Surgical treatment of perforated inferior vena cava filters Two cases
Received: 31-Dec-2020 Accepted Date: Jan 15, 2021; Published: 22-Jan-2021, DOI: 10.37532/1983-8905.2021.14(2).10-11
Citation: Choi CW. Surgical treatment of perforated inferior vena cava filters: Two cases. J Phlebol Lymphol 2021;14(2):10-11.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Inferior vena cava filters are a useful therapeutic option for patients in whom anticoagulant therapy is contraindicated or ineffective, especially those at high risk of bleeding. These filters can erode or penetrate the wall of the inferior vena cava, injuring adjacent retroperitoneal and abdominal organs, especially the duodenum. The perforation rate is estimated to be as high as 4%–40%, although there are no clinical symptoms. We describe two cases: one with a duodenal perforation and another with an inferior vena cava filter transfixed to the lumbar spine (L2 to 3). A brief review of the literature is also provided as is a discussion of the presenting symptoms and treatment regimen for such rare complications.
Keywords
Deep vein thrombosis; Inferior vena cava filters; Intestinal perforation
Introduction
Inferior vena cava (IVC) filters are well known as a useful therapeutic option to prevent pulmonary embolism in patients with deep vein thrombosis, especially those at high risk of bleeding. However, these filters can cause major complications such as thrombus and perforation of the IVC or surrounding organs. We describe, herein, two cases of complications after IVC filter placement: one was a duodenal perforation and the other was an IVC filter transfixed to the lumbar spine (L2 to 3). We also discuss the safety of IVC filter placement and removal.
Case-1
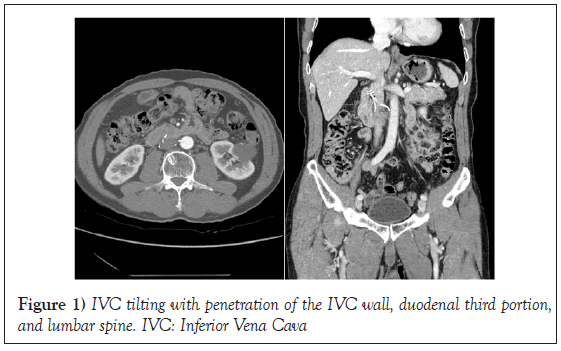
A 68-year-old male was admitted to the emergency room for sudden severe abdominal pain. The patient had been admitted four years prior for dyspnea, hemoptysis, fever, and edema in the left leg and was transferred to a different hospital due to worsening of the edema. He was diagnosed with deep vein thrombosis (DVT) and pulmonary embolism (PE) and underwent IVC filter placement. Anticoagulant therapy was not initiated during the initial hospitalization due to PE, and the patient was treated as an outpatient. He did not regularly come for follow-up and was re-admitted for IVC filter removal after 10 months. The IVC filter was slightly repositioned but not removed during the procedure because it had perforated the IVC and was firmly transfixed into the lumbar spine and the area surrounding the aorta. The patient did not experience any complications until 1 year ago when he reported intermittent abdominal pain and a cycle of constipation and diarrhea. Perforation of internal organs by the IVC filter was suspected; therefore, an abdominal CT scan was performed (Figure 1).
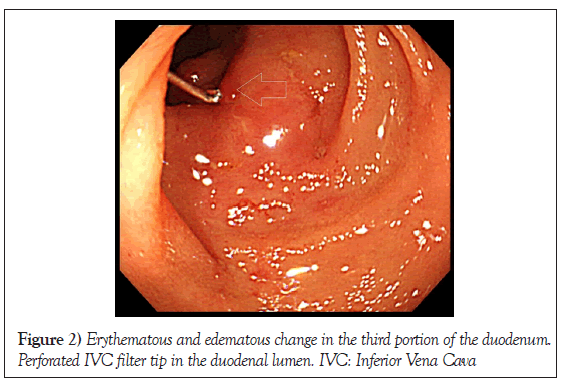
On gastroduodenoscopy, the third portion of the duodenum was found to be perforated by the IVC filter (Figure 2).
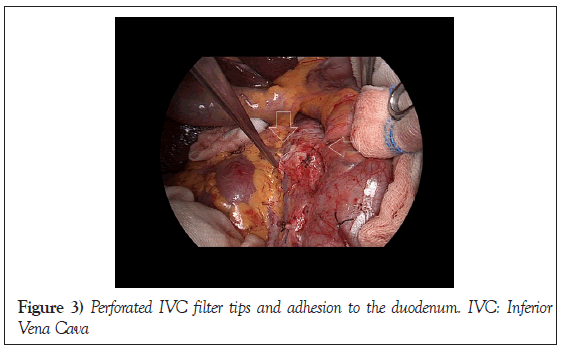
IVC filter removal was deemed necessary, and a laparotomy was performed. Although aortic rupture was suspected, it was not visualized due to adhesions. The IVC filter tip was firmly transfixed to the lumbar spine, and the inflammatory response around the duodenal perforation was not severe. The duodenal perforation was repaired using simple sutures (Figure 3).
After the filter removal, adhesion or neointimal hypertrophy of the IVC were not severe, and the incision on the IVC was repaired with simple suturing. After the surgery, abdominal pain was alleviated, and the patient was discharged on postoperative day 10 without complications.
Case-2
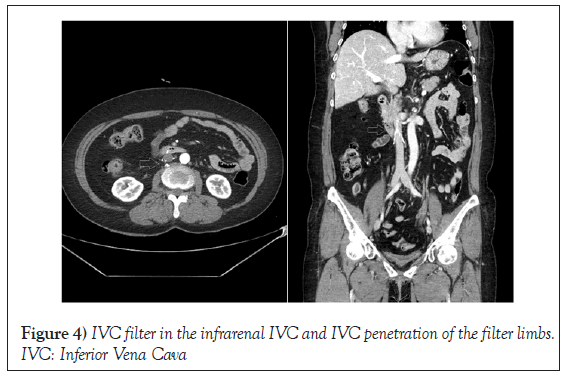
A 57 year-old female was admitted for intermittent abdominal pain and stabbing backache when in the sitting position. The patient had been admitted 10 years prior for left ovarian cystic tumor, approximately 7 cm in size, and edema in the right leg. Abdominal CT imaging showed a thrombus and an occlusion from the right common iliac vein extending down the entire length of the lower leg, and intraperitoneal bleeding was suspected. An IVC filter was placed for ovariectomy. Interventional occlusion removal was attempted on postoperative day 3 since the patient was at low risk of bleeding. Although the thrombotic occlusion in the right common iliac vein was removed and dissolved, the thrombotic occlusion below the femoral vein remained. Anticoagulant therapy was initiated with a vitamin K antagonist. Signs such as edema in the lower extremities were alleviated, but anticoagulant therapy was continued to treat the recurrent occlusion. Due to worsening of the edema in the lower extremities 4 years after IVC filter placement, a CT scan was performed, which revealed an adhesion and a thrombotic occlusion of the IVC. Although the thrombus was dissolved after percutaneous thrombectomy, the perforating IVC and adhesion were not removed. As the patient’s symptoms improved and no other signs of perforation was noted, we decided to do follow-up monitoring for the patient. The patient reported numbness in bilateral lower extremities and an intermittent stabbing backache after 3 years. Since she had an intervertebral disc herniation, we did not suspect that it was caused by the IVC filter, and so we continued to monitor the patient while treating the pain with analgesics and physiotherapy. In the CT scan, thrombotic occlusion in the right iliac vein and lumbar and duodenal perforation by the IVC filter were suspected; therefore, a laparotomy was performed. The IVC filter tip was firmly transfixed into the lumbar spine and no damage to duodenum or other organs was observed. Adhesion of the IVC due to neointimal hypertrophy was noted around the filter insertion site; therefore, IVC angioplasty was performed using an arteriovenous graft. After surgery, backache and abdominal pain were alleviated, and the patient was discharged on postoperative day 8 without complications (Figure 4).
Results and Discussion
Regardless of the types, clinical indicators for IVC filter placement include cases with DVT in whom anticoagulant therapy is contraindicated; other indications include patients with bleeding in vital organs, those that need surgery, and those with thrombocytopenia or PE due to recurrent DVT. A study by Decousus et al. on patients who are likely to develop severe PE from those with DVT in their proximal muscles in the lower extremities compared the effectiveness of PE prevention between a group that received anticoagulant therapy alone and another group that received anticoagulant therapy and IVC filter placement. The results showed that IVC filter placement in conjunction with anticoagulant therapy was the most effective method in the prevention of PE [1]. However, there is no study on the effect of the long-term placement of an IVC filter. Ferris et al. reported the need for long-term observation, but follow-ups with significant clinical implication were reported in only 16% [2]. Another study stated that IVC perforation is found in most cases over time and recommended removing the filter as early as possible [3].
Currently, the IVC filter that is most often used is removable; therefore, it is an appropriate therapeutic option for the prevention of PE in the short term. However, it is actually removed in approximately 50% of cases [4]. The IVC filter may lead to complications such as neointimal hypertrophy (18%), PE that requires interventional surgery or pharmacological therapy (2.27%), and <1 cm PE inside the filter (6.8%). Reviewing a study on IVC perforation or injury, which is one of the long-term complications, showed the following: the complications are asymptomatic in most cases; perforation commonly occurs in the small intestine, ureters, and organs surrounding the IVC; and in some cases, it may progress into complications such as retroperitoneal hemorrhage and intestinal obstruction [5]. In this study, IVC perforation was reported in 4.4% of cases and symptomatic perforation in approximately 0.4% of cases. In a study involving 37 subjects who developed fistula between the IVC and duodenum, the main cause in 10 subjects was identified to be due to perforation by an IVC filter [6]. The fistula was the late complication of the IVC filter placement, and the average fistula development period was 6 years after the surgery. Therefore, IVC filter perforation is commonly reported, but it is rare for IVC filter to perforate vital organs, and it takes a long time to develop symptoms. The only treatment for symptomatic IVC perforation is to remove the IVC filter via laparotomy and to repair the damaged area. Most studies related to duodenal perforation are case reports. Although this study also reports duodenal perforation, these patients were aware of IVC perforation before the symptoms appeared. The difference between asymptomatic patients and patients from this case report is that the filter tip was firmly transfixed into the lumbar spine. Movements such as the pulsing movement of the IVC, breathing, and positional change may displace the IVC transfixed into the lumbar spine and cause duodenal perforation.
Conclusion
IVC filter placement is the most effective therapeutic option for PE prevention, and it yields a positive result when its use is limited. However, its long-term use can lead to complications, even though they are rare; therefore, tests and treatments for patients with susceptible signs and symptoms should be performed proactively for appropriate diagnosis. Surgery such as laparotomy may place burden on patients and healthcare professionals, but it yields the best result as shown in this case report. In addition, long-term placement of an IVC filter should be determined with caution.
Acknowledgments
The author certifies that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
REFERENCES
- Decousus H, Leizorovicz A, Parent F, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. New England Journal of Medicine. N Engl J Med. 1998; 338(7):409-15
- Ferris E, McCowan T, Carver D, et al. Percutaneous inferior vena caval filters: Follow-up of seven designs in 320 patients. Radiology. 1993; 188(3):851-6.
- Durack JC, Westphalen AC, Kekulawela S, et al. Perforation of the IVC: Rule rather than exception after longer indwelling times for the Günther Tulip and Celect retrievable filters. Cardiovascular and Interventional Radiology 2012; 35(2):299-308.
- Rectenwald JE. Vena cava filters: Uses and abuses. Seminars in Vascular Surgery. 2005; 18(3):166-75.
- Streiff MB. Vena caval filters: A comprehensive review. Blood 2000; 95(12):3669-77.
- Guillem PG, Binot D, Dupuy-Cuny J, et al. Duodenocaval fistula: A life-threatening condition of various origins. Journal of vascular surgery. 2001; 33(3):643-45.