The effect of impacted wisdom tooth surgery on the rate of mouth opening
2 Department of Engineering, Russian National Research Medical University, Moscow, Russia
Received: 30-Aug-2022, Manuscript No. PULBECR-22-5297; Editor assigned: 01-Sep-2022, Pre QC No. PULBECR-22-5297 (PQ); Reviewed: 15-Sep-2022 QC No. PULBECR-22-5297; Revised: 30-Dec-2022, Manuscript No. PULBECR-22-5297 (R); Published: 06-Jan-2023, DOI: 10.37532/PULBECR. 2023.5(1).1-4
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background and aim: Surgery of the third incisor molars leads to inflammatory reactions that cause pain, swelling and trismus. The aim of this study was to determine the effect of various factors before and during surgery such as age, sex and experience of the surgeon on the amount of trismus after latent third molar surgery. In this prospective study, 76 patients with different wisdom teeth occlusions in the maxilla or mandible participated. Preoperative and intraoperative factors were recorded in a checklist according to clinical examinations and radiography. The amount of trismus was assessed by maximal opening of the mouth in the area of central teeth before surgery and 48 hours after surgery. The obtained data were analyzed by SPSS software version 27 and paired t-test. The rate of mouth opening before surgery was at least 22 and at most 65 and the mean was 47.1 8 8.5 mm. 2 days after surgery, the maximum opening was at least 8 and at most 62 and the mean was 28.5 6 6.2 mm. none of the variables, except for root morphology, had a specific relationship with the rate of mouth opening. However, trismus was lower in patients who underwent surgery by specialists than in assistants. Most trismus was observed in cases performed by students. Trismus was more common in patients with joint disorders than in normal individuals. As a result, the rate of trismus was significantly higher in patients with third molars with distinct and subsequent roots.
Keywords
Truisms; Third molar; Affected tooth; Postoperative complications
Introduction
An impacted tooth is a tooth that cannot be placed in the dental arch at the expected time. The most common impacted teeth are the maxillary third and upper mandibular teeth. Generally, all impacted teeth should be extracted, unless their extraction is contraindicated [1]. Extraction of the third mandibular incisor naturally results in inflammatory reactions that cause pain, swelling, and truisms [2,3].
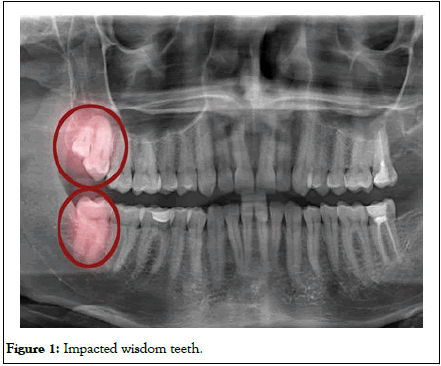
In clinical practice, it is better to predict when we will have a severe postoperative reaction than to consider appropriate preventive measures. Therefore, the dentist can reduce the occurrence of further misunderstandings between the dentist and the patient by informing the patient and predicting the possible complications of the surgery, and may use different drugs and methods to reduce these complications [4,5]. Surgery to remove affected third molar teeth, like any other surgery, has postoperative complications and symptoms that vary from mild to severe (Figure 1).
The occurrence of these complications is influenced by several factors and factors. Many studies have been done on postoperative complications and the factors affecting them. Although the association between preoperative and postoperative factors and postoperative complications has been established, clinical experience and reports indicate that these complications are widely varied and suggest that unknown factors are still present in postoperative reactions. Latent intellect has an effect [6]. The aim of this study was to determine the maximum rate of mouth opening after surgical removal of the third incisors. The next goal is to determine the relationship between different factors and the amount of truisms.
Materials and Methods
In this prospective study, the sample consisted of patients who underwent latent third molar surgery in the surgery department of the faculty of dentistry of Tabriz University of medical sciences. Based on the error of 0.05 according to Cohen's table, the minimum sample size was estimated to be five patients who participated in the present study. A checklist was prepared to record pre and intraoperative factors for each patient according to clinical examinations and radiography [7]. Preoperative factors were age, sex, presence of systemic diseases, drug use, temporomandibular joint disorders (pain, click, etc.), location of impacted teeth, type of occlusion (vertical, mesioangular, distangolar, horizontal, etc.). Injury in adjacent teeth (crown decay, root resorption and envelope formation), root morphology (root attachment or separation), root curvature mild (close to straight), moderate (we are between mild and severe) and severe (close to upright) and the maximum amount of mouth opening before surgery.
Intraoperative factors include: Experience and skill of the surgeon (specialist, specialist assistant and general student), number of carpools used and type of flap used (envelope, triangular), operations during surgery.
• Soft tissue incision (mucopriosteal flap alone).
• Bone removal.
• Bone extraction and tooth section), ankylosis of the impacted tooth
and duration of operation.
The maximum distance between incisors was measured by abslanger immediately before local anesthesia. For this purpose, patients were asked to open their mouths as much as possible, and the distance between the incisal edge of the upper and lower incisors (always by one person) was measured. For anesthesia in the upper jaw, posterior upper alveolar nerve block and palatal infiltration were used, and in the lower jaw, lower and buccal alveolar nerve blocks were used. For this purpose, 1.9 mm carpools containing 2% lidocaine and 1.80000 epinephrine were used.
The flaps used were envelopes or triangles, which in the envelope type were cut from the anterior edge of the ramus to the mesial of the tooth and in the triangular type; the incision was made from the anterior edge of the ramus to the mesial of the tooth. In addition, 0-3 thread was used for suturing [8]. In all cases, the duration of the operation from the time of incision to the last suture was recorded. After surgery, patients were prescribed antibiotics (amoxicillin), analgesics (NSAIDs and acetaminophen codeine), and chlorhexidine mouthwash. Oral and written home care recommendations were given to each patient. Each patient has an ice pack before discharge received and it was recommended to keep it in place for 15 minutes and remove it for 15 minutes and repeat this operation for 2 hours. The maximum distance between incisors was recorded 2 hours after surgery [9].
The data obtained from the study were analyzed by descriptive statistics, paired t-test and chi-square test or fisher's exact test using SPSS version 27 statistical software. In this study, P value less than 0.05 was considered statistically significant.
Results
In the present study, 52 females (68.42%) and 24 males (31.57%) with a mean age of 25. 11 years (16 to 58 years) participated. None of the patients studied had systemic diseases and did not take medication. The maximum amount of open mouth in the anterior teeth before surgery was at least 22, maximum 65 and on average 47.1 8 8.5 mm. 13 patients (17.1%) had discomfort in TMJ area (pain, click, etc.). 64 cases (84.2%) of the third molars were located in the mandible and 12 cases (15.8%) were located in the maxilla [10].
The position and curvature of the root of the third molars embedded in the upper and lower jaws are shown in Tables 1. In 52 cases (68.4%), the third molar did not damage the second molar. In 2 cases (14.5%) of the patient, caries of the second molar was observed. In five cases (10.5%) of the second molars had root resorption and in 4 cases (6.6%) periodontal pockets were formed. 28 patients (36.8%) were operated by a specialist surgeon and 24 cases (31.6%) were operated by specialist assistants and 2 cases (31.6%) were operated by general students.
| Type of occlusion in the maxilla | Number | Percent |
|---|---|---|
| Vertical | 4 | 5.3 |
| Disto-angular | 8 | 10.5 |
| Horizontal | 1 | 1.3 |
| Total | 13 | 17.1 |
Table 1: Position of the third molars located in the maxilla.
The average number of anesthetic cartridges used was 2.64 8 1.8 (from a minimum of 1 to a maximum of 6). In 50 patients, envelope flap (65.78%) and in 26 patients, triangular flaps (34.21%) were used to remove the impacted third molar.
The operations during surgery to remove the latent molar are listed in Table 2. In none of the patients, the third molar is latent. Ankylosis was not observed. The mean duration of the operation was 31.8 minutes (from 5 to 110 minutes). 2 out of 4 patients completed the study and 3 patients were excluded from the study. Maximum mouth opening 3 days after surgery (in 5 patients who completed the study) was at least 8, maximum 62 and mean 28.5 6 6.2 mm.
| Type of occlusion in the mandible | Number | Percent |
|---|---|---|
| Vertical | 21 | 27.6 |
| Disto-angular | 1 | 1.3 |
| Mesio-Angular | 31 | 40.8 |
| Horizontal | 14 | 18.4 |
| Total | 67 | 88.2 |
Table 2: Position of the third molars in the mandible.
The rate of mouth opening before surgery was significantly different from the rate of mouth opening 2 days after surgery (P=0.015). Overall, the analyzes showed that none of the factors except root morphology had a statistically significant relationship with the rate of mouth opening on the second day after surgery. The rate of mouth opening, two days after surgery, was significantly lower in patients with broad and distinct roots than in patients with conical and interconnected roots (P=0.03) (Tables 3 and 4).
| Root curvature | Number | Percent |
|---|---|---|
| Slight | 56 | 73.7 |
| Medium | 14 | 18.4 |
| Intense | 6 | 7.9 |
| Total | 76 | 100 |
Table 3: the amount of root curvature of the third molars lies.
| Surgical operations | Number | Percent |
|---|---|---|
| Soft tissue incision alone | 23 | 30.3 |
| Bone removal | 40 | 52.6 |
| Bone extraction with tooth section | 13 | 17.1 |
| Total | 76 | 100 |
Table 4: Operations during surgery.
Discussion
Removing the latent third molar always causes some pain, swelling, and trismus. Trismus is caused by inflammation of the masticatory muscles after tooth extraction. Because trismus usually reaches its maximum on the second day after surgery [11]. Postoperative status was recorded 3 days after surgery. The results of the present study did not show a statistically significant relationship between trismus level and age of patients. However, the patients participating in this study were mostly young and most (45 people) were about 17 to 23 years old. Also did not find a clear relationship between age and postoperative complications. Naserzadeh and colleagues observed more complications in older patients [12].
In this study, trismus was lower in males than females, but was not statistically significant. The above results were also applied to the plain by leaves and [13]. In contrast, reported gender as a predictor of postoperative discomfort [14,15]. It has been stated that the threshold of low pain in women and the use of more anesthetized carpool can increase the amount of trismus in them [16].
Patients who had discomfort (pain, clicks, etc.) in TMJ showed more trismus than others did. This may be due to the fact that surgical trauma causes more complications in patients suffering from TMJ discomfort.
The amount of trismus after mandibular third maxillary molar surgery was lower than that of the mandible. Induction of mandibular anesthesia through the lower alveolar nerve block due to proximity to anatomical areas, and trauma has more complications. In addition, the high bone density in the mandible causes more bone to be removed when the impacted tooth is extracted. As a result of increased trauma and surgical manipulation at the operation site, complications increase. On the other hand, removal of the third molars embedded in the maxilla requires less opening of the mouth and the patient's mouth is semi-open, which ultimately causes fewer traumas to the jaw muscles and TMJ. Nabahat also showed that postoperative complications were higher for the mandible (4.3%) than for the maxilla (1.2%) [17]. The results of this study showed less trismus in maxillary distangolar occlusion than the vertical type. It seems that it is easier to remove the impacted maxillary third molars in the distangolar position than in the vertical position. Also in the mandible, the amount of trismus was the lowest in patients with vertical occlusion and the highest in the horizontal type. Trismus was mediated in the micro vascular position. However, the amount of trismus was not significantly related to the type of latency. The same results are consistent with the results of leaf study [18].
In cases distal to the adjacent tooth (second molar) of the periodontal pocket, the rate of trismus was lower than in patients with seven healthy teeth without any damage. This may be due to the lower bone density in patients with periodontal pockets, which results in less bone extraction and reduced side effects [19].
Patients who had surgery by specialists had less trismus than patients in specialist residents and general students did. In addition, patients in the specialized residents group showed less trismus than patients in the third group. However, these results from statistical opinion were not significant. In other studies, there was no significant difference in the incidence of complications, including trismus among specialists and surgical assistants, surgical residents with general dentistry students, and oral surgeons with dentists. However, Nabahat reported a higher rate of trismus in the resident treated group compared to specialists, indicating that at least a number of complications could be related to the surgeon's experience.
The results showed that there was no clear relationship between the number of carpools consumed and postoperative trismus.
The amount of trismus in cases where the triangular flap was used was less than that of the enoloped flap, but this difference was not clear. In Kirk's study, there was no statistical difference between enoloped and triangular flaps in terms of pain or trismus on the second day after surgery.
The amount of trismus was the lowest in cases where only the mucopriosteal flap was used and the highest when the bone was removed with a tooth section. Studies have shown that in patients who underwent simple extraction (with forceps alone and without lifting the mucopriosteal flap), the amount of trismus was lower than in the surgical extraction group (mucopriosteal flap with or without cystectomy) [20]. The severity of trismus after surgical extraction did not depend on the severity of the surgery (cystectomy with or without coronary resection) [21,22].
In another trismus study, there was no clear association with the deeper occlusion of the third molar [23]. However, in one study, the location of the third molar and mastectomy were positively correlated with the amount of trismus and postoperative discomfort. Other papers show that when the third molar is located deep in relation to the occlusal surface or has distant, spherically rooted roots, trismus due to its extraction due to further bone extraction and even the section of the crown or roots increases [24]. In the present study, trismus increased with increasing root curvature (mild to severe), but this relationship was not statistically significant. The amount of trismus in patients with conical and interconnected roots was less than patients whose third molar roots were wide and distinct and this difference was statistically significant (P<0.05).
In this study, no significant relationship was observed between trismus after surgery and the duration of surgery. Grossi and Kim, Pedersen also found no significant relationship between trismus and duration of surgery. However, in one study, the severity of trismus was significantly related to the duration of surgery. The results of our research may be because the duration of the operation does not indicate the difficulty of surgery. Rather, it is more influenced by the surgeon's skill, and although surgeries performed by general education students have been easier than others have, they have taken more time and it is likely that surgical manipulation of the surgical site is less common among specialists and assistants. The results of previous studies suggest that unknown internal factors may influence the postoperative reaction of the third molar. For example, a patient's physical composition, weight, and preoperative anxiety may be more important determinants of radiographic variables. More attention is needed in this area and more studies are needed.
Conclusion
None of the factors, except for root morphology, had a statistically significant relationship with the rate of mouth opening on the second day after impacted wisdom tooth surgery. The rate of postoperative trismus was significantly higher in patients with third molars with separate and subsequent roots compared to conical and interconnected roots.
References
- Ghaeminia H, Nienhuijs ME, Toedtling V, et al. Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth. Cochrane Database Syst Rev. 2020;5(5):1-27. [Crossref] [Google Scholar] [PubMed]
- Eroglu CN, Durmus E, Kiresi D, et al. Effect of low-dose dexketoprofen trometamol and paracetamol on postoperative complications after impacted third molar surgery on healthy volunteers: A pilot study. Oral Surg Oral Med. 2014;19(6):622. [Crossref] [Google Scholar] [PubMed]
- Dodson TB, Susarla SM. Impacted wisdom teeth. BMJ Clinical Evidence. 2014.
- Farhadi F, Eslami H, Majidi A, et al. Evaluation of adjunctive effect of low-level laser Therapy on pain, swelling and trismus after surgical removal of impacted lower third molar: A double blind randomized clinical trial. Laser ther. 2017;26(3):181-7. [Crossref] [Google Scholar] [PubMed]
- Jaron A, Preuss O, Grzywacz E, et al. The impact of using kinesio tape on non-infectious complications after impacted mandibular third molar surgery. Int J Environ Res. 2021;18 (2):399. [Crossref] [Google Scholar] [PubMed]
- Mohammed IA, Deleme ZH. Kinesiology Tape in Comparison with Submucosal Injection of Dexamethasone in Reducing Pain and Swelling After Surgical Removal of Impacted Lower Wisdom Teeth. Dental J. 2020;20(1):18-24. [Crossref] [Google Scholar]
- Qassab AHM, Kumar N. Effects of hyaluronic acid gel application in reduction of post-surgical complications after lower wisdom teeth removalâ??a prospective study. Plant Arch. 2020;20(1):2796-800.
- Liu S, You Z, Ma C, et al. Effectiveness of drainage in mandibular third molar surgery: A systematic review and meta-analysis. J Oral Maxillofac Surg. 2018;76(8):1640-50. [Crossref] [Google Scholar] [PubMed]
- Zhu J, Yuan X, Yan L, et al. Comparison of postoperative outcomes between envelope and triangular flaps after mandibular third molar surgery: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2020;78(4):515-27. [Crossref] [Google Scholar] [PubMed]
- Badiee M, Jafari N, Fatemi S, et al. Comparison of the effects of toothpastes containing nanohydroxyapatite and fluoride on white spot lesions in orthodontic patients: A randomized clinical trial. J Dent Res. 2020;17(5):354. [Crossref] [Google Scholar] [PubMed]
- Yousef N, Niloufar M, Elena P, et al. Antipathogenic effects of emulsion and nanoemulsion of cinnamon essential oil against Rhizopus rot and grey mold on strawberry fruits. Foods Raw Mater. 2019;7(1):210-6. [Google Scholar]
- Duarte-Rodrigues L, Miranda EFP, Souza TO, et al. Third molar removal and its impact on quality of life: systematic review and meta-analysis. Qual Life Res. 2018;27(10):2477-89. [Crossref] [Google Scholar] [PubMed]
- Cervino G, Cicciu M, Biondi A, et al. Antibiotic prophylaxis on third molar extraction: Systematic review of recent data. Antibiotics. 2019;8(2):53. [Crossref] [Google Scholar] [PubMed]
- Hounsome J, Pilkington G, Mahon J, et al. Prophylactic removal of impacted mandibular third molars: a systematic review and economic evaluation. "Health Technol Assess Rep. 2020;24(30):1.
- Leung YY. Management and prevention of third molar surgery-related trigeminal nerve injury: time for a rethink. J Korean Assoc Oral Maxillofac Surg. 2019;45(5):233-40. [Crossref] [Google Scholar] [PubMed]
- De Poortere A, Van Der Cruyssen F, et al. The benefit of surgical management in post-traumatic trigeminal neuropathy: a retrospective analysis. Int J Oral Maxillofac Surg. 2021;50(1):132-8. [Crossref] [Google Scholar] [PubMed]
- Naserzadeh Y, Mahmoudi N, Nafchi AM, et al. Antipathogenic effects of plant essential oil nanoemulsions. Bio-Based Nanoemulsions for Agri-Food Applications: Elsevier. 2022;245-57.
- Naserzadeh Y, Mahmoudi N, et al. Chelating effect of black tea extract compared to citric acid in the process of the oxidation of sunflower, canola, olive, and tallow oils. Int J Agric Eng. 2018;12(5):5.
- Bouloux GF, Steed MB, Perciaccante VJ, et al. Complications of third molar surgery. Oral Maxillofac Surg Clin. 2007;19(1):117-28. [Crossref] [Google Scholar]
- Chiapasco M, De Cicco L, Marrone G, et al. Side effects and complications associated with third molar surgery. "Oral Surg Oral Med. 1993;76(4):412-20. [Crossref] [Google Scholar] [PubMed]
- Faress F, Yari A, Rajabi Kouchi F, et al. Developing an accurate empirical correlation for predicting anti-cancer drugsâ?? dissolution in supercritical carbon dioxide. Sci Rep. 2022;12(1):1-17. [Crossref] [Google Scholar] [PubMed]
- Park S-Y, Kim S-H, Kang S-H, et al. Improved oral hygiene care attenuates the cardiovascular risk of oral health disease: a population-based study from Korea. Eur Heart J Title. 2019;40(14):1138-45. [Crossref] [Google Scholar] [PubMed]
- Nabahatm H, Tahan M, Davoudabadi FA, et al. Regeneration of Permanent Tooth Enamel (Alternative Solution of Nano-hydroxyapatite) after Exposure to Beer (Laboratory Study at the Dental Center, Moscow, Russia). Adv Dent Oral Health. 2021;14(4): 555891.
- Apatzidou DA. The role of cigarette smoking in periodontal disease and treatment outcomes of dental implant therapy. Periodontology. 2022;90(1):45-61. [Crossref] [Google Scholar] [PubMed]