Successful Treatment of Aortic Dissection with Open Surgical Repair: A Case Report
Received: 28-Mar-2023, Manuscript No. ijav-23-6238; Editor assigned: 01-Mar-2023, Pre QC No. ijav-23-6238 (PQ); Accepted Date: Mar 21, 2023; Reviewed: 14-Mar-2023 QC No. ijav-23-6238; Revised: 21-Mar-2023, Manuscript No. ijav-23-6238 (R); Published: 28-Mar-2023, DOI: 10.37532/1308-4038.16(3).248
Citation: Karl M. Successful Treatment of Aortic Dissection with Open Surgical Repair: A Case Report. Int J Anat Var. 2023;16(3):269-270.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aortic dissection is a life-threatening condition that requires prompt diagnosis and management. Here we present a case of a 65-year-old male patient who was diagnosed with a Stanford type A aortic dissection. The patient underwent open surgical repair of the ascending aorta, aortic arch, and descending thoracic aorta. The surgery was successful, and the patient had an uneventful postoperative recovery. This case highlights the importance of prompt diagnosis and appropriate management of aortic dissection to achieve favorable outcomes.
Keywords
Aortic dissection; Surgical Repair; Angiogram; Hypothermia
INTRODUCTION
Aortic dissection is a rare but life-threatening condition that occurs due to the tear in the aortic wall, which leads to the formation of a false lumen. The incidence of aortic dissection is estimated to be 2.6 to 3.5 per 100,000 person-years. The condition is associated with high mortality rates if left untreated, with a 50% mortality rate within the first 48 hours. Early diagnosis and prompt treatment are crucial for improving outcomes. Aortic dissection is a life-threatening condition that occurs when the inner layer of the aorta tears, causing blood to flow between the layers and potentially leading to organ damage or even death. While some cases of aortic dissection can be managed with medication and monitoring, others may require surgical intervention [1-3].
One effective method of treating aortic dissection is through open surgical repair, which involves removing the damaged section of the aorta and replacing it with a graft. This procedure is typically performed under general anesthesia and involves making a large incision in the chest to access the aorta. Open surgical repair is generally considered the gold standard for treating aortic dissection, as it allows for complete visualization and repair of the affected area. It is often recommended for patients with complex dissections or those who are at high risk for complications. While open surgical repair is a major procedure that carries some risks, including bleeding, infection, and damage to surrounding organs, it has been shown to be a highly effective treatment for aortic dissection. With appropriate postoperative care, patients who undergo this procedure can expect to experience significant improvement in their symptoms and a reduced risk of further complications [4].
CASE REPORT
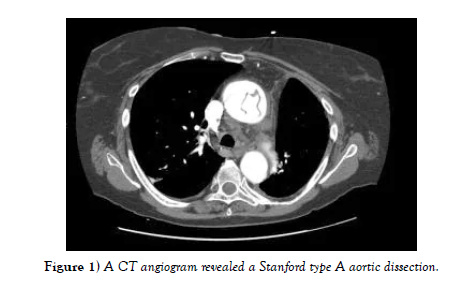
A 65-year-old male patient presented to the emergency department with severe chest pain that started suddenly. He had a history of hypertension, smoking, and hypercholesterolemia. A CT angiogram revealed a Stanford type A aortic dissection, with the intimal flap extending from the aortic root to the descending thoracic aorta [5]. The patient was immediately transferred to the operating room for open surgical repair (Figure 1).
The patient underwent open surgical repair of the ascending aorta, aortic arch, and descending thoracic aorta. The surgery was performed under cardiopulmonary bypass with moderate hypothermia and antegrade cerebral perfusion. The aortic root was replaced with a composite graft, and the aortic arch was repaired with a four-branch graft. The descending thoracic aorta was repaired with a straight graft. The surgery was successful, and the patient had an uneventful postoperative recovery. He was discharged from the hospital on postoperative day 10 and was followed up for six months, during which he remained symptom-free [6-7].
CONCLUSION
Aortic dissection is a rare but life-threatening condition that requires prompt diagnosis and management. Open surgical repair remains the gold standard for treating aortic dissection, particularly in cases of Stanford type A dissection. Early diagnosis and prompt treatment are crucial for improving outcomes and reducing mortality rates [8].
ACKNOWLEDGEMENT:
None.
CONFLICTS OF INTEREST:
None.
References
- Qi L, Xiaojie T, Yafang D. Evaluation of Carotid Plaque Rupture and Neovascularization by Contrast-Enhanced Ultrasound Imaging: an Exploratory Study Based on Histopathology. Transl Stroke Res. 2021 Feb; 12(1):49-56.
- Kuo-Shyang J, Shu-Sheng L, Chiung-FC. The Role of Endoglin in Hepatocellular Carcinoma. Int J Mol Sci. 2021 Mar 22;22(6):3208.
- Anri S, Masayoshi O, Shigeru H. Glomerular Neovascularization in Nondiabetic Renal Allograft Is Associated with Calcineurin Inhibitor Toxicity. Nephron. 2020;144 Suppl 1:37-42.
- Mamikonyan VR, Pivin EA, Krakhmaleva DA. Mechanisms of corneal neovascularization and modern options for its suppression. Vestn Oftalmo. 2016;132(4):81-87.
- Brian M, Jared PB, Laura E. Thoracic surgery milestones 2.0: Rationale and revision. J Thorac Cardiovasc Surg. 2020 Nov; 160(5):1399-1404.
- Amy LH, Shari LM. Obtaining Meaningful Assessment in Thoracic Surgery Education . Thorac Surg Clin. 2019 Aug;29(3):239-247.
- Farid MS, Kristin W, Gilles B. The History and Evolution of Surgical Instruments in Thoracic Surgery. Thorac Surg Clin. 2021 Nov; 31 (4): 449- 461.
- John C, Christian J. Commentary: Thoracic surgery residency: Not a spectator sport. J Thorac Cardiovasc Surg. 2020 Jun; 159(6):2345-2346.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref