Successful Treatment of a Traumatic Brain Injury Patient through Neurosurgery
Received: 28-Mar-2023, Manuscript No. ijav-23-6237; Editor assigned: 01-Mar-2023, Pre QC No. ijav-23-6237 (PQ); Accepted Date: Mar 21, 2023; Reviewed: 14-Mar-2023 QC No. ijav-23-6237; Revised: 21-Mar-2023, Manuscript No. ijav-23-6237 (R); Published: 28-Mar-2023, DOI: 10.37532/1308-4038.16(3).247
Citation: Karl M. Successful Treatment of a Traumatic Brain Injury Patient through Neurosurgery. Int J Anat Var. 2023;16(3):267-268.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
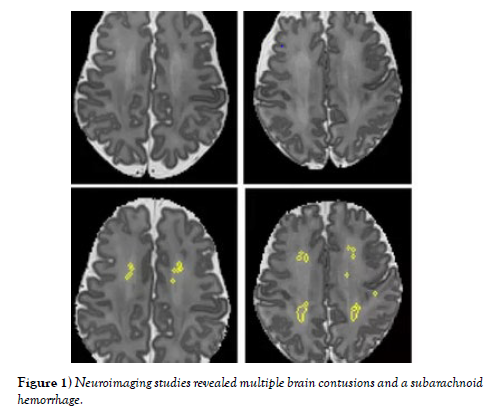
This case report describes the successful neurosurgical treatment of a patient who suffered a severe traumatic brain injury (TBI) following a motor vehicle accident. The patient was admitted to the hospital with a Glasgow Coma Scale (GCS) score of 4, indicating severe neurological impairment. Neuroimaging studies revealed multiple brain contusions and a subarachnoid hemorrhage. A multidisciplinary team consisting of neurosurgeons, neurologists, and critical care specialists was assembled to provide the best possible care for the patient. After initial stabilization, the patient underwent emergency neurosurgery to evacuate a large subdural hematoma and to decompress the brain. The patient remained in a medically induced coma for several days following surgery to allow for optimal brain healing. Over the course of several weeks, the patient underwent intensive rehabilitation and was able to make significant gains in neurological function.
At the time of discharge from the hospital, the patient had made a remarkable recovery and was able to return to work and resume normal daily activities. This case demonstrates the importance of prompt and effective neurosurgical intervention in the treatment of severe traumatic brain injuries.
Keywords
Traumatic brain injury; Neurosurgery; Subarachnoid hemorrhage; Subdural hematoma; Brain
INTRODUCTION
Traumatic brain injury (TBI) is a leading cause of death and disability worldwide, with an estimated 69 million cases occurring annually. The severity of a TBI can range from mild to severe, and in severe cases, can result in significant neurological impairment and long-term disability. Neurosurgical intervention is often required in severe cases to relieve intracranial pressure and prevent further brain damage [1].
CASE REPORT
A 32-year-old male was brought to the emergency department following a motor vehicle accident. On arrival, he had a GCS score of 4, indicating severe neurological impairment. Neuroimaging studies revealed multiple brain contusions and a subarachnoid hemorrhage. A multidisciplinary team consisting of neurosurgeons, neurologists, and critical care specialists was assembled to provide the best possible care for the patient. After initial stabilization, the patient underwent emergency neurosurgery to evacuate a large subdural hematoma and to decompress the brain [2] (Figure 1).
Figure 1: Neuroimaging studies revealed multiple brain contusions and a subarachnoid hemorrhage.
Post-surgery, the patient was placed in a medically induced coma for several days to allow for optimal brain healing. Over the course of several weeks, the patient underwent intensive rehabilitation and was able to make significant gains in neurological function. Outcome: At the time of discharge from the hospital, the patient had made a remarkable recovery and was able to return to work and resume normal daily activities. Follow-up neuroimaging studies showed significant resolution of brain contusions and no evidence of further hemorrhage [3].
DISCUSSION
Traumatic brain injury (TBI) is a devastating condition that can lead to a range of physical, cognitive, and emotional impairments. Treatment of TBI is complex and requires a multidisciplinary approach involving various medical specialties, including neurosurgery. Neurosurgery is a medical specialty that deals with the prevention, diagnosis, and treatment of disorders of the nervous system, including the brain and spinal cord. In the case of TBI, neurosurgery may involve various surgical interventions, such as decompressive craniectomy, hematoma evacuation, and repair of skull fractures. The successful treatment of a TBI patient through neurosurgery depends on several factors, including the severity and location of the injury, the age and overall health of the patient, and the timely intervention and management of the injury [4-5].
CONCLUSION
A successful treatment of a traumatic brain injury patient through neurosurgery would typically involve several key factors. First, the patient would need to receive prompt and appropriate medical attention, which may include emergency care to stabilize the patient’s condition and imaging tests to assess the extent of the injury. Once the patient is stable, neurosurgery may be performed to address any structural damage or bleeding within the brain. This could involve removing any blood clots or repairing damaged blood vessels, or removing any damaged tissue to reduce pressure on the brain. After the surgery, the patient would receive intensive rehabilitation to help them regain lost functions and skills, such as speech and motor skills. This may include physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation.
ACKNOWLEDGEMENT:
None.
CONFLICTS OF INTEREST:
None.
References
- Tantanapornkul W, Kiyoshi O, Yoshikuni F, Masashi Y. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 103(2):253-259.
- Jones AV. Craig GT. Franklin CD. Range and demographics of odontogenic cysts diagnosed in the UK over a 30 year period. J Oral Pathol Med. 35(8):500-700.
- Rood JP, Shehab N. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 28(1):20-25.
- Sarikov R, Juodzbalys G. Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res. 29; 5(4):e1.
- Maegawa H, Sano K, Kitagawa Y. Preoperative assessment of the relationship between the mandibular third molar and mandibular canal by axial computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 96(5):639-46.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref