Successful treatment of an acute sub-massive pulmonary embolism in a renal transplant patient with thrombolytic of low dosage in low infusion protocol
Received: 16-Mar-2018 Accepted Date: Jun 07, 2018; Published: 11-Jun-2018, DOI: 10.4172/2368-0512.1000103
Citation: Akhundova A, Sonmez K. Successful treatment of an acute submassive pulmonary embolism in a renal transplant patient with thrombolytic of low dosage in low infusion protocol. Curr Res Cardiol 2018;5(2):13-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The Pulmonary embolism (PE) incidence is higher in patients with chronic kidney disease and renal transplantation (RT) than in general population. Thrombotic events are multifactorial in renal transplantation recipients and hypercoagulability is the most common factor. We present a case of a 67-yearold renal transplant patient with acute, large thrombus in pulmonary arteries and right heart cavities treated successfully with thrombolytic with low dosage in low infusion protocol.
Keywords
Pulmonary embolism; Renal transplantation; Thrombolytic
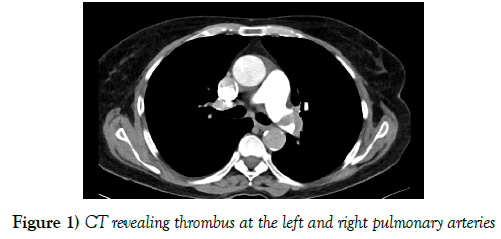
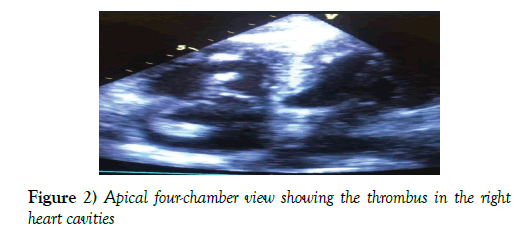
A67-year-old woman was presented with a weeklong chest pain and breathing difficulty. She had a renal transplantation three months ago. She had denied any symptoms after the operation and took drugs-deltacortril 5 mg, prograf 1 mg, certican 0.25 mg, bactrim 400 mg and avalcept 450 mg tb daily. Creatinine level was 1.24 mg/dL and glomerular filtration rate (GFR) was 45. The patient’s O2 was 88% in room atmosphere, breath rate 28 per min, heart rate 120 beat/min, and blood pressure 100/60 mmHg. Laboratory dates was positive: Troponin I (high sensitive) was 0.34 ng/ml, D-dimer was >10.000. Hypoxemia and hypocapnia were seen in Arterial gase analysis: pH 7.31 PaO2 412, PaCO2 47, HCO3 23.3, EB - 3.0, SatO2 99.8%. ECG showed sinus tachycardia with a heart rate of 120 beats/min. Transthoracic echocardiography was performed with a high suspicion of acute pulmonary embolism. TTE showed large, free thrombus moving in right heart cavities. Right heart cavities were dilatated and severe tricuspid regurgitation was revealed with pulmonary artery systolic pressure (sPAB) of 65 mmHg. Pulmonary CT angiography showed an extensive intraluminal and bilateral thrombosis in pulmonary arteries. The diagnosis of acute PE was confirmed. A Doppler ultrasound revealed deep vein thrombosis in right popliteal and crural veins (Figure 1).
Treatment
Because of refractory hypoxaemia and highly repeated embolisation risk of right heart thrombus, thrombolysis treatment decision was taken (Figure 2).
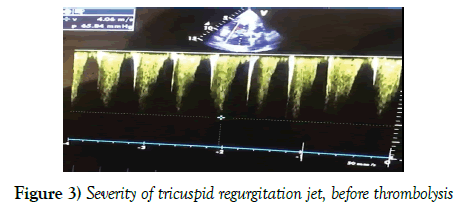
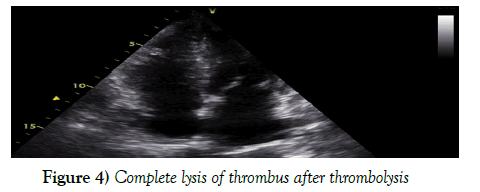
A low dosage of tissue plasminogen activator (tPA) was applied to reduce the risk of bleeding. Slow dose and slow infusion protocol, 2 mg/hour infusion after 10 mg loading dosage were applied. Chest pain and breathlessness were resolved after 24 hours. The O2 level became 100% in room air. She developed a massive hematoma over her right arm after a few hours of thombolytic infusion. Right arm pulses were normal. Hemoglobin level was checked periodically. The patient was haemodynamically stable. No blood transfusion was needed. The size of right heart and systolic pressure normalized and no thrombus in the right heart was seen after 24 hours in control Transthoracic echocardiography study. A 50 mg tPA was enough for a clinical and echocardiographic recovery, the second 50 mg tPA was not given. The hematoma in the right arm was resolved in a few days. He was continued on Coumadin 5 mg tb per day to maintain International Normalized Ratio (INR)-2 to 3. The patient was discharged after a week (Figure 3).
Discussion
PE is common in renal transplant (RT) and patients on dialysis than general population [1]. The disease incidence was 2%-14% and 4.4% of deaths were due to pulmonary embolism after renal transplantation recipients in studies [2,3]. RT patients show a hypercoagulable state, increasing thromboembolic complication. The cause of procoagulable state remains multifactorial. Patient age, prolonged bedrest after transplantation, surgical treatment and pelvic pathology, long time immunosuppressive drugs, antiphospholipid antibodies, and hemoglobin concentration level are important risk factors for thromboembolism [4,5]. Alterations of hemostasis have been demonstrated in relation to immunosuppressive treatment in these patients, in particular to calcineurin inhibitors [5]. In addition, the occurrence of acute CMV infection is reported as a risk factor for the occurrence of venous thromboembolism (VTE) [5]. Pre-transplant dialysis modality, recurrent proteinuria and post-transplant erythrocytosis have also been associated with a hypercoagulable state [5]. Hyperhomocysteinemia is frequently found in RT patients, and increasing evidence exists that homocysteine may affect the coagulation system [6] (Figure 4).
Disease can be present with different clinical manifestation from mild dyspnea to sudden cardiac death. Patients with an acute pulmonary embolism hemodynamically categorized into three subtypes: massive, sub-massive and low risk groups [7]. Patients with massive PE indicate sustained hypotension and shock symptoms. Thrombolysis decreased mortality and recurrent events in massive embolism [8]. Regarding the conflicting date about thrombolysis in sub-massive PE, many trials showed beneficial effect in sub-massive PE [9].
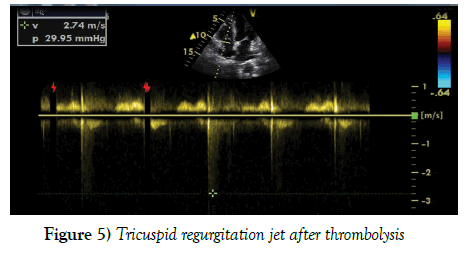
We report the case of a 67-year-old woman with acute pulmonary embolism after renal transplantation three months ago. The patient had not any shock symptoms. PE was categorized as sub-massive due to the presence of right heart dilatation, troponin elevation and severe hypoxemic condition. Bleeding is the most common complication of thrombolytics and this risk is more in renal transplantation in comparison to general population. We administrated 50 mg tPA in slow infusion protocol (for 24 hours) to reduce bleeding complication. The widespread hematoma over the right arm was seen, which resolved within a week and no blood transfusion was needed (Figure 5).
The first case of thrombolytic treatment for acute sub-massive pulmonary embolism and right heart thrombus in renal transplant patient were presented who was successfully treated with thrombolysis.
Conclusion
PE is life threatening disease and thrombolytics may be lifesaving in submassive pulmonary embolism in renal transplant patients.
Competing Interest
The authors declare that they have no competing interests.
REFERENCES
- Sakhuja A, Stephany B, Deitzer D, et al. Trends of pulmonary embolsim before and after kidney transplantation in black versus whites patients. Transplant Proc 2014;46(5):1353-61.
- Advisory committee to the renal transplant registry. The 12 th report of the human renal transplant registry. JAMA 1975;233:787-93.
- European and and dialysis and transplant association. Combined report on regular dyalisis and transplantation in Europe. London Pitman 1983:13.
- Poli D, Zanazzi N, Antonucci E, et al. Renal transplant recipients are at high risk for both symptomatic and asymptomatic deep vein thrombosis. J Thromb Haemost 2006;4(5):988-92.
- Kazory A, Ducloux D. Acquired hypercoagulable state in renal transplant recipients. Thromb Haemost 2004;91:646-5.
- Ducloux D, Motte G, Challier B, et al. Serum total homocysteine and cardiovascular disease occurrence in chronic, stable renal transplant recipients: a prospective study. J Am Soc Nephrol 2000;11:134.
- Management of Pulmonary Embolism: An Update. J Am Coll Cardiol 2016;67:976-90.
- Konstantinides S, Tiede N, Geibel A, et al. Comparison of alteplase versus heparin for resolution of major pulmonary embolism. Am J Cardio 1998;82:966-70.
- Sharifi M, Bay C, Skrocki L, et al. Moderate pulmonary embolism treated with thrombolysis. Am J Cardio 2013;111:273.