Survey of thalassemia major patients receiving regular blood transfusion at day care oncology of a tertiary care hospital in Karachi, Pakistan
Received: 23-Nov-2018 Accepted Date: Dec 26, 2018; Published: 10-Jan-2019
Citation: Aziz A, Khurshid M, Shaheen Z, et al. Survey of thalassemia major patients receiving regular blood transfusion at day care oncology of a tertiary care hospital in Karachi, Pakistan. J Mol Cancer. 2019;2(1):8-10.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: The objective of this study is to identify the reasons behind delays in scheduled blood transfusion, to promote education and awareness of timely blood transfusions in thalassemia major patients and to bring into the notice of physicians the reasons behind delays and how to overcome them.
Material and method: Data for this survey was collected in two parts, from the patient charts, which included demographics of the patients i.e. name,address, phone numbers, e-mail address, medical record number. Laboratory and next follow up plan data was also collected. This is a prospective study,duration of this study was 3 months from April 2017 to June 2017 and 3 months after intervention from June 2018 to August 2018. Inclusion criteria includes patients with thalassemia major, of any age or gender visiting day care oncology at Aga Khan University Hospital for receiving blood transfusion whereas, exclusion criteria includes patients of any age or gender with thalassemia intermediate/minor or other haemoglobinopathies.
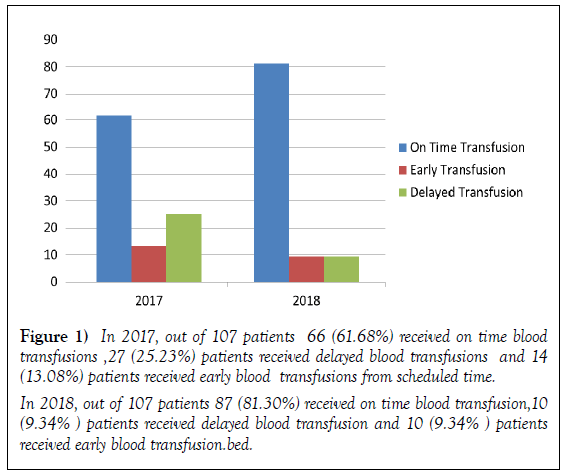
Results: A total of 214 patients were included in this study, in part one out of 107 patients 66 (61.68%) received on time blood transfusions,27 (25.23%)patients received delayed blood transfusions and 14 (13.08%) patients received early blood transfusions. In part two data analysis which was done after intervention, out of 107 patients 87 (81.30%) patients received on time transfusion, 10 (9.34%) patients received early blood transfusion and 10 (9.34%) patients received late blood transfusion. During data analysis it was identified that out of 66 (61.68%) patients coming on time for blood transfusion 38 (57.57%) patients have their Hb level less than 9 g/dL in 2017 and 41 (47.12%) patients out of 87 (81.30%) in 2018 have their Hb level less than 9 g/dL.
Conclusion: In first part before intervention 66 (61.68%) patients were coming on time for blood transfusion and after intervention 87 (81.30 %) patients were receiving timely blood transfusion. Patients receiving on time blood transfusion 38 (57.57%) patients in 2017 and 41 (47.12%) patients in 2018 had hemoglobin level less than 9 g/dL, which needs further workup
Keywords
Thalassemia major; On time blood transfusions; Hemoglobin maintenance level; Educational sessions
Thalassemia is a common hereditary disease. The presence of which culminates in many physical and psychological problems that can affect the quality of life of patients with thalassemia major. If we look globally, in Mediterranean and Southeast Asia countries 5% people are effected which are the carriers of thalassemia gene [1]. Iran falls inside thalassemia zone [2] so that 10% of people living in Caspian Sea margins and southern Iran are the carriers of thalassemia gene. In other regions of Iran, 4 to 8% of people carry the gene [3], Sistan and Baluchistan province accounts for 2600 thalassemia major cases [4] and 197 thalassemia cases in Zabol [5]. In Pakistan the overall carrier rate for thalassemia is 5%-7% however no proper registry is maintained, it is predicted that 5000-9000 neonates are born per annum with thalassemia major, racial group, i.e. Punjabi: 4.5%, Pathan: 5.2%, Sindhi: 1.3%, Baluchi: 9% and Muhajir:5.2% [6,7]. If thalassemia major is not identified and managed timely then patient has to face lot of complications like chronic anemia, bone deformation, growth change, short height and delayed physical maturation [8,9]. Treatment of thalassemia major patient is long term and very costly, regular blood transfusion administration in patients need contribution and financial support of all family members beside cooperation of patient, which is very important. It is seen from the research that without the contribution of the patients, their treatment will not be effective and no satisfactory results will be obtained [10]. Patients when not receiving blood on time due to lack of knowledge of benefits of timely blood transfusion or due to financial burden, leads to complications which not only effect patient’s physical health but this can also cause social harms which in turn increases difficulties of thalassemia patients and their families [11], family members plays a vital role in providing good care for such patients in terms of both physical and mental health [12]. During this study, patients were educated according to Bandura’s theory of self-efficiency, self-care training which can help thalassemia patients and make them accept and engage in managing timely blood transfusion and maintain their hemoglobin level between 9 and 10.5 g/dL [13,14]. This in turn, reduces side effects, increases self-sufficiency and can decrease patients physical problems and promote the quality of life [11,15]. Our main focus is to prevent complications and improve quality of life by convincing patients to receive timely blood transfusion and keep their hemoglobin levels well maintained. Thalassemia is a genetic disorder, which we can effectively manage by regular blood transfusion, to help prevent complications. Diet and exercise may also be helpful, this may help to improve quality of life with increase in duration of lifespan [16].
Materials and Methods
This is a prospective study that took place at day care oncology of The Aga Khan University Hospital Karachi. Total duration of this study was 6 months, 3 months before intervention from April 2017 to June 2017 and after intervention of educational sessions, data was collected from June 2018 to August 2018. Patient’s information was collected from patient’s demographic charts and laboratory results. Patients name, medical record number, age and hemoglobin at the time of admission for blood transfusion was recorded and they were given a scheduled date for their next transfusion. Same patients were followed, whether they came on given date or not and also whether their hemoglobin levels were within range of 9 to 10.5 g/dL or not. Sample size was 107 before and after intervention. Educational sessions were taken twice weekly at day care oncology by physician and head nurse mainly focused on importance of timely blood transfusion. These educational sessions started after first data collection results. Both patients and their attendants were included in educational sessions, emphasizing benefits of timely blood transfusion so as to keep hemoglobin level well maintain. After intervention, data of 107 patients were taken from June 2018 to August 2018 and data analysis was done. This study was approved by Institutional Ethical Review Committee number 4980-Onc-ERC 2017.
Results
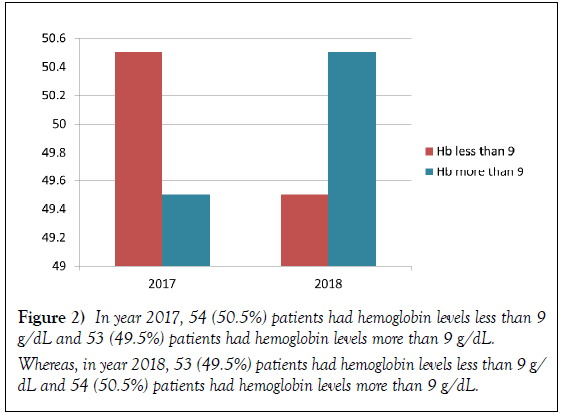
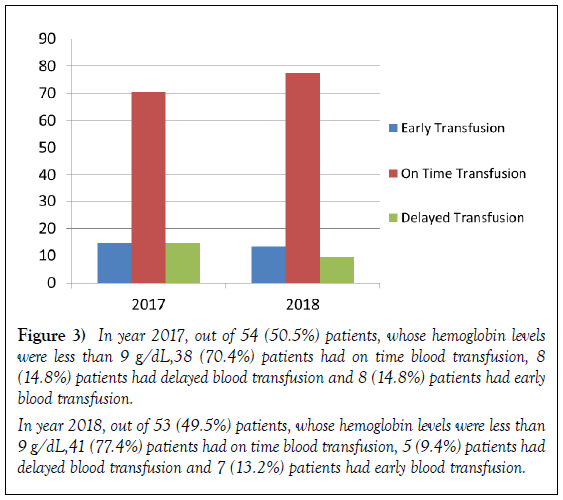
A total of 214 patients were included in this study, in part one out of 107 patients 66 (61.68%) received on time blood transfusions,27 (25.23%) patients received delayed blood transfusions and 14 (13.08%) patients received early blood transfusions from scheduled time. In part two data analysis which was done after intervention, out of 107 patients 87 (81.30%) patients received on time blood transfusion, 10 (9.35%) patients received delayed blood transfusion and 10 (9.35%) patients received early blood transfusion (Table 1a and b and Figure 1). During our survey it was identified incidentally that patients despite of receiving timely blood transfusion were not able to maintain their hemoglobin between 9 to 10.5 g/dL. In year 2017, 38 (57.57%) patients out of 66 (61.68%) patients had their hemoglobin level less than 9 g/L and in 2018, 41 (47.12%) patients out of 87 (81.30%) had their hemoglobin level less than 9 g/dL as shown in Table 2 and Figure 2. Analysis report of 2017, also shows that 8 (14.8%) patients, who received early transfusion have their hemoglobin less than 9 g/dL and 8 (14.8%) patients who received delayed blood transfusion have their hemoglobin less than 9 g/dL, similarly if we compare the results with 2018 data analysis 7 (13.2%) patients who received early blood transfusion have their hemoglobin less than 9 g/dL and 5 (9.4%) patients who received delayed blood transfusion have their hemoglobin less than 9 g/dL (Table 3 and Figure 3). The above analysis report make it very clear that there is an urgent need of regular educational sessions and support group meeting for thalassemia patients and their families and further workup is required for the patients who despite of coming timely for blood transfusion were unable to maintain their hemoglobin level.
Analysis of year 2017 and 2018 Year 2017
| Transfusion | Numbers | Percentage |
|---|---|---|
| On time transfusion | 66 | 61.68% |
| Early transfusion | 14 | 13.08% |
| Delayed transfusion | 27 | 25.24% |
| Total transfusions | 107 | 100% |
Table 1(a) In 2017, out of 107 patients 66 (61.68%) received on time blood transfusions ,27 (25.23%) patients received delayed blood transfusions and 14 (13.08%) patients received early blood transfusions from scheduled time
| Transfusion | Numbers | Percentage |
|---|---|---|
| On time transfusion | 87 | 81.30% |
| Early transfusion | 10 | 09.35% |
| Delayed transfusion | 10 | 09.35% |
| Total transfusions | 107 | 100% |
Table 1(b)In 2018, out of 107 patients 87 (81.30%) received on time blood transfusion,10 (9.34% ) patients received delayed blood transfusion and 10 (9.34% ) patients received early blood transfusion.bed.
Figure 1) In 2017, out of 107 patients 66 (61.68%) received on time blood transfusions ,27 (25.23%) patients received delayed blood transfusions and 14 (13.08%) patients received early blood transfusions from scheduled time.
In 2018, out of 107 patients 87 (81.30%) received on time blood transfusion,10 (9.34% ) patients received delayed blood transfusion and 10 (9.34% ) patients received early blood transfusion.bed.
Analysis of Hb
| YEAR | Hb less than 9 | Hb more than 9 |
|---|---|---|
| 2017 | 54 (50.5%) | 53 (49.5%) |
| 2018 | 53 (49.5%) | 54 (50.5%) |
Table 2In year 2017, 54 (50.5%) patients had hemoglobin levels less than 9 g/dL and 53 (49.5%) patients had hemoglobin levels more than 9 g/dL. Whereas, in year 2018, 53 (49.5%) patients had hemoglobin levels less than 9 g/dL and 54 (50.5%) patients had hemoglobin levels more than 9 g/dL.
Figure 3) In year 2017, out of 54 (50.5%) patients, whose hemoglobin levels were less than 9 g/dL,38 (70.4%) patients had on time blood transfusion, 8 (14.8%) patients had delayed blood transfusion and 8 (14.8%) patients had early blood transfusion.
In year 2018, out of 53 (49.5%) patients, whose hemoglobin levels were less than 9 g/dL,41 (77.4%) patients had on time blood transfusion, 5 (9.4%) patients had delayed blood transfusion and 7 (13.2%) patients had early blood transfusion.
| YEAR | EARLY TRANSFUSION Hb less than 9 |
ON TIME TRANSFUSIONS Hb less than 9 |
DELAYED TRANSFUSIONS Hb less than 9 |
|---|---|---|---|
| 2017 | 8 (14.8%) | 38 (70.4%) | 8 (14.8%) |
| 2018 | 7 (13.2%) | 41 (77.4%) | 5 (9.4%) |
Table 3 In year 2017, out of 54 (50.5%) patients, whose hemoglobin levels were less than 9 g/dL,38 (70.4%) patients had on time blood transfusion, 8 (14.8%) patients had delayed blood transfusion and 8 (14.8%) patients had early blood transfusion.
In year 2018, out of 53 (49.5%) patients, whose hemoglobin levels were less than 9 g/dL,41 (77.4%) patients had on time blood transfusion, 5 (9.4%) patients had delayed blood transfusion and 7 (13.2%) patients had early blood transfusion.
Discussion
Regular blood transfusion throughout life is the treatment for betathalassemia major; blood is usually administered every two to five weeks in order to maintain the pre-transfusion level of hemoglobin between 9 and 10.5 g/dL [8,9]. Timely blood transfusion with maintenance of hemoglobin reassures proper growth, allows normal physical activities, and minimizes the accumulation of transfusional iron [17]. Thalassemia major is the most common genetic disorder on a worldwide basis and needs vigilant close followup to avoid complications [18,19]. It was noticed by physicians at day care oncology of Aga Khan University Hospital that thalassemia major patients are not coming on a scheduled date given to the patients at the time of discharge and are coming late. Day care oncology is a 54 bedded area where we admit patients for cancer chemotherapy drug administrations and thalassemia patients for blood transfusion among other services provided to the patients, approximately 70 patients with thalassemia major were adjusted per week for blood transfusion. After first part of data analysis results showed that only 66 (61.68%) patients are coming timely and out of this 38 (57.57%) patients had hemoglobin which was less than 9 g/dL and in second part of data analysis 41 (47.12%) patients out of 87 (81.30%) receiving blood transfusion on time had hemoglobin level less than 9 g/dL. This result showed that patients despite of coming on time for blood transfusion are not maintaining their hemoglobin levels and it was also observed from data analysis that on average six patients who are either coming early or late from scheduled date also have their Hb level less than 9 g/dL as shown in Table 3. This analysis report is out of our expectations which now need further research to find out why patients are not maintaining their hemoglobin levels. More over as Pakistan is a developing country with low income resources, patients due to financial burden avoid coming early if hemoglobin is low, patients wants to come on schedule time only, even if hemoglobin is low, which is alarming and require urgent need to start convincing patients to keep hemoglobin level between 9-10.5 g/dL. The reasons for delayed blood transfusions from data analysis were because their hemoglobin level was within maintenance levels which is 9-10 g/dl and some had financial issues. Most frequent reason for early blood transfusions was either decrease in hemoglobin levels and in a very few cases school schedule/family travelling issues. There is a strong need of educational sessions for thalassemia patients in day care oncology, in which emphasis should be given on need of early blood transfusion if hemoglobin level is less than 9 g/dL and they should not wait till scheduled date. The aim of present work is to identify how many patients are receiving timely blood transfusion and whether there is any further intervention needed like regular follow up with primary physician. Regular blood transfusion decreases the complications of severe anemia and prolongs survival. Transfusion carries the risk of complications therefore knowing different adverse effects of blood transfusion represent a great issue in managing thalassemic patients [20]. Blood reactions may be acute or chronic which make patients worried and they want to avoid regular blood transfusions therfore there is an immense need of counselling of patients and their families.
Conclusion
After taking educational sessions there is a drastic improvement in percentage of patients receiving timely blood transfusion from 61.68% to 81.30%. During data analysis it was identified that patients receiving on time blood transfusion 38 (57.57%) patients in 2017 and 41 (47.12%) patients in 2018 had hemoglobin level less than 9 g/dL and few patients who received early and delayed blood transfusion also have hemoglobin less than 9 g/dL, which needs further workup.
Way Forward
Patients and family educational sessions about importance of timely blood transfusion in thalassemia patients, so that hemoglobin levels can be well maintained. Identify reasons behind delays and how can we address these issues. Need to identify reasons why, despite of receiving timely blood transfusion good number of patients have hemoglobin less than 9 g/dL.
Acknowledgement
We are grateful to Saba Saleem for helping in collecting patient’s data, Ghulam Rasool for helping in formatting this manuscript and all authors of references we have cited in our manuscript. We would also like to thank patients and their families for participation in educational sessions.
REFERENCES
- Piel FB, Weatherall DJ. The a-thalassemias. N Engl J Med. 2014;371:1908-16.
- Arbabisarjou A, Karimzaei T, Jamalzaei A. The perception of Biological experience in patients with major thalassemia: A qualitative research. Glob J Health Sci. 2015;7:79-87.
- Nazila Rezaei M, Anoosheh Ghasemian D, Gohari K, et al. Burden of Hemoglobinopathies (Thalassemia, Sickle Cell Disorders and G6PD Deficiency) in Iran 1990–2010: findings from the Global Burden of Disease Study 2010. Arch Iran Med. 2015;18:502-7.
- Miri-Moghaddam E, Naderi M, Izadi S, et al. Causes of new cases of major thalassemia in sistan and balouchistan province in South-East of Iran. Iran J Public Health. 2012;41:67-71.
- Shahramian I, Razzaghian M, Ramazani AA, et al. The correlation between troponin and ferritin serum levels in the patients with major beta-thalassemia. Int Cardiovasc Res J. 2013;7:51-5.
- Ahmed S, Petrou M , Saleem M. Molecular genetics of beta-thalassaemia in Pakistan: a basis for prenatal diagnosis. Br J Haematol. 1996;94:476-82.
- Ansari SH, Shamsi TS, Ashraf M, et al. Molecular epidemiology of ß-thalassemia in Pakistan: far reaching implications. Int J Mol Epidemiol Genet. 2011;2: 403-8.
- Hattab FN. Patterns of physical growth and dental development in Jordanian children and adolescents with thalassemia major. J Oral Sci. 2013;55:71-7.
- Wong P, Fuller PJ, Gillespie MT, et al. Bone Disease in Thalassemia: A Molecular and Clinical Overview. Endocr Rev. 2016;37:320-46.
- Muncie HL, Campbell J. Alpha and beta thalassemia. Am Fam Physician. 2009;80:339-44.
- Cappellini MD, Cohen A, Porter J, et al. Guidelines for the management of Transfusion Dependent Thalassaemia (TDT). 3rd ed. Nicosia (CY): Thalassaemia International Federation, 2014.
- Baraz S, Miladinia M, Mosavinouri E. A Comparison of Quality of Life between Adolescences with Beta Thalassemia Major and their Healthy Peers. Int J Pediatr. 2016;4:1195-204.
- Shahdadi H, Balouchi A, Sepehri Z, et al. Factors Affecting Hemodialysis Adequacy in Cohort of Iranian Patient with End Stage Renal Disease. Glob J Health Sci. 2015;8:50-6.
- Kiani F, Balouchi A, Shahsavani A. Investigation of Nursing Students’ Verbal Communication Quality during Patients’ Education in Zahedan Hospitals: Southeast of Iran. Glob J Health Sci. 2016;8:331-6.
- Kiani F, Rahnama M, Dadkani E, et al. A Comparison of Hospital Stressors and their Related Factors: From the Perspective of the Cardiac and Internal Wards’ Patients. IJPCR. 2016;8:80-5.
- Morowatisharifabad M, Tonekaboni NR. Perceived self-efficacy in self-care behaviors among diabetic patients referring to Yazd Diabetes Research Center. J Birjand Univ Med Sci. 2008;15:91-9.
- Borgna-Pignatti C, Cappellini MD, De Stefano P, et al. Survival and complications in thalassemia. Ann N Y Acad Sci. 2005;1054:40-7.
- Gretchen Holm, Kristeen Cherney. Medically reviewed by University of Illinois-Chicago, College of Medicine on April 11, 2017.
- Hazirolan T, Eldem G, Unal S, et al. Dual-echo TFE MRI for the assessment of myocardial iron overload in beta-thalassemia major patients. Diagn Interv Radiol. 2009;16:59-62.
- Katz EA. Blood transfusion: Friend or foe. AACN Adv Crit Care. 2009;20:155-63.