Surgical treatment practitioner
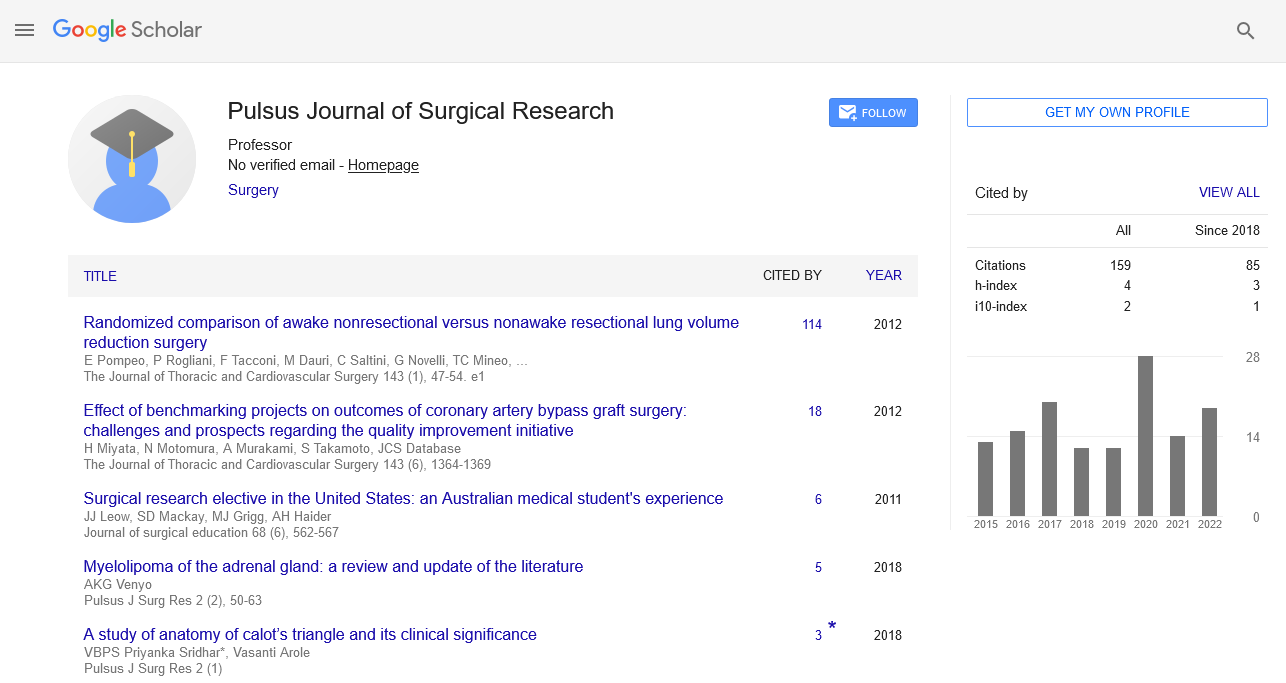
Received: 03-Dec-2022, Manuscript No. pulpjsr- 22-5821; Editor assigned: 06-Dec-2022, Pre QC No. pulpjsr- 22-5821 (PQ); Accepted Date: Dec 26, 2022; Reviewed: 18-Dec-2022 QC No. pulpjsr- 22-5821 (Q); Revised: 24-Dec-2022, Manuscript No. pulpjsr- 22-5821 (R); Published: 30-Dec-2022
Citation: Marry A . surgical treatment practitioner. J surg Res. 2022; 6(6):82-84.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The persistent tension between training and service delivery caused by the European Working Time Directive has made it necessary to reassess the surgical staff and adopt new working practices. Surgical services can be delivered with the assistance of the expanded surgical team. Surgical care professionals are prepared to look after surgical patients along the whole patient pathway, including in clinics, operating rooms, and wards. Due to the flexible nature of the work, they are ongoing members of the surgical team and can support both the service and training. This article provides a general overview of the surgical care practitioner's (SCP) job and how it affects surgical education.
Keywords
Surgical care; Virtual reality; Neuro surgery; Interprofessional collaboration.
Introduction
The National Health Service (NHS) is always changing in order to T meet the sociopolitical, economic, and demographic demands imposed on it in order to provide healthcare in a safe manner. As a result of the introduction of the European Working Time Directive (EWTD), the surgical workforce has been under added logistical strain, making it more difficult to provide safe and effective surgical care. Other healthcare professionals were used by surgeons to support surgical care as a result of a decrease in the number of workers needed to meet service requirements. 1 However, the safety risks connected with using unskilled personnel and performing two roles simultaneously raise the possibility of patient errors and unfavorable results. Therefore, it is crucial that practitioners who support surgical services as a part of the extended surgical team undergo thorough training programmers and examinations. These demands have led to changes in the surgical workforce, including the development of new models for collaborative multi-professional patient care delivery. The training of healthcare professionals for advanced positions, such as the Surgical Care Practitioner (SCP), has been a crucial component. This has been further expanded with the introduction of the Extended Surgical Team (EST), which is currently in a pilot phase. In addition to having an effect on service delivery, EWTD has made it harder for surgical trainees to obtain learning opportunities and the capacity to sufficiently complete curriculum requirements. The role of SCP is frequently unclear among different professions, which could lead to conflict. However, the assistance provided by the SCP function strives to give trainees the time and resources they need to take advantage of additional training options.
During the pilot phase of the Improving Surgical Training (IST) program, the demand for an EST was brought to light. By creating a better training service balance for trainees, IST hopes to raise satisfaction levels and improve training quality. These goals and the surgeons of the future can be supported by the development of the EST. Examining is now taking place for the surgical care practitioner curriculum. The current definition is a registered non-medical practitioner working in clinical practice as a member of the extended surgical team, who performs surgical intervention, pre-operative care, and post-operative care under the direction and supervision of a Consultant surgeon, and who has completed a programmer accredited by the Royal College of Surgeons (or another previously recognized course). The SCP job assists in providing surgical patients with highquality, secure patient care. SCPs can work in all areas of the surgical pathway, including clinics, the ward, the operating room, and on-call. The surgical staff can be more flexible thanks to this range of abilities.
The lack of standardization of the job is one drawback to this, though. Requirements for service delivery, supporting surgical training, corporate culture, and subsequent assistance at work frequently have an impact on the SCP job. Different specialties need assistance with certain patient pathway components According to the SCP curriculum, SCPs may participate as long as they are directed by a consultant surgeon, follow local regulations, and, if necessary, pursue additional qualifications
Clinics that see certain preoperative patients and schedule them for surgical operations while also receiving further training in accordance with regional standards and specifications
Clinical examinations and improved recovery education are two preoperative assessment procedures that the surgical team may order. Setting up suitable preoperative and postoperative investigations as a multidisciplinary team effort would improve patient safety, enable patient-centered care, and support the efficient operation of operating lists.
The consent procedure adheres to local trust or healthcare provider requirements as well as GMC criteria. To support cogent service delivery, liaison with medical, theatre, ward, and clerical staff on pertinent problems, including theatre lists.
Checklist for safe surgery from the World Health Organization. The process of preparing patients for surgery, includes venous puncture, male and female catheterization, and patient positioning. Under the supervision and guidance of the operating surgeon, surgical procedures are performed in the operating room as a member of the multidisciplinary team for the surgical specialty. Working as a first or second assistant during operations as instructed by the supervising surgeon. To support cogent service delivery, liaison with medical, theatre, ward, and clerical staff on pertinent problems, including theatre lists. checklist for safe surgery from the world health organization. the process of preparing patients for surgery, includes venous puncture, male and female catheterization, and patient positioning. under the supervision and guidance of the operating surgeon, surgical procedures are performed in the operating room as a member of the multidisciplinary team for the surgical specialty. working as a first or second assistant during operations as instructed by the supervising surgeon. a range of outpatient tasks, such as seeing patients as and when it is determined that they are capable of doing so. the support of a training session or the provision of delegated care to a patient while the supervising surgeon is leading a training session to facilitate the teaching of trainee surgeons. within their surgical department, they conduct research, development, instruction, and audit. the recommendation of drugs relevant to their particular specialty (if the consultant deems it essential and after receiving the necessary training). the scp role comes with a lot of advantages. it offers practitioners a different career path from management or teaching. As a result, skilled experts who can mentor other allied healthcare workers in the surgical teams remain in the front lines. They are dependable team members that provide continuity of care alongside consultants and associatspecializeded surgeons. They havorganizationalal expertise because they are a permanent team member, which can be very helpful for problem-solving and patient management. They have e vast knowledge of the health system and strong fundamental clinical expertise because they are seasoned practitioners before taking on the SCP post. They also get a comprehension of team dynamics as a result of this. The SCP position is multi-faceted. An experienced registered practitioner is required for application, while the required level of experience may vary. The trainee SCP must decide on a specialty before starting training, and this choice will be reflected in their educational and clinical experiences. Higher education institutes provide a Masters-level SCP course. The program body is made up of both generic and specialtyspecific elements. In their clinical setting, trainee SCPs will be required to demonstrate both their clinical aptitude and their underlying theoretical understanding. To make it more obvious what is expected of a qualified SCP, the present SCP curriculum is being changed. The emphasis will be on collaborating across the patient route and there will be core and specialty-specific components. It will include professional conduct that is in line with the standards of conduct for the SCP trainees' primary profession as well as the framework for generic professional competencies. The clinical supervisor and educational supervisor roles in the existing medical model will be modeled in the supervision models.
The needs of the entire team must be taken into account, recognized, and sensitively addressed during SCP training.
Every team member should receive an equitable amount of training. SCPs will need ongoing professional development after receiving their first training, which calls for more instruction. SCPs are supervised in a manner similar to how surgical residents are supervised. A clinical and educational supervisor is expected for SCPs.
They must create a portfolio of evidence to demonstrate their abilities, which may include evaluations like in-person case-based conversations, mini-clinical evaluation activities, and direct observation of processes. It is crucial to finish the multi-source feedback process and create and keep a logbook. Due to the overlap in requirements for SCPs and surgical trainees, there may be interprofessional conflict that will affect each group's need for training. However, this can be prevented. SCPs are registered practitioners, thus even when they are still in training, they are responsible for their own professional behavior. The SCP's supervision criteria may shift from directly supervised practice to a more independent level of practice with consultant oversight if they are certified and judged competent. The intraoperative component, which includes both assistance and independent operating, is one of the most divisive facets of the SCP function. Surgical trainees are worried that the SCP function may affect their intraoperative training experiences, portfolio creation, and logbook development. The SCP function has as one of its objectives to assist, safeguard, and improve surgical training.
In a statement titled "Trainees should be trainees first and service providers second," the Joint Committee of Surgical Training recommended this approach. The integration of trainee surgeons into the department can be assisted by the organizational knowledge and familiarity of the SCP. A more seamless transition into the department can also be made possible by SCP's knowledge of consultant preferences in the care of patients. The quality of surgical trainees' training can be improved with skilled theatre support. SCPs who are knowledgeable and experienced assistants can enable the learner to receive more concentrated and uninterrupted consultant training. Senior trainees would have greater opportunities to execute procedures independently with the consultant supervising while unscrubbed with an experienced SCP assisting. By enabling more inexperienced surgical trainees to access independent SCP operating lists for training, additional possibilities for training are created. SCPs can assist trainees who have little exposure to or experience with surgery, particularly during time-constrained lists. Depending on the training needs of the trainees, SCPs can assist in the organization of extra training lists. The ability to autonomously conduct and manage the surgical ward round is a prerequisite for SCP training. This can relieve stress on the trainees, especially on days when they must balance training requirements with properly finishing a ward before going to theatres, clinics, teaching, or endoscopy. It would be less necessary for surgical trainees to be excused from the operating room to attend to patients and support the ward if the SCP, who is trained to care for patients along the entire patient pathway, manages patients on the ward in order to assist the surgical trainees. Due to the potential overlap in the scope of practice and training requirements, as well as the misinterpretation of one another's roles, the formation of a professional relationship between the SCP and the trainees can be difficult. The provision of safe and efficient patient care depends on the SCP and trainees having a positive interpersonal working relationship. Additionally, this is necessary for effective teamwork and career advancement.
It is seen as best practice for all disciplines to behave professionally, respect one another's duties in the team, and communicate effectively. Patient care may suffer from poor communication and disagreement within any healthcare team. Different interpretations of the SCP role could perhaps develop as a result of a national deficiency in the implementation of standards Position Confusion may result from this, especially when considering Considering the area of practice, the overlap in both the skill set and Training. There is little advice in the present SCP curriculum on The criteria for a freshly certified scp, as well as the abilities that universal and specialty-specific additional direction for the position and ways in which it can be successfully incorporated into clinical practice would be very helpful and might lessen inter-professional confusion. a lack of comprehension could potentially lead to conflict. each function within the surgical team. however there the positions and training requirements may have some overlap. integral to fulfilling training objectives is team synergy. the provision of high-quality patient care that meets patients' requirements. to gain a clearer understanding of how these functions interact interdisciplinary simulation training's effectiveness is a the crucial need for surgical and scp training recommended. it's critical that all parties involved comprehend the position completely of the scp to make sure they can function properly and efficiently as a part of the surgical team. planning the surgical workforce requires knowledge of the strengths and shortcomings. est roles in order to choose the one that best fits the department's requirements.