Symphysiolysis and Pregnancy Related Pelvic Girdle Pain – Mystery Resolved?
Received: 28-May-2020 Accepted Date: Aug 11, 2020; Published: 18-Aug-2020
Citation: Pomp G. Symphysiolysis and Pregnancy Related Pelvic Girdle Pain-Mystery Resolved?. J Reprod Biol Endocrinol 2020;4(3):2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Introduction
Symphysiolysis, also referred as Pregnancy Related Pelvic Girdle Pain (PRPGP), is a common disabling illness in pregnancy, incidence ranging from 4% to 76.4%, probably due to lack of agreed definition and the use of different study designs.
Symptoms describedare vast ranging from mild pelvic discomfort to inability to move out of bed.
The diagnosis is mostly clinical. Imaging of the symphysis pubis joint can be performed by US or MRI.
Current treatments mainly include oral pain medications, NSAID’s (until 28-30 week of pregnancy, Pelvic Support belt, physiotherapy, hydrotherapy, lifestyle modifications, and bed rest. More severe cases are treated by local injection of steroids and local anesthetic agents to into the pelvic joint or around it - done in “pain clinics”.
Extreme cases demand surgical interventions or constant regional nerve block such as epidural analgesia [1-7].
The highly respected British Medical Journal published a 'letter to the editor' of a medical doctor telling her story of having an enormous painduring pregnancy, while getting no answers whatsoever from the conventional medicine. She describes her experience with integrative/ alternative medicine (such as acupuncture). She states that overall, there was a small reduction in pain, but at least she did not need to increase the analgesia throughout the pregnancy. It was relaxing andcomforting to know that someone cares [8]. Case reports of innovative medical approaches for rapid pain relief described using epidural analgesia as early as 20th week of gestation, and using bedside ultrasound guided intra-articular symphysis pubis injection [1-9].
Mostly, PRPGP is a self-limited condition - 93% reported symptoms settled within 3 months postdelivery. There is tendency for reoccurrence in next pregnancies with higher intensity. A few would have a persistent form which leads to a lifetime disability. In these very severe cases, extreme interventions are described, such as pelvic-joint-fusion [4].
My Perspective
As an obstetricianin 'high risk pregnancy' (HRP) clinic, I occasionally met patients with complaints of groin and / or lower back pain. As my colleagues, I prescribed bed rest, physiotherapy exercises, orthopedic consultation, oral analgesics such as paracetamol and dipyrone. I emphasized NSAID's could be used as a second-line treatment, but only until 30th week of gestation due to fetal safety issues (premature closure of the ductus arteriosus vessel). I recommended pelvic or abdominal supporting belts, since I heard physiotherapist use that practice, and referred them to physiotherapy clinics to get the instructions on how exactly to use these support belts. Mostly I wondered why they came to me, since pelvic pain is not my expertise nor field of interest. Of course I knew the real reason they came to the HRP clinic - they needed me to sign the papers for the social insurance "disability" claim. Not only had I felt they were wasting my time, I also felt being used.
I felt sorry for those in pain and quoted that "pregnancy is not a disease", explaining that these are physiologic changes related to widening of the pelvic joint, caused by the relaxin hormone [10].
I still remember the feeling of incompetencywhen a patient informed me she uses diapers at night since she could not get out of bed to get to the toilet.
Still, I could offer her empathy, recommend pain killers and bed rest, and sign the form for the insurance claim.
An Incidental Observation
In years 2013-2014 I was head of maternal ward in LaniadoHospital located in Netanya, Israel. I was told of a patient that could not move out of bed since her delivery. We gave her all painkillers available, including morphine derivatives (such as tramadol) that helped for a while or at least enabled her to sleep. Later the pain recurred, she was treated again, had some relief or fell asleep, and so on. The source of pain was the symphysis pubis joint, as easily demonstrated but lightly palpating that location. Computed Tomography imaging showed no abnormality.
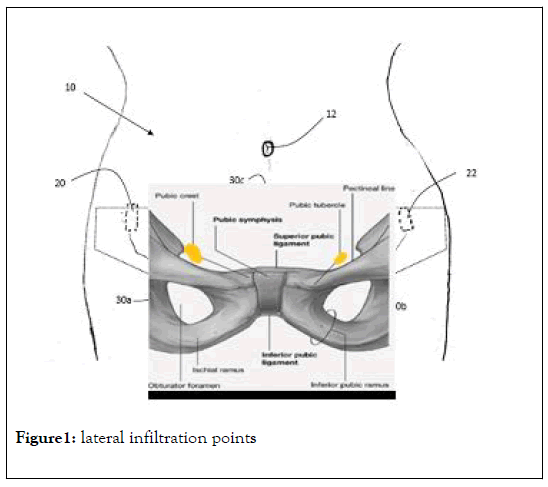
In the Jewish tradition a festive event is performed in the eighth day. Since that patient was bed ridden,she was not discharged from maternity ward (though she was more of an orthopedic patient). I tried to figure out if there was anymeasure that could enable her to attend her celebrations. Searching pubmed.comformanagement of 'acute symphysis pubis dysfunction', or 'symphysiolysis'showed that the only intervention for a rapid pain relief was injection of local anesthetics such as lidocaine into the symphysis pubis joint, as published by Schwarz et al. in 1985 [11-13] (Figure 1).
Since that technique was absent from the obstetrics and gynecology literature for 30 years afterwards, it seemed imprudent to use. Nevertheless, local infiltration of bupivacaine in the vicinity of the joint seemed like a possible alternative, if only for a few hours. It was decided to offer that treatment for a temporary pain relief, to enable the patient to leave the ward for 3 to 4 hours and return afterwards for pain management and more evaluation of the differential diagnosis.
Since the area around the pubic bone was very tender, it was impossible to inject at that location, so instead we planned to enter the skin 5 cmlaterally from both sides and to approach the pubic region subcutaneously byusing a large bore needle (such as used for spinal anesthesia). All was set for the unconventional compassion treatment, informed consent was granted and as we cleansed the area preparing for the procedure, it seemed like a good idea to infiltrate the injection sites with a small amount of rapid-onset local anesthesia (lidocaine 1%), since we were using a large bore needle. Immediately after the application of subcutaneous lidocaine (1%, 1 ml) given as a pre-treatment and just before approaching with the actual bupivacaine treatment, the patient stood up from the bed by herself and began to walk with no pain. That surprising observation that was repeated in a similar scenario few months later with a similar patient, led to the hypothesis that signals of pain were conducted by nerves from the pubic bone, laterally. It was presumed that branches of the Ilio-inguinal or Genitofemoral nerves were involved [14]. I assumed that the anesthetic fluid drained through the subcutaneous plane towards the pubic regionin a manner similarto the accumulation of blood in the vulva ("vulvar hematomas") occasionally seenafter laparoscopic operations, affecting nerve fibers emerging from the inguinal canal through the superficial inguinal ring.
Implementation in Pregnancy
That observation and the proposed mechanism remained undocumented becauseit had no support in thepublished literature. A properly designed prospective study could not be approved in pregnant subject, since there wereno grounds in the literature for such approach. 5 years later, a severe case of pelvic pain in pregnancy renewed the interest in that incidental observation.
A patient with a known chronic pain disorder (CRPS - chronic regional pain disorder) presented in 29th gestational week of her first pregnancysuffering from anterior pelvic pain that appearedearly in the second trimester. She was unable to walk at all and was confined to a wheelchair from 24th gestational week. Her pain was constant and unbearable to the level she asked to be 'relieved' of herpregnancy. All supporting management was ineffective. I described my old observation and offered to perform it a as compassion treatment, if approved as such by an academic medical center, and performed within its boundaries.
The director of pain clinic in Hadassah Medical Center, Prof. Elyad Davidsonoffered his support, stating that the known alternative he could offer her in pregnancy is continuous epidural analgesia. Therefore, using the same medications (lidocaine, bupivacaine) for the same indication, applied in a subcutaneous route without the risks of invasive reginal anesthesia, is a preferred therapy.
On October 31st 2018 "patient zero" received subcutaneous injection of 5 ml lidocaine 1%, at mid-inguinal location, bilaterally. 5 minutes later she was able to leave her wheelchair and to walk by herself with no pain (video attached elsewhere). On the same day, Maccabi Health Services permitted subcutaneous anesthesia as a treatment for pregnant women with severe pelvic girdle pain, as an alternative to invasive epidural analgesia.
Since then, during a period of 19 months (31/10/2018 to 25/5/2020) a total of 116 pregnant patients undergone 409 treatmentsof subcutaneous anesthesia for PRPGP. Insight derived from these treatments, including the optimal combination of local anesthetics (lidocaine and bupivacaine), the exact technique of injection, the methods used to achieve longer pain relief (up to 14 days) will be presented in another paper.
REFERENCES
- Desmond FA, Harmon D. (2010) Ultrasound-guided symphysis pubis injection in pregnancy. Anesth Analg 111: 1329-1330.
- Díaza RR, Riverab AL. (2012) Management of non-obstetric pain during pregnancy, Review article Rev. colomb. Anestesiol 40: 3.
- Albert HB, Godskesen M, Westergaard JG. (2002) Incidence of Four Syndromes of Pregnancy-Related Pelvic Joint Pain. Spine 27: 2831-2834.
- Kanakaris NK, Roberts CS, Giannoudis Pv. (2011) Pregnancy-related pelvic girdle pain: An update. BMC Med 9.
- Vermani E, Mittal R, Weeks A. (2010) Pelvic girdle pain and low back pain in pregnancy: A review. Pain Pract 10: 60-71.
- Scicluna JK, Alderson JD, Webster VJ, Whiting P. (2004) Epidural analgesia for acute symphysis pubis dysfunction in the second trimester. Int J Obstet Anesth, 13: 50–52.
- Casagrande D, Gugala Z, Clark SM, Lindsey RW. (2015) Low Back Pain and Pelvic Girdle Pain in Pregnancy. J Am Acad Orthop Surg 23: 539-549.
- Manickasamy K. (2018) Patient Commentary: I was pregnant, in pain, and desperate when i chose acupuncture. The BMJ 360.
- Scicluna JK, Alderson JD, Webster VJ, Whiting P. (2004) Epidural analgesia for acute symphysis pubis dysfunction in the second trimester. Int J Obstet Anesth, 13: 50–52.
- Gabbe S. (2012) textbook of obstetrics, 6thedition. Saunders 1312.
- Norvilaite K, Kezeviciute M, Ramasauskaite D, Arlauskiene A, Bartkeviciene D, et al. (2020) Postpartum pubic symphysis diastasis-conservative and surgical treatment methods, incidence of complications: Two case reports and a review of the literature. World J Clin Cases 8: 110–119.
- Hou Z, Riehl ZT, Smith WR, Strohecker KA, Maloney PJ. (2011) Severe postpartum disruption of the pelvic ring: report of two cases and review of the literature. Patient Saf Surg 5: 2.
- Schwartz Z, Katz Z, Lancet M. (1985) Management of puerperal separation of the symphysis pubis. Int J Gynecol Obstet 23: 125-128.
- Marcovici ISE. (2001) Operative laparoscopy and vulvar hematoma: an unusual association. JSLS 5: 87–88.