The aspartate aminotransferase platelet count ratio index (APRI) as an ideal predictor of dengue severity
Received: 18-Jan-2023, Manuscript No. puljcmid-23-6062; Editor assigned: 20-Jan-2023, Pre QC No. puljcmid-23-6062 (PQ); Reviewed: 03-Feb-2023 QC No. puljcmid-23-6062; Revised: 17-Apr-2023, Manuscript No. puljcmid-23-6062 (R); Published: 24-Apr-2023
Citation: Nagarjuna P. The Aspartate aminotransferase Platelet count Ratio Index (APRI) as an ideal predictor of dengue severity. J Clin Microbiol Infect Dis 2023;6(1):1-5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Purpose of the research: Now a days, majority of dengue patients with an abnormal Aspartate amino Transferase (AST) level, and a decreased blood Platelet count (PLT) is linked to the severity of dengue fever. However, just a few researchers, assessed its predictive relevance for determining the severity of dengue. Hence, we aimed to assess the diagnostic value of Aspartate Aminotransferase/Platelet count Ratio Index (APRI) for predicting dengue severity.
Methods: A prospective study done among 115 patients with confirmed dengue fever (ELISA based NS1 antigen/IgM antibody positive report) who were admitted in tertiary care hospital from June 2021 to December 2021. All patients were clinically assessed and investigated for serum transaminases and platelet count on day 1, day 4 and day 7 or on the day of discharge/ death. Data was analysed using Microsoft excel and SPSS version 21.
Results: A total of 115 patients, 76 (66.1%) males and 39 (33.9%) females, with the median age of the patients were 27 years (range from 15-45). Most of the patients (65, 56.5%) had dengue fever without warning signs and 20 patients (17.4%) had severe dengue disease. The aspartate aminotransferase (AST), leukocyte count, Platelet count (PLT), aspartate Aminotransferase/Platelet count Ratio Index (APRI) showed a significant association with severe dengue (p<0.05). With the observed 2.5 cut off value, we found the sensitivity and specificity of APRI for prediction of dengue severity as 80.0%and 76.8% respectively.
Conclusion: Our study revealed that Aspartate aminotransferase/Platelet count Ratio Index (APRI), can be useful for clinicians to predict the severity of dengue fever infection during the onset of symptoms and course of treatment for better outcome.
Keywords
Aspartate; Platelet count; APRI; Ideal; Predictor; Dengue; Severity
Introduction
Dengue fever is one of the important Neglected Tropical Diseases (NTDs) that poses a public-health concern and threat globally and national wide [1]. Global prevalence has risen dramatically, with nearly half of the world's population now at risk. Although 100-400 million infections are estimated to occur each year, more than 80% are generally mild and asymptomatic. Despite the fact that there is a risk of infection in 129 countries, Asia bears 70% of the actual burden. The number of dengue cases reported to WHO has more than doubled in the last two decades, while the total number of cases appears to have decreased in the years 2020 and 2021, as well as for reported deaths. However, this might be attributed to COVID-19 pandemic in view of reporting in several countries [2].
Dengue is a mosquito borne viral caused by dengue virus of the Flaviviridae family and there are four distinct, but closely related, serotypes of the virus that cause dengue (DENV-1, DENV-2, DENV-3 and DENV-4) that can transmitted by female mosquitoes mainly of the species Aedes aegypti and to a lesser extent, Aedes albopictus. The risk of dengue varies locally depending on local climate, social, and environmental factors, which are both common in the tropics. Prior to a few decades, dengue fever was primarily urban based, but it is now also being reported from peri-urban and rural areas [3].
Dengue fever is a wide spectrum of disease ranges from subclinical disease to severe flu like symptoms in those infected. The WHO classified symptomatic dengue virus infection in 1997 as Dengue Fever (DF), Dengue Haemorrhagic Fever (DHF), and Dengue Shock Syndrome (DSS). The revised WHO classification of 2009 categorizes dengue patients according to different levels of severity as dengue without warning signs, dengue with warning signs (abdominal pain, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy, liver enlargement, and increasing haematocrit with decreasing platelets) and severe dengue. Dengue/severe dengue have no specific treatment. Early detection of disease progression associated with severe dengue and access to proper medical care reduces severe dengue fatality rates to less than 1%. Severe dengue has a higher risk of hospitalisation and death if not treated properly [4,5].
Recovery from infection is believed to provide lifelong immunity against that serotype. However, cross-immunity to the other serotypes after recovery is only partial, and temporary. Subsequent infections (secondary infection) by other serotypes increase the risk of developing severe dengue [6]. DENV is frequently transported from one place to another by infected travellers; when susceptible vectors are present in these new areas, there is the potential for local transmission to be established. There are many clinical manifestations of dengue fever and other mosquito borne illnesses that are similar to each other, making it challenging to distinguish between them, especially after the onset of the illness [7].
A numerous of markers are thought to have the potential to predict severe dengue fever. With a high White Blood Cell count (WBC) and a low platelet count, dengue fever becomes more severe [8,9]. In a few studies, Aspartate Transaminase (AST) and Platelets count Ratio Index (APRI) have been identified as a markers that can be used to predict the severity of dengue infection. However, there is a dearth of evidence to support the usefulness of the AST/platelets count ratio index in clinical decision making. The results of this study could help predict the severity of dengue in tropical and subtropical nations where the disease is more prevalent. Therefore, the purpose of this study is to determine whether the AST/ platelet count ratio index is a reliable indicator of dengue virus infection in patients over the course of illness.
Materials and Methods
A prospective study done among 115 patients aged above 12 years with confirmed dengue fever who were admitted in tertiary care hospital, Guntur from June 2021 to December 2021. Patients with chronic illness, concomitant infections like hepatitis B/C and coinfection with malaria/ leptospirosis were excluded from study. All patients were clinically assessed and investigated for serum transaminases and platelet count on day 1, day 4 and day 7/on the day of discharge/death. During admission, blood samples were collected and haemoglobin, haematocrit, white blood cell count, Red Blood Cell (RBC), Mean Cell Volume (MCV), platelet count, Alanine Transaminase (ALT), AST, bilirubin and creatinine were measured on different days. We limited the time intervals for analysis to within 7 days after the date of a positive test. This period refers to days of illness or the course of illness.
The viral infection was detected using Immunoglobulin M (IgM) and NS1 antigen antibody Enzyme Linked Immunosorbent Assay (ELISA) tests InBios, India as they were performed routinely during the first week of illness onset. The data was tabulated and analysis was carried out using Microsoft Excel and SPSS version 21. Demographic and clinical data were summarized using mean and standard deviation and percentages. ANOVA test was applied to find association between dengue severities with laboratory parameters. The ability of the AST/Platelet Ratio Index (APRI) to predict the severity of dengue virus infection was assessed using the AUROC (areas under the receiver operating characteristic) curve.
Results
A total of 115 patients, two third of them were (76, 66.1%) males and the median age of the patients was 27 year (range from 15-45). Most of the patients (100, 87%) belongs to age group 20-39 years and around one third of them (36, 31.3%) were having past history of dengue infection as shown in Table 1.
| Characteristics | N | Percentage | |
|---|---|---|---|
| Age category | 12-19 years | 13 | 11.3 |
| 20-29 years | 57 | 49.6 | |
| 30-39 years | 43 | 37.4 | |
| >40 years | 2 | 1.7 | |
| Gender | Female | 39 | 33.9 |
| Male | 76 | 66.1 | |
| Dengue infection | Primary | 79 | 68.7 |
| Secondary | 36 | 31.3 | |
Table 1: General characteristics.
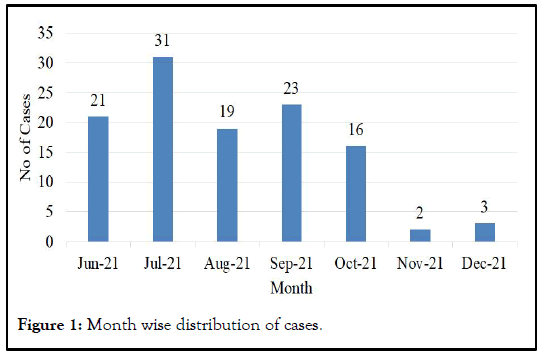
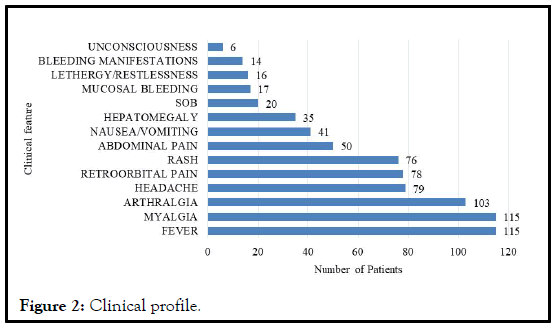
More than half (65, 56.5%) of the patients were presented as dengue without warning signs at the time of admission. However, along with duration, some of them progressed to dengue with warning signs and severe dengue before getting discharged as illustrated in Table 2. Most of the cases presented in the monsoon period (June to October) and most common symptoms were fever, myalgia followed by arthralgia, headache, retro orbital pain and rash etc., as depicted in Figures 1 and 2 respectively.
| Dengue classification (WHO 2009) | At the time of admission (n, %) | Before discharge (n, %) |
|---|---|---|
| Dengue without warning signs | 65 (56.5) | 55 (47.8) |
| Dengue with warning signs | 30 (26.1) | 37 (32.2) |
| Severe dengue | 20 (17.4) | 23 (20.0) |
Table 2: Disease profile.
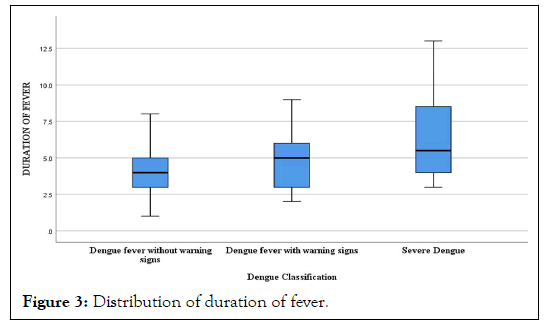
Duration of fever ranges from 1 to 13 days, overall mean duration was 4.53 ± 2.09 days and the mean duration was increased with the severity of disease as shown in Table 3 and Figure 3. The mean values of various lab parameters were shown in Table 4 and also we found determine positive association between various lab parameters with the dengue severity; total leucocyte (WBC) count (p=0.03), Mean Corpuscular Volume (MCV) (p=0.037), platelet count (p<0.001), Aspartate Transaminase (AST)(p<0.001), serum bilirubin (p=0.021) and serum creatinine (p=0.040) and were found statistically significant.
| Diagnosis | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Dengue fever without warning sings | 3.97 | 1.468 | 1 | 8 |
| Dengue fever with warning signs | 4.57 | 1.924 | 2 | 9 |
| Severe dengue | 6.3 | 3.011 | 3 | 13 |
| Total | 4.53 | 2.096 | 1 | 13 |
Table 3: Distribution of duration of fever.
| Lab parameters | Dengue without warning signs | Dengue with warning signs | Severe dengue | F-test | P-value |
|---|---|---|---|---|---|
| Hb (%) | 12.518 ± 1.45 | 12.480 ± 1.27 | 12.555 ± 1.15 | 0.019 | 0.981 |
| RBC | 3.968 ± 0.47 | 3.987 ± 0.59 | 4.015 ± 0.49 | 0.069 | 0.934 |
| WBC | 5417.38 ± 2535.82 | 4641.33 ± 2665.42 | 3807.50 ± 1568.09 | 3.636 | 0.030* |
| MCV | 71.22 ± 15.88 | 80.13 ± 15.04 | 73.80 ± 14.73 | 3.409 | 0.037* |
| PLT count | 139.26 ± 56.11 | 118.3 ± 36.98 | 82.00 ± 32.56 | 11.013 | <0.001* |
| AST | 78.23 ± 22.86 | 100.63 ± 22.65 | 125.40 ± 29.37 | 31.897 | <0.001* |
| ALT | 74.23 ± 16.37 | 71.67 ± 17.82 | 73.55 ± 16.08 | 0.242 | 0.785 |
| Sr. Bilirubin | 1.80 ± 0.86 | 2.09 ± 1.15 | 2.49 ± 0.96 | 4.015 | 0.021* |
| Creatinine | 1.21 ± 0.44 | 1.32 ± 0.49 | 1.54 ± 0.72 | 3.304 | 0.04 |
Table 4: Distribution of various lab parameters among patients at time of admission.
Aspartate transaminase and Platelet count Ratio Index (APRI) value ranges from 0.487 to 12.265 and we found that it is positively associated with severity of dengue and also found statistically significant (p<0.001) that means the risk of dengue virus infection increases with an AST/platelet count ratio index and then decreases with course of illness as shown in Table 5.
| Diagnosis | Mean | SD | F-test | P-value | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Dengue without warning signs | 2.005 | 1.4 | 22.266 | <0.001 | 0.487 | 7.763 |
| Dengue with warning sign | 2.402 | 1.11 | 0.899 | 5.833 | ||
| Severe dengue | 4.834 | 2.81 | 1.386 | 12.265 | ||
| Total | 2.601 | 1.95 | 0.487 | 12.265 |
Table 5: Distribution of APRI among patients and its association with severity of disease.
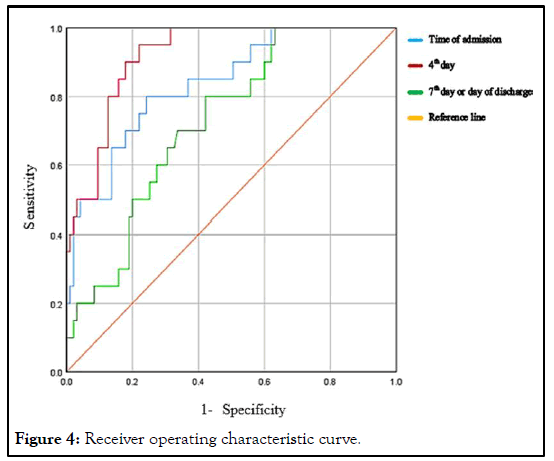
The AUC (areas under the receiver operating characteristic curve) for the APRI was 0.838 (95% CI: 0.744-0.932, P<0.001), 0.920 (95% CI: 0.869-0.971, P<0.001) and 0.726 (95% CI: 0.619-0.833, P=0.002) at the time of admission, 4th day and 7th day or day of discharge respectively as shown in Table 6 and we observed that APRI cut off value greater than or equal to 2.5 to predict dengue severity with sensitivity of 80% and specificity of 75.8% and after 4th day of admission the sensitivity of 90% and specificity of 77.9%. Also we observed with the decrease in APRI cut off value, there was increase in sensitivity as depicted in Figure 4.
| Parameters | Day of admission | 4th Day | 7th day/day of discharge |
|---|---|---|---|
| Area Under Curve (AUC) | 0.838 | 0.92 | 0.726 |
| Standard error | 0.048 | 0.026 | 0.055 |
| P-value | 0.000* | 0.000* | 0.002* |
| Lower bound (95% CI) | 0.744 | 0.869 | 0.619 |
| Upper bound (95% CI) | 0.932 | 0.971 | 0.833 |
| Sensitivity | 80 | 90 | - |
| Specificity | 75.8 | 77.9 | - |
| Cut off value | 2.5 | 2.5 | - |
Table 6: Receiver Operating Characteristic (ROC) curve of APRI.
Discussion
The incidence of dengue fever has significantly increased in recent years, might be attributed to the constant expansion of international travel and urbanization, making it an important health concern in India. Most manifestations of dengue are unspecific, which means that its correct diagnosis can be difficult, because of the similar presentation as other tropical diseases, especially for severe disease. There is no specific treatment for dengue fever. However, with good supportive care for severe cases, the mortality rate is less than 1%.
In the current study out of total 116 patients with dengue fever, 20-29 years age group was found mostly affected and males were more pretentious than females which was similar findings with the studies done in India. Most of the cases in this study were reported during peak of monsoon (July to September) similar to other studies also [10-13].
Our study revealed that most of the patient’s condition was not life threatening, as dengue fever with or without warning signs was found in 80%, severe dengue was observed in 20%. In some studies showing similar findings as our study and a few studies showing very less number of severe dengue cases as compared to our study no death was observed in our study, however some previous studies shown few deaths [14-17].
Most common symptoms in our study was fever (115, 100%) followed by myalgia, Headache which was similar in studies done in southern part of India shown that fever which was the most common presenting symptom followed by headache, myalgia and retro orbital pain etc. [18,19].
The relationship between various markers and dengue virus infection has been reported in the most of the literature, but with limited data on the role of the AST/platelet count ratio index. In a study done in malaria patients, APRI shown as potential marker of severity of disease [20]. And some previous studies also showed that AST/platelet count ratio index as a novel predictor of severe dengue infection. Our study also revealed that the AST/platelet count ratio index was an important indicator of severity of dengue virus infection.
Area under receiver operating characteristic curve in various studies were, 0.785 (95% CI: 0.724-0.893), 0.69 (95% CI: 0.27-1.00) and 0.703 (95% CI: 0.599-0.807) respectively. Whereas, in our study we found that the AUC (areas under the receiver operating characteristic curve) for the APRI was 0.838 (95% CI: 0.744-0.932, P<0.001), 0.920 (95% CI: 0.869-0.971, P<0.001) and 0.726 (95% CI: 0.619-0.833, P=0.002) at the time of admission, 4th day and 7th day or day of discharge respectively.
Our study revealed that, with the cut off value of APRI greater than or equal to 2.51, to predict dengue severity with sensitivity of 80% and specificity of 75.8% and after 4th day of admission the sensitivity of 90% and specificity of 77.9% and associated with increased risk of severe dengue which was almost similar to a study showed that sensitivity of 75% and a specificity of 76% for AST/platelet count ratio index as a marker of dengue infection. Our study also shown the impact of treatment on the AST/ platelet count ratio index. These biomarkers can be used to identify individuals at risk of developing dengue fever at an earlier stage, increase the likelihood of proper management, and prevent severe infection.
Conclusion
Our study concluded that laboratory markers, particularly aspartate Aminotransferase/Platelet count Ratio Index (APRI), can be useful for clinicians in primary care settings to predict the severity of dengue fever infection during the onset of symptoms, early referral to higher centers and the course of treatment for better outcome.
References
- Wilder-Smith A, Chawla T, Ooi EE, et al. Dengue: An expanding neglected tropical disease. Neglect Trop Dis East Asia. 2019;65-8.
- World Health Organization. Dengue and Severe Dengue Key Facts. World Health Organization. 2021;1-13.
- Ganeshkumar P, Murhekar MV, Poornima V, et al. Dengue infection in India: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(7):2-3.
[Crossref] [Google Scholar] [PubMed].
- World Health Organization. Dengue haemorrhagic fever: Diagnosis, treatment, prevention and control. World Health Organization. 1997.
- Aguas R, Dorigatti I, Coudeville L, et al. Cross serotype interactions and disease outcome prediction of dengue infections in Vietnam. Sci Reports. 2019;9(1):1-12.
[Crossref] [Google Scholar] [PubMed].
- Vu DM, LaBeaud AD. Chikungunya, dengue, zika, and other emerging mosquito-borne viruses. Neglect Trop Dis East Asia. 2021; 157-96.
- Kuo HJ, Lee IK, Liu JW, et al. Analyses of clinical and laboratory characteristics of dengue adults at their hospital presentations based on the World Health Organization clinical phase framework: Emphasizing risk of severe dengue in the elderly. J Microbiol Immunol Infect. 2018;51(6):740-8.
[Crossref] [Google Scholar] [PubMed].
- Murhekar M, Joshua V, Kanagasabai K, et al. Epidemiology of dengue fever in India, based on laboratory surveillance data, 2014-2017. Int J Infect Dis. 2019;84:10-4.
[Crossref] [Google Scholar] [PubMed].
- Ahmed AE, Dahman B, Altamimi A, et al. The aspartate aminotransferase/platelet count ratio index as a marker of dengue virus infection: Course of illness. J Infect Public Health. 2020;13(7):980-4.
[Crossref] [Google Scholar] [PubMed].
- Wiwanitkit V. The aspartate Aminotransferase/Platelet count Ratio Index (APRI) in dengue. J Med Virol. 2019;91(5):723.
- Zhang H, Xie Z, Xie X, et al. A novel predictor of severe dengue: The aspartate Aminotransferase/Platelet count Ratio Index (APRI). J Med Virol. 2018;90(5):803-9.
[Crossref] [GoogleScholar] [PubMed].
- Khan M, Venkateshwarlu C, Sandeep N, et al. A study of clinical and laboratory profile of dengue fever in a tertiary care hospital, Nizamabad, Telangana State, India. Int J Contemp Med Res. 2016;115(8):76-7.
- Kumari PL. Clinical Profile and outcome of dengue fever in tertiary care hospital at Kerala. Acad J Med. 2020;3(2):1-5.
- George T, Mankara Valsan S. Clinical and epidemiological profile of patients admitted with dengue fever in a tertiary care hospital, Thrissur, Kerala, India. Int J Community Med Public Heal. 2020;7(9):3654.
- Goudar SR, D HR, Mathew J, et al. Clinical profile and outcomes of dengue fever during monsoon season at a tertiary care hospital in South India. Int J Adv Med. 2021;8(11):1674.
- Badreddine S, Al-Dhaheri F, Al-Dabbagh A, et al. Dengue fever. Saudi Med J. 2017;38(10):1025-33.
[Crossref] [Google Scholar] [PubMed].
- Jampana KR, Paka AC. A study of clinical and laboratory profile of dengue fever in a tertiary care teaching hospital. Acad J Med. 2019; 2(2):18-20.
- Mohan K, Malaiyan J, Nasimuddin S, et al. Clinical profile and atypical manifestation of dengue fever cases between 2011 and 2018 in Chennai, India. J Fam Med Prim Care. 2020;9(2):1119.
[Crossref] [Google Scholar] [PubMed].
- Guedes KS, Sanchez BAM, Gomes LT, et al. Aspartate Aminotransferase to Platelet Ratio Index (APRI): A potential marker for diagnosis in patients at risk of severe malaria caused by Plasmodium vivax. PLoS One. 2019;14(11).
- Martins S, Pinheiro M, LD-JB, et al. Aspartate Aminotransferase to Platelet Ratio Index (APRI) for differentiation of primary and secondary infection by dengue virus. J Bras Patol Med Lab. 2018;54 (5):273-8.