TAVR-in-TAVR procedure on a patient with cardiogenic shock due to a degenerated corevalve
2 Hospital Meridional, Cariacica-ES, Brazil
3 Hospital Evangelico, Vila Velha-ES, Brazil
4 Instituto do CoraçãoINCOR, São Paulo-SP, Brazil
Received: 24-Sep-2022, Manuscript No. puljhr-22-5409; Editor assigned: 28-Sep-2022, Pre QC No. puljhr-22-5409 (PQ); Accepted Date: Oct 23, 2022; Reviewed: 11-Oct-2022 QC No. puljhr-22-5409 (Q); Revised: 20-Oct-2022, Manuscript No. puljhr-22-5409 (R); Published: 26-Oct-2022, DOI: 10.37532/ puljhr.2022.5(5).01-03
Citation: Arruda JAD, Neto ANF, Machado BM, et al. TAVR-In-TAVR procedure on a patient with cardiogenic shock due to a degenerated corevalve. Int J. Heart Res. 2022; 5(5):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
While Transcatheter Aortic Valve Replacement (TAVR) has expanded accept changas a treatment for symptomatic aortic valve stenosis, little is known about its long-term outcomes. We present a 92-years-old female presenting with cardiogenic shock due to an 8-years-old degenerated transcatheter heart valve submitted to life-saving balloon valvuloplasty and redo TAVR.
Keywords
Aortic stenosis; Acute heart failure; TAVR-in-TAVR
Introduction
A 92-years-old female patient was admitted to the emergency department with chest pain and acute pulmonary edema, progressing within 12 hours with pale skin, diaphoresis, hypotension, and acute renal oliguric failure. The ECG presented a complete left bundle branch block and first-degree atrioventricular block.
Case Presentation
Past medical history
She had a Transcatheter Aortic Valve Replacement (TAVR) with a 26-mm CoreValve (Medtronic, Santa Rosa, California) Transcatheter Heart Valve (THV) 8 years prior to her admission to treat severe aortic stenosis, as well as a percutaneous coronary intervention to her right coronary, left circumflex and left anterior descending coronary arteries.
Previous investigations
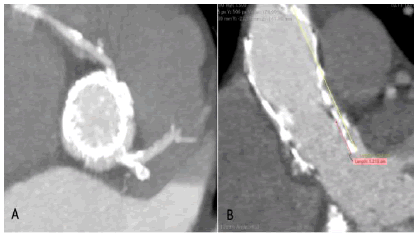
Before hospital admission, she was submitted to a Transesophageal Echocardiogram (TEE) that unveiled severe THV stenosis with a mean pressure gradient of 80 mmHg. The severity of the THV stenosis was confirmed with cardiac catheterization and hemodynamic measurements. The cardiac tomography revealed an advanced degenerative process in THV, with leaflets’ calcification adjacent to both coronary arteries ostia (Figure 1).
Thus, a TAVR-in-TAVR procedure was proposed, with the performance of a basilica technique as to minimize the risk of coronary obstruction and the placement of a balloon-expandable valve in the lowest possible position within the aortic annulus and left ventricular outflow. Unfortunately, while waiting for the suggested procedure, the patient was admitted to the hospital in critical clinical condition
Management
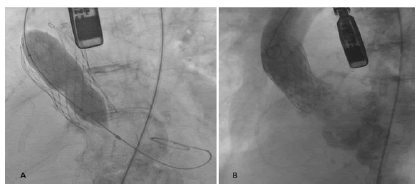
In the first 12 hours of hospital admission, cardiogenic shock was present and no THVs were available, therefore, the patient was submitted to a life-saving aortic balloon valvuloplasty (Figure 2A). The induction of general anesthesia worsened her hemodynamic profile, requiring a rapid infusion of intravenous vasoactive drugs. The procedure was performed under fluoroscopic and TEE guidance with rapid pacing and a 22 mm Atlas Gold balloon. Post-valvuloplasty, the patient developed severe acute aortic regurgitation (Figure 2B).
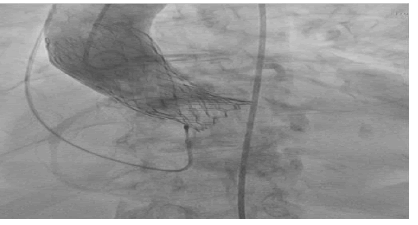
The patient was kept in mechanical ventilation and continuous infusion of vasoactive drugs at the Coronary Care Unit (CCU) for approximately 6 hours until a new THV was available for implantation. Just before the TAVR-in-TAVR procedure, the patient had a cardiac arrest in asystole, demanding 9 minutes of resuscitation. A 23-mm Edwards Sapien 3 (Edwards Lifesciences, Irvine, CA) was deployed in a very deep position (Figure 3), as compared to the standard technique, to reduce the risk of coronary obstruction, guided by fluoroscopy and with right ventricular pacing at 180 beats/min
Figure 3: Aortic Angiography After Valve Deployment Showing Deeply Positioned 23-mm Edwards Sapien 3
TEE and post-deployment aortogram showed a low THV with no perivalvular leaks, and despite its final position, there was no impairment of the mitral valve apparatus. The mean aortic gradient was 6 mmHg at the end of the procedure. The patient was transferred to the CCU with a complete heart block and dependent on a transvenous pacemaker, most likely due to the very deep THV implantation. On the following day, a dual chamber permanent pacemaker was implanted. The patient remained in mechanical ventilation for 5 days, and paroxysmal atrial fibrillation was noticed. After 12 days of admission, she was discharged with full recovery of the renal function, in sinus rhythm, and no more complications were registered
Follow up
The patient was seen at one-month follow-up with a good clinical condition, and a mean aortic gradient of 10 mmHg, with an aortic valvular area estimated in 1.7 cm2 by transthoracic echocardiogram.
DISCUSSION
TAVR has been placed as the gold standard treatment for symptomatic severe aortic stenosis after multiple randomized clinical trials have demonstrated TAVR to be either non-inferior or superior to surgical aortic valve replacement in short- and mid-term outcomes [1-3]. While the number of TAVR procedures is rapidly growing regardless of STS risk scores, some concerns regarding heart rhythm complications and specially THV durability remain. Thus, the durability question remains more than ever on the top of the agenda [4,5]. Further apprehensions are observed in the setting of valve-invalve procedures, such as coronary obstruction particularly when selfexpandable THVs are to be treated by TAVR-in-TAVR, and these concerns must be taken into account before deciding to move forward with the procedure [6]. The reported case of a 92-years-old female with an 8-year-old degenerated CoreValve illustrates these relevant and increasingly common TAVR concerns, particularly that regarding the potential for the degeneration of THVs implanted in the setting of a TAVR-in-TAVR procedure and in those patients with an ever more present increased life expectancy. As of today, how to eliminate coronary obstruction in the TAVR-in-TAVR population are still an unanswered question.
We added in this report a solution not anticipated of destroying an old THV leaflet with balloon valvuloplasty and implanting a new one in a lower position to avoid coronary obstruction.
Conclusion
Some lessons could be observed in this case report:
1. Aortic balloon valvuloplasty in THV to treat aortic stenosis as a life-saving procedure can cause severe aortic insufficiency.
2. The treatment of an old THV with structural degeneration through redo TAVR could represent a challenge in certain anatomies.
Abbreviations
TAVR: Transcatheter Aortic Valve Replacement, TEE: Transesophageal Echocardiogram, CU: Coronary Care Unit
References
- Thyregod HG, Steinbruchel DA, Ihlemann N, et al. Transcatheter Versus Surgical Aortic Valve Replacement in Patients With Severe Aortic Valve Stenosis: 1-Year Results From the All-Comers NOTION Randomized Clinical Trial. J Am Coll Cardiol. 2015;65:2184-94.
- Bonow RO, Carabello B, de Leon Jr AC, et al. Guidelines for the management of patients with valvular heart disease: executive summary A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Valvular Heart Disease). Circulation. 1998 Nov 3;98(18):1949-84
- Gleason TG, Reardon MJ, Popma JJ, et al. 5-Year Outcomes of Self-Expanding Transcatheter Versus Surgical Aortic Valve Replacement in High-Risk Patients. J Am Coll Cardiol. 2018;72:2687-96.
- Jorgensen TH, De Backer O, Gerds TA, et al. Mortality and Heart Failure Hospitalization in Patients With Conduction Abnormalities After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2019;12:52-61.
- Sawaya F, Jorgensen TH, Sondergaard L, et al. Transcatheter Bioprosthetic Aortic Valve Dysfunction: What We Know So Far. Front Cardiovasc Med. 2019;6:145.
- Bernardi F L M, Dvir D, Rodes-Cabau J, et al. Valve-in-Valve Challenges: How to Avoid Coronary Obstruction. Front Cardiovasc Med. 2019;6:120.