generally preferred as it usually has less blood loss and fluid shifts as compared to cesarean section [17] while on the other hand cesarean sections may be completed in significantly less time potentially avoiding prolonged cardiovascular stress due to protracted labor. Moreover, a small prospective study found no differences in maternal or fetal outcomes in high-risk cardiac parturients undergoing either vaginal or cesarean delivery under regional anesthesia [18] but further studies are needed to replicate these findings.
Conclusion
Although the Ross procedure is the generally preferred procedure for young female with severe aortic valve disease, due to its excellent durability and lower early and late mortality as compared to mechanical and bioprosthetic aortic valves [3] it can present with complications, as seen in our patient. Referring high-risk cardiac parturients to anesthesia early in their pregnancy is essential, and allows for pre-partum discussion and decision-making regarding airway, anesthesia, hemodynamic monitoring, and delivery strategies. Consequently, despite her emergent presentation at 28 weeks, gathering of information and her anesthetic planning had already taken place, facilitating a successful delivery and post-partum outcome for both mother and child.
REFERENCES
- Thompson JL, Kuklina EV, Bateman BT, et al. Medical and Obstetric Outcomes Among Pregnant Women With Congenital Heart Disease. Obstet Gynecol 2015;126(2):346-54.
- Lawley CM, Lain SJ, Algert CS, et al. Prosthetic heart valves in pregnancy, outcomes for women and their babies: a systematic review and meta-analysis. BJOG 2015;122(11):1446-55.
- Etnel JRG, Elmont LC, Ertekin E, et al. Outcome after aortic valve replacement in children: A systematic review and meta-analysis. J Thorac Cardiovasc Surg 2016;151(1):143-52.
- Vitale N, De Feo M, De Santo LS, et al. Dose-dependent fetal complications of warfarin in pregnant women with mechanical heart valves. J Am Coll Cardiol 1999;33(6):1637-41.
- Elkayam U, Bitar F. Valvular heart disease and pregnancy: part II: prosthetic valves. J Am Coll Cardiol 2005;46(3):403-10.
- Al-Halees Z, Pieters F, Qadoura F, et al. The Ross procedure is the procedure of choice for congenital aortic valve disease. J Thorac Cardiovasc Surg 2002;123(3):437-41.
- Callaghan WM. Overview of maternal mortality in the United States. Semin Perinatol 2012;36(1):2-6.
- Creanga AA, Syverson C, Seed K, et al. Pregnancy-Related Mortality in the United States, 2011-2013. Obstet Gynecol 2017;130(2):366-73.
- Cantwell R, Clutton-Brock T, Cooper G, et al. Saving Mothers Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011;118:1-203.
- Sachs A, Aaronson J, Smiley R. The role of the anesthesiologist in the care of the parturient with cardiac disease. Semin Perinatol 2014;38(5):252-9.
- Siu SC, Sermer M, Colman JM, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001;104(5):515-21.
- Drenthen W, Boersma E, Balci A, et al. Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J 2010;31(17):2124-32.
- Thorne S, MacGregor A, Nelson-Piercy C. Risks of contraception and pregnancy in heart disease. Heart 2006;92(10):1520-5.
- Balci A, Sollie-Szarynska KM, van der Bijl AGL, et al. Prospective validation and assessment of cardiovascular and offspring risk models for pregnant women with congenital heart disease. Heart 2014;100(17):1373-81.
- Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition). Reg Anesth Pain Med 2010;35(1):64-101.
- Butwick AJ, Carvalho B. Anticoagulant and antithrombotic drugs in pregnancy: what are the anesthetic implications for labor and cesarean delivery? J Perinatol 2011;31(2):73-84.
- Elkayam U, Goland S, Pieper PG, et al. High-Risk Cardiac Disease in Pregnancy: Part I. J Am Coll Cardiol 2016;68(4):396-410.
- Langesaeter E, Dragsund M, Rosseland LA. Regional anaesthesia for a Caesarean section in women with cardiac disease: a prospective study. Acta Anaesthesiol Scand 2010;54(1):46-54.