The Effect of Intra-Aortic Balloon Pump Counterpulsation in Patients with Cardiogenic Shock Due to Myocardial Infarction - A Research Study
Received: 14-Feb-2020 Accepted Date: May 20, 2020; Published: 27-May-2020
Citation: Nguyen MD, Hoa LTV, Anh TD, et al. The Effect of Ntra-Aortic Balloon Pump Counterpulsation in Patients with Cardiogenic Shock Due to Myocardial Infarction - A Research Study. Clinical Cardiology Journal 2020;4(1):4-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Albeit there have been many studies on IABP, there is no description about the time since the patient was shocked until the ball was placed and applied other treatments, and hence, there are not enough grounds to conclude the effectiveness of the IABP concerning the outcome or the degree of hemodynamic improvement immediately after placing the balloon - This is a bridge to apply coronary revascularization measures. This study aims to assess the effectiveness and safety of intra-aortic balloon pump counter-pulsation (IABP) in hemodynamic support to patients with CS due to myocardial infarction. Efficacy of intra-aortic balloon pump counter-pulsation (IABP) in hemodynamic support to patients with cardiogenic shock after myocardial infarction was a rapid recovery of hemodynamics after placing the shadow. The average time of shock escape is 24.1hours.The time from shock to the placing of the ball was 12.62 hours; the survival group placed the ball earlier than the mortality group (696 compared to 20.37 hours). The number of saved balls was 58.33 hours, the shortest is 4 hours, the longest is 240 hours (10 days).ICU day: 5.81 days, mechanical ventilation: 121.1 hours. Survival rate was 57.8%, the mortality rate was 42.2%.The study did not encounter technical problems: helium gas leakage, stabbing catheter fracture and the rate of infection was 8.8%, of which the infection at the ball placement was 6.6% and the systemic infection was 2.2%. Complications of thrombocytopenia: 8.8%, local bleeding 4.4%, limb ischemia of 4.4%.
Keywords
Efficacy; IABP; Myocardial infarction; Cardiogenic shock (CS)
Introduction
Cardiogenic shock (CS) is a condition of reduced tissue perfusion, due to impairment of the pumping function of ventricles under normal circulation volume. In patients with myocardial infarction, cardiogenic shock was the highest mortality rate [1-3], the previous mortality rate was70% [4], thanks to improvements in emergency and treatment, mortality rates were reduced to 40-50% [5-7]. Active treatment to restore, maintain hemodynamic stability, ensure optimal blood oxidation and coronary revascularization was the main treatment for patients with cardiogenic shock after myocardial infarction.
The emergence of mechanical support facilities such as intra-aortic balloon pump counter-pulsation (IABP), left ventricular support, ECMO contribute to increasing the quality of cardiogenic shock treatment. IABP is a device that supports mechanical circulation, is placed through the femoral artery by Seldinger technique, the balloon is inflated in the diastole (increased coronary artery perfusion, cerebral vessels), is rapidly flushed in the systole (reduced heart activity, reduced the need for O2 cardiac muscles and increased cardiac output) [8]. Research on cardiogenic shock after MI is divided into 2 stages. Stage before reperfusion treatment. During this period, the main treatment method was to maintain hemodynamics with vasopressor drugs and to begin the study to apply IABP [9-11]. The stage of reperfusion treatments was performed.
During this period, treatments for reperfusion were established such as CABG, fibrinolytic and PTCA with advances in resuscitation such as ventilation, dialysis... focusing on assessing the effectiveness of reperfusion treatment, the use of IABP and several mechanical hemodynamic support devices [12-15]. Previous studies [13,16-18] outlined that IABP improves prognosis and survival rate in cardiogenic shock.
In Vietnam, IABP has been used in some hospitals, such as Ho Chi Minh City Heart hospital (2005), 108 Military Central Hospital (2009), Hanoi Heart hospital (2012) has brought good effects on patients with severe heart failure after open-heart surgery, CS.
Although there have been many studies on IABP, there has been a limitation that lack of data about the time since the patient was shocked until the ball was placed and applied other treatments, so there are not enough grounds to conclude the effectiveness of the IABP concerning the outcome or the degree of hemodynamic improvement immediately after placing the balloon - This is a bridge to apply coronary revascularization measures.
Therefore, the study evaluated the efficacy and safety of IABP in the treatment of cardiogenic shock after myocardial infarction is the necessary research direction. To assess the effectiveness and safety of intra-aortic balloon pump counter-pulsation (IABP) in hemodynamic support to patients with CS due to myocardial infarction, we conducted the study with two objectives: 1, Efficacy of IABP in hemodynamic support to patients with CS after MI; 2, Remarks on the efficacy of treatment and complication of IABP in the treatment of CS after MI.
Research Methodology
Study population
A total of 45 patients were adminstr Place: 108 Military Central Hospital and Hanoi Heart Hospital from 2012 to 2017. Cardiogenic shock after myocardial infarction patients treated by IABP criteriaare described elsewhere [19,20]. Reduce tissue perfusion including at least one of the following: Urine<30 ml/hour, changes of consciousness, irritation or coma and/or spasm of peripheral vessels, cold limbs. Hemodynamic exploration parameters: cardiac index (CI) below 2.0 l/min/m2 of skin when no cardiac support is used or less than 2.2 l/min/m2 of skin when cardiac support is used. Patients withshock due to other causes such as hypovolemic shock, distribution disorder, congestion shock or even CS not because of myocardial infarction: aortic separation, acute cardiac arrest, acute myocarditis, progressive severe heart failure, or circulatory stop due to other causes were excluded.
This was a prospective, interventional study. All patients were examined thoroughly and collected general information. Especially, patients were assessed the severity of hospitalization and treatment, put central venous catheter, the arterial pressure measurement line, measurement of cardiac enzymes, arterial blood gas, ECG, cardiopulmonary X-ray, coronary angiography, and echocardiography: EF%, SV, SVR, CO, CI, mechanical complications.
For patientswith cardiogenic shock, we used Datascope CS 300 machine of the US and other types of balloon pump counter-pulsation. Before utilizing the balloon, we based on the height of patients to choose the volume of the ball. After placing IABP, all patients were followed up in the ICU according to the Vietnam national protocol for critical care patients. When hemodynamics improves well and is stable plus doses of dobutamine<8, epinephrine<0.4; norepinephrine<0.4, we reduced support rate from 1:1 to 1:2, 1:3 (4 hours), reduced ball volume, and finally removed the ball. Patients followed check-ups at the time of hospitalization (T0), after placing the ball for one hour (T1), after 3 hours (T3), after 6 hours (T6), after 24 hours (T24), after the fourth day of the year 4, 6, 7 (D4, D5, D6, D7) and when withdrawing the ball.
Results
There were 45 patients included in the study. The percentage of female was 40%. The average of age was 69.11years.There was 64.4% patients with angina pectoris, 48.8% with hypertension, 26.6% smokers; 35.5% patients with acute kidney disease; 22.2% diabetes; 6.6% COPD; Peripheral vascular disease (6,67%) (Table 1).
TABLE 1
Study population characteristics and CVD risk factors.
| Indices | Mean (SD) | n (%) |
|---|---|---|
| Age (years) | 69.11 (10.94) | |
| Gender | 18/27 (40/60) | |
| BMI (kg/m2) | 21.25 (2.44) | |
| Risk factors | ||
| Angina pectoris | 29 (64.4) | |
| Diabetes | 10 (22.2) | |
| Hypertension | 22 (48.8) | |
| COPD | 3 (6.6) | |
| Smoking | 12 (26.6) | |
| Lipoprotein abnormal | 9 (20.0) | |
| PVD | 3 (6.67) | |
| Stroke | 3 (6.67) | |
| Acute kidney diseases | 16 (35.5) |
There was 34 out of 45 has ST elevation (75.5%). The patient witharrhythmic complications (Atrial fibrillation 13,3%, Ventricular tachycardia 15,5%, Ventricular fibrillation 6,6%). There was 77% patients had shocked before registed to hospital.EF: 26.5 ± 13.5%;Killip class IV: 77.7%. CI: 2.0 ± 0.5 l/p/m2. Mean of APACHE II score was 20.50 ± 7.33 and SOFA score was 10.33 ± 4.53 (Table 2).
TABLE 2
Clinical pictures of patients at the time of administration.
| Indices | Mean (SD) | n (%) |
|---|---|---|
| Stenosis | ||
| Three coronary arteries | 30 (66.7) | |
| The carotid artery | 1 (1.2) | |
| Other arteries | 2 (4.4) | |
| AF | 6 (13.3) | |
| ST elevation | 34 (75.5) | |
| VT | 7 (6.6) | |
| VF | 3 (4.4) | |
| Severity | ||
| Killip III | 10 (22.3) | |
| Killip IV | 35 (77.7) | |
| Aforementioned Shock | 35 (77.7) | |
| EF% | 26.5 (13.5) | |
| Cardiac index (L/min/m2) | 2.0 (0.5) | |
| APACHE II | 20.50 (7.33) | |
| SOFA | 10.33 (4.53) |
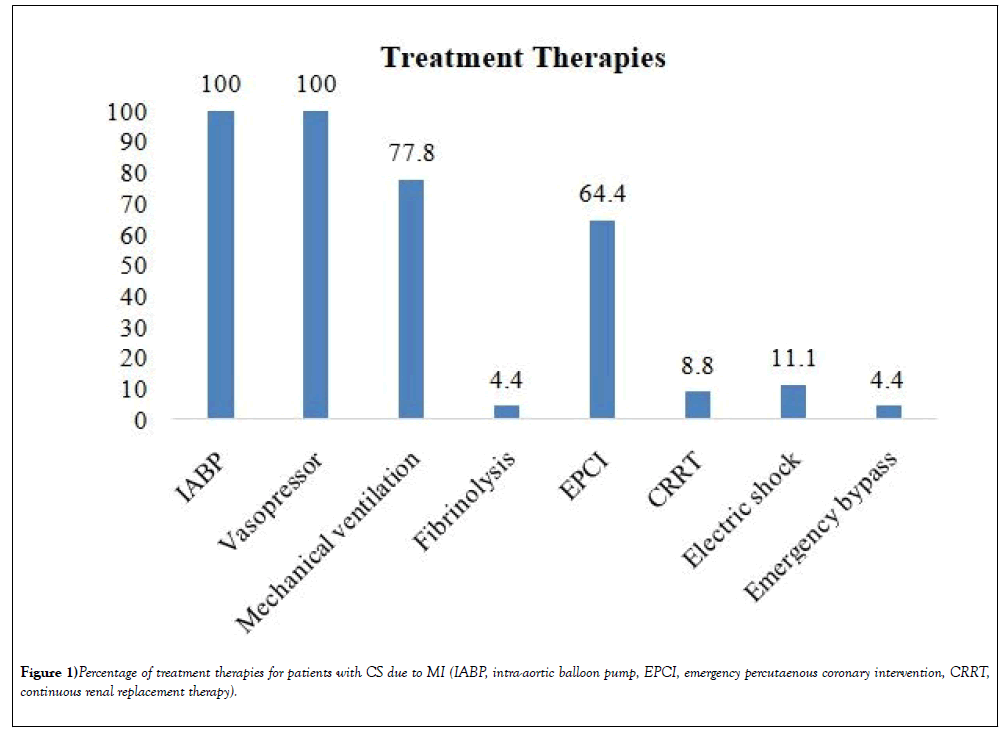
100% patients were treated with vasopressor and IABP. 64.4% with percutaneous coronary intervention, Mechanical ventilation: 77.8%, CRRT: 8.8%; Electric shock: 11.1%, Emergency surgery: 4.4% (Figure 1).
The time from cardiogenic shock to the time IABP was 12.62 ± 11.37 hours, before 12 hours: 60% (27/45). Group 1 was IABP earlier than group 2 (6,96 ± 7.4 hours vs. 20.37 ± 11.36 hours) (Table 3).
TABLE 3
The time from cardiogenic shock to the time IABP.
| Time | 01-Jun hours |
07-Dec hours |
13-24 hours |
After 24 hours | Mean (SD) (hours) | p-value |
|---|---|---|---|---|---|---|
| Group 1 (n=26) | 15 (88.2%) | 7 (70%) | 1 (10%) | 3 (37.5%) | 6,96 (7,45) | |
| Group 2 (n=19) | 2 (11.8%) | 3 (30%) | 9 (90%) | 5 (62.5%) |
20,37 (11,36) | <0.01 |
| Total (n=45) | 17 (100%) | 10 (100%) | 10 (100%) | 8 (100%) |
12,62 (11,37) |
Variability in hemodynamic parameters of cardiogenic shock after acute myocardial infarction patients treated by IABP
Heart rate decreased significantly after 72 hours, from 125.1 ± 15.2 to 97.1 ± 5.6 beats/min (p<0.05). Group 1: heart rate changes earlier than group 2, after 6 hours of IABP (124.1 ± 16.5 to 110.1 ± 7.0 beats/min) (Table 4).
TABLE 4
Heart rate after IABP.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 125.1 ± 15.2 | 124.1 ± 16.5 | 127.5 ± 15.4 | >0.05 |
| T1 | 121.2 ± 12.2 | 120.2 ± 11.2 | 125.1 ± 13.4 | >0.05 |
| T3 | 118.9 ± 10.5 | 116.5 ± 10.7 | 121.2 ± 11 | >0.05 |
| T6 | 115.8 ± 7.1 | 110.1 ± 7.0* | 118.7 ± 8.2 | <0.05 |
| T24 | 110.2 ± 6.1 | 108.4 ± 7.4* | 114.2 ± 76.8 | <0.05 |
| T48 | 106.7 ± 5.3 | 104.9 ± 6.2* | 109.5 ± 5.7 | <0.05 |
| T72 | 97.1 ± 5.6* | 95.1 ± 6.1* | 103.4 ± 6.3 | <0.05 |
| D4 | 95.1 ± 5.1* | 93.3 ± 4.2* | 96.1 ± 5.4* | >0.05 |
| D5 | 90.6 ± 4.8* | 90.1 ± 4.1* | 90.6 ± 4.1* | >0.05 |
| D6 | 87.1 ± 3.1* | 86.1 ± 3.4* | 87.1 ± 3.5* | >0.05 |
| D7 | 87.3 ± 3.4* | 88.1 ± 3.6* | 86.2 ± 3.5* | >0.05 |
MAPincreased rapidly after IABP and changed significantly from 24 hours: increasing from 56.1 ± 18.2 to 77.5 ± 12.6 mmHg (p<0.05) - MAP of the two groups has a difference in the sixth hour after IABP (Table 5).
TABLE 5
Mean arterial pressure (mmHg)after IABP.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 56.1 ± 18.2 | 58.1 ± 18.6 | 55.2 ± 19.5 | >0.05 |
| T1 | 60.9 ± 15.8 | 62.6 ± 15.0 | 58.8 ± 18.7 | >0.05 |
| T3 | 63.5 ± 15.5 | 61.5 ± 13.0 | 65.5 ± 17.6 | >0.05 |
| T6 | 67.5 ± 12.1 | 70.2 ± 12.1 | 65.4 ± 14.2 | <0.05 |
| T24 | 77.5 ± 12.6* | 80.1 ± 13.4* | 74.1 ± 13.2 | <0.05 |
| T48 | 80.6 ± 10.3* | 84.6 ± 13.1* | 75.6 ± 10.7* | <0.05 |
| T72 | 81.1 ± 12.5* | 82.7 ± 12.6* | 78.1 ± 12.8* | <0.05 |
| D4 | 81.9 ± 9.7* | 83.9 ± 10.2* | 80.1 ± 9.7* | >0.05 |
| D5 | 82.5 ± 10.2* | 84.1 ± 10.0* | 80.7 ± 10.2* | >0.05 |
| D6 | 82.4 ± 11.3* | 84.4 ± 11.1* | 80.4 ± 18.1* | >0.05 |
| D7 | 78.8 ± 15.4* | 85.8 ± 15.7* | 66.8 ± 15.2* | <0.05 |
EF improved after IABP and changed significantly from 72 hours (from 26.5 ± 13.5 to 34.6 ± 14.1%) (Table 6).
TABLE 6
EF% after IABP, CI improved after IABP 48 hours: 2.0 ± 0.5 to 3.9 ± 1,2l/min/m2.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 26.5 ± 13.5 | 27.5 ± 13.5 | 23.1 ± 13.2 | >0.05 |
| T1 | 26.5 ± 14.4 | 27.9 ± 15.6 | 23.0 ± 13.2 | >0.05 |
| T3 | 28.8 ± 12.1 | 29.9 ± 15.2 | 27.1 ± 12.4 | >0.05 |
| T6 | 28.4 ± 11.1 | 30.9 ± 16.5 | 27.3 ± 16.1 | <0.05 |
| T24 | 30.5 ± 11.4 | 32.1 ± 12.2* | 28.2 ± 12.6 | <0.05 |
| T48 | 31.4± 14.2 | 35.9 ± 11.4* | 27.5± 11.7 | <0.05 |
| T72 | 34.6 ± 14.1* | 36.4 ± 13.6* | 28.5 ± 13.1 | <0.05 |
| D4 | 36.1 ± 13.3 | 39.7± 10.1* | 28.7± 10.6* | <0.05 |
| D5 | 40.3 ± 11.1 | 44.2 ± 12.5* | 32.2 ± 12.9* | <0.05 |
| D6 | 42.5 ± 12.2 | 44.5 ± 13.1* | 35.5 ± 13.7* | <0.05 |
| D7 | 43.5 ± 14.5 | 46.5 ± 14.3* | 37.5 ± 14.9* | <0.05 |
Group 1, CI increased significantly after 24 hours: 4.0 ± 1.5 compared with 2.2 ± 0.5l /min/m2(p<0.05). Group 2, CI increased significantly after 48 hours: 3.9 ± 0.9 compared with 2.0 ± 0.3 l /min /m2 (p<0.05) (Table 7).
TABLE 7
CI (L/min/m2 ) after IABP.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 2.0 ± 0.5 | 2.2 ± 0.5 | 2.0 ± 0.3 | >0.05 |
| T1 | 2.7 ± 0.8 | 2.9 ± 0.8 | 2.6 ± 0.7 | >0.05 |
| T3 | 2.9 ± 0.1 | 2.9 ± 0.1 | 2.9 ± 0.2 | >0.05 |
| T6 | 2.6 ± 0.7 | 3.1 ± 0.4 | 2.5 ± 0.5 | <0.05 |
| T24 | 3.8 ± 1.5 | 4.0 ± 1.5* | 3.4 ± 1.4 | <0.05 |
| T48 | 3.9 ± 0.8* | 3.8 ± 0.7* | 3.9 ± 0.9* | >0.05 |
| T72 | 4.0 ± 1.2 | 4.1 ± 1.3* | 3.8 ± 1.3* | >0.05 |
| D4 | 3.8 ± 0.9 | 3.9 ± 0.8* | 3.7 ± 0.7* | >0.05 |
| D5 | 4.1 ± 1.1 | 4.3 ± 1.0* | 3.8 ± 1.3* | >0.05 |
| D6 | 4.0 ± 0.9 | 4.2 ± 0.8* | 3.8 ± 0.8* | >0.05 |
| D7 | 3.9 ± 0.9 | 4.1 ± 0.8* | 3.8 ± 0.6* | >0.05 |
SVR decreased after 72 hours: 986.7 ± 9.5 vs. 1316.3 ± 112.8. The difference between the two groups at the 24th hour after IABP (926.7 ± 90.1 vs. 1185.1 ± 101.5 p<0.05) (Table 8).
TABLE 8
SVR (dynes/sec/cm-5) after IABP.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 1316.3 ± 112.8 | 1308.6 ± 134.1 | 1335.3 ± 120.2 | >0.05 |
| T1 | 1204.4 ± 123.4 | 1190.9 ± 103.4 | 1292.7 ± 115.2 | >0.05 |
| T3 | 1183.7 ± 102.9 | 1156.5 ± 100.2 | 1209.4 ± 99.2 | >0.05 |
| T6 | 1057.2 ± 101.2 | 930.2 ± 104.2 | 1194.9 ± 90.1 | >0.05 |
| T24 | 1037.2 ± 98.2 | 926.7 ± 90.1* | 1185.1 ± 101.5 | <0.05 |
| T48 | 1052.7 ± 90.1 | 925.3 ± 121.2 | 1190.7 ± 105.6 | <0.05 |
| T72 | 986.7± 89.5* | 874.7 ± 88.2 | 1105.0 ± 99.0* | <0.05 |
| D4 | 975.2 ± 99.1 | 861.3 ± 101.6 | 1069.9 ± 89.3 | <0.05 |
| D5 | 919.1 ± 79.2 | 850.4 ± 100.2 | 1058.0 ± 97.4 | <0.05 |
| D6 | 838.4 ± 101.9 | 822.8 ± 90.6 | 901.9 ± 95.2 | <0.05 |
| D7 | 814.5 ± 99.0 | 807.6 ± 91.3 | 934.2 ± 93.1 | <0.05 |
Lactate decreased after 24 hours: 7.9 ± 4.2 mmol/l decreased to 3.1 ± 1.1 mmol/l. The difference between the two groups at 24 hours after IABP (2.2 ± 1.5 vs. 3.9 ± 1.4 mmol/l, p<0.05) (Table 9).
TABLE 9
Lactate (m mol/l) after IABP.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 7.9 ± 4.2 | 7.8 ± 4.6 | 7.9 ± 5.1 | >0.05 |
| T1 | 7.1 ± 5.7 | 6.9 ± 5.1 | 7.2 ± 5.2 | >0.05 |
| T3 | 6.0 ± 7.7 | 5.9 ± 7.3 | 6.0 ± 7.8 | >0.05 |
| T6 | 3.1 ± 1.2 | 2.8 ± 1.1* | 3.2 ± 1.6 | >0.05 |
| T24 | 3.1 ± 1.7 * | 2.2 ± 1.5* | 3.9 ± 1.4 | <0.05 |
| T48 | 1.9 ± 1.3* | 1.8 ± 1.3* | 2.1 ± 1.9* | >0.05 |
| T72 | 2.0 ± 0.4* | 2.1 ± 0.2* | 1.9 ± 0.4* | >0.05 |
| D4 | 2.2 ± 0.5* | 2.3 ± 0.4* | 2.1 ± 0.1* | >0.05 |
| D5 | 2.3 ± 0.9* | 2.0 ± 0.8* | 2.4 ± 0.3* | >0.05 |
| D6 | 2.1 ± 0.9* | 2.0 ± 0.5* | 2.3 ± 0.3* | >0.05 |
| D7 | 1.7 ± 0.2* | 1.5 ± 0.1* | 1.9 ± 4.1* | >0.05 |
The Noradrenalin dose decreases after IABP, significantly changed affter 48 hours: 0.026 ± 0.03 μg/kg/min (p<0.05). The dose of noradrenalin of group 1 decreased faster than group 2: 0.10 ± 0.21 vs. 0.19 ± 0.27 μg/kg /min after 24 hours of IABP, p<0.05 (Table 10).
TABLE 10
The dose of Noradrenalin between the two group (μg/kg/min) used in treatment.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 0.68 ± 0.89 | 0.7 ± 0.81 | 0.66 ± 0.71 | >0.05 |
| T1 | 0.55 ± 0.31 | 0.53 ± 0.33 | 0.60 ± 0.41 | >0.05 |
| T3 | 0.50 ± 0.26 | 0.48 ± 0.21 | 0.52 ± 0.36 | >0.05 |
| T6 | 0.16 ± 0.20 | 0.11 ± 0.22 | 0.19± 0.25 | >0.05 |
| T24 | 0.15± 0.22 | 0.10 ± 0.21* | 0.19 ± 0.27 | <0.05 |
| T48 | 0.02 ± 0.03* | 0.01 ± 0.04* | 0.03 ± 0.04* | <0.05 |
| T72 | 0.02 ± 0.03* | 0.01 ± 0.05* | 0.04 ± 0.07* | <0.05 |
| D4 | 0.03 ± 0.05* | 0.01 ± 0.06* | 0.05 ± 0.06* | <0.05 |
| D5 | 0.02 ± 0.03* | 0.01 ± 0.01* | 0.03 ± 0.04* | <0.05 |
| D6 | 0.01 ± 0.02* | 0.007 ± 0.01* | 0.02 ± 0.02* | <0.05 |
| D7 | 0.01 ± 0.02* | 0.008 ± 0.02* | 0.02 ± 0.01* | <0.05 |
The adrenaline dose decreased rapidly after IABP, after 24 hours from 0.91 ± 0.17 to 0.11 ± 0.38 μg/kg/min (p<0.05). The dose of adrenalin of group 1 decreased faster than group 2: 0.71 ± 0.53 vs. 0.94 ± 0.56 μg/ kg/min after 06 hours of IABP, p<0.05 (Table 11).
TABLE 11
The dose of adrenalin (μg/kg/min) used in treatment.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 0.91 ± 0.17 | 0.92 ± 0.11 | 0.9 ± 0.19 | >0.05 |
| T1 | 1.04 ± 0.57 | 0.83 ± 0.52 | 1.11 ± 0.58 | >0.05 |
| T3 | 0.83 ± 0.51 | 0.71 ± 0.53 | 0.94 ± 0.56 | >0.05 |
| T6 | 0.32 ± 0.41 | 0.14 ± 0.45* | 0.45 ± 0.44 | >0.05 |
| T24 | 0.11 ± 0.38* | 0.05 ± 0.31* | 0.22 ± 1.31* | <0.05 |
| T48 | 0.12 ± 0.33* | 0.01 ± 0.34* | 0.24 ± 1.31* | <0.05 |
| T72 | 0.06 ± 0.21* | 0.02 ± 0.21* | 0.10 ± 1.23* | <0.05 |
| D4 | 0.05 ± 0.12* | 0.01 ± 0.14* | 0.11 ± 1.14* | <0.05 |
| D5 | 0.04 ± 0.06* | 0.01 ± 0.03* | 0.08 ±1.09* | <0.05 |
| D6 | 0.015 ± 0.02* | 0.01 ± 0.08* | 0.02 ± 1.01* | <0.05 |
| D7 | 0.01 ± 0.13* | 0.01 ± 0.12* | 0.02 ± 1.12* | <0.05 |
The dose of Dobutamin decreased significantly after 48 hours of IABP: from 14.8 ± 5.5 to 8.6 ± 5.0 μg/kg/minute, p<0.05 (Table 12).
TABLE 12
The dose of dobutamin (μg/kg/min) used in treatment.
| Time | Total | Group 1 | Group 2 | P (1-2) |
|---|---|---|---|---|
| (n=45) | (n=26) | (n=19) | ||
| T0 | 14.8 ± 5.5 | 13.8 ± 7.3 | 15.1 ± 6.1 | >0.05 |
| T1 | 14.5 ± 8.7 | 14.1 ± 6.7 | 14.9 ± 5.1 | >0.05 |
| T3 | 11.7 ± 10.3 | 10.1 ± 4.2 | 12.5 ± 6.2 | >0.05 |
| T6 | 10.1 ± 6.3 | 8.6 ± 5.1 | 11.2 ± 9.1 | >0.05 |
| T24 | 9.6 ± 6.7 | 9.2 ± 7.3* | 10.1± 8.6 | >0.05 |
| T48 | 8.6 ± 5.0* | 8.2 ± 5.2* | 9.1 ± 4.3* | >0.05 |
| T72 | 6.3 ± 6.3* | 4.0 ± 5.1* | 8.2 ± 7.5* | <0.05 |
| D4 | 5.7 ± 4.3* | 3.5 ± 4.0* | 7.1 ± 8.3* | <0.05 |
| D5 | 4.6 ± 6.4* | 3.1 ± 6.6* | 6.0 ± 5.9* | <0.05 |
| D6 | 4.7 ± 4.1* | 2.8 ± 3.4* | 6.2 ± 10.9* | <0.05 |
| D7 | 4.6 ± 6.1* | 1.1 ± 3.5* | 7.1 ± 13.8* | <0.05 |
Efficacy and complication of IABPin treatment cardiogenic shock after myocardial infarction
Time of shock appearance was 8.5 hours. Time of sock escape: 24, 1 ± 6,2 giá». The time from the time of cardiac shock to the time IABP was 12.62 ± 11.37 hours. The number of hours saved was: 58.33 ± 40.14 hours (Table 13).
TABLE 13
Time to escape shock, ventilation, putting the ball and ICU treatment.
| Time | Mean ± SD (Min-Max) |
|---|---|
| Cardiogenic shock (hours) | 8.5 ± 55.37 (1-75) |
| Cardiogenic shock to IABP (hours) | 12.62 ± 11.37 (1-36) |
| IABP (hours) | 58.33 ± 40.14 (4 - 120) |
| Out of Shock (hours) | 24.1 ± 6.2 (1-32) |
| Mechanical ventilation (hours) | 121.1 ± 102.2 (19 - 301) |
| ICU treatment (days) | 5.81 ± 8.21 (1 - 21) |
Time to recover systolic blood pressure≥90 mmHg of groups: IABP + PCI, group without acute renal failure, group EF>40% and group of Killip I-II at ICU faster than groups other.The group with IABP before 12 hours recovered faster than the group with IABP after 12 hours (7.2 ± 4.1 hours compared to 16.3 ± 6.8 hours, p<0.001) (Table 14).
TABLE 14
Time to recover systolic blood pressure (SBP) in different subgroups.
| Variables | SBP³ 90 mmHg (hours) | p-value | |
|---|---|---|---|
| IABP | IABP + PCI (n = 29) | 6.9 ± 3.0 | <0.01 |
| IABP (n = 16) | 12.1 ± 5.3 | ||
| Befor 12 hours group (n=27) | 7.2 ± 4.1 | <0.001 | |
| After 12 hours group (n= 18) | 16.3 ± 6.8 | ||
| Acute renal failure | Yes | 6.4 ± 2.8 | <0.001 |
| No | 12.5 ± 4.9 | ||
| Killip ICU hospitalization | Class I-II | 7.9 ± 5.4 | <0.05 |
| Class III-IV | 10.9 ± 5.2 | ||
| Time of shock appearing | ≤ 48 hours | 9.7 ± 5.1 | >0.05 |
| >48 hours | 10.0 ± 5.6 | ||
| EF indicators | <40% | 10.6 ± 5.3 | <0.05 |
| ³ 4% | 8.6 ± 4.6 | ||
At the time of the ball draw, hemodynamic indicators improved clearly.Heart rate decreased to 89.2 ± 3.9 compared with 125.1 ± 15.2 beats/minute, BP increased to 81.6 ± 16.1 mmHg. EF% increased to 40.9 ± 10.8 vs.26.5 ± 13.5%. CI increased to 3.9 ± 0.9 vs. 2.0 ± 0.5 L/min/ m2 (Table 15).
TABLE 15
Hemodynamic indicators after treatment with IABP.
| Varaibles | T0 | T ball drawn | p-value |
|---|---|---|---|
| HR | 125.1 ± 15.2 | 89.2 ± 3.9 | <0.05 |
| MBP | 56.1 ± 18.2 | 81.6 ± 16.1 | <0.05 |
| (EF%) | 26.5 ± 13.5 | 40.9 ± 10.8 | <0.05 |
| CI (L/min/m2) | 2.0 ± 0.5 | 3.9 ± 0.9 | <0.05 |
| Urine (ml/ hours) | 15.1 ± 10.3 | 90.2 ± 25.2 | <0.05 |
| Lactate (mmol/l) | 7.9 ± 4.2 | 2.4 ± 0.8 | <0.05 |
Survival rate is 57.8%, overall mortality rate is 42.2%. The group that IABP and PCI was lower than the group with only 37.9% compared with 50%, p<0.01 (Table 16).
TABLE 16
The mortality rate in this study.
| Variables | Total | Reconstruction of coronary arteries | p-value | |
|---|---|---|---|---|
| Yes | No | |||
| In general | 42.2% (19/45) | 37.9% (11/29) | 50.0% (8/16) | <0.01 |
| In 30 days | 40% (18/45) | 38% (11/29) | 43.75% (7/16) | <0.05 |
Thrombocytopenia: 8,8%, Multi-organ failure: 4,4% và Anemia: 4,44%, Bleeding:4.4% (Table 17).
TABLE 17
Systemic and local complications.
| Variables | Total | Group 1 | Group 2 |
|---|---|---|---|
| (n=45) | (n=26) | (n=19) | |
| Thrombocytopenia | 4 (8.8%) | 2 (8.6%) | 2 (12.5%) |
| Anemia | 2 (4.4%) | 1 (4.3%) | 1 (6.25%) |
| Bleeding | 2 (4.4%) | 1 (4.3%) | 1 (6.25%) |
| Technical problems | 0 | ||
The percentage of infection was 8.8%, the infection at the placement was 6.6% and the whole body was 2.2% (Table 18).
TABLE 18
Infection complications.
| Area | Total | Group 1 | Group 2 |
|---|---|---|---|
| (n=45) | (n=26) | (n=19) | |
| In place | 3 ( 6.6%) | 1 (3.5%) | 2 (12.5%) |
| Body | 1 (2.2%) | 1 (6.3%) | |
| Total | 4 (8.8%) | 1 (3.5%) | 3 (18.8%) |
Discussion
We have conducted IABP for 45 patients with cardiogenic shock after myocardial infarction: 27 men and 18 women, the average age was 69.11 ± 10.94. Hypertension 48.8%, chest paint 64.4%, diabetes 22.2%, smoking 26.6%, 64.6% of patients with emergency coronary intervention and 4.4% of patients received fibrinolysis.
Patients hospitalized in severe condition, 77.7% of patients with cardiogenic shock, EF%: 26.5 ± 13.5; Killip class IV 77.7%, APACHE II score 20.50 ± 7.33 and SOFA score was 10.33 ± 4.53. Tran Duy Anh's study on 115 patients with IABP, showed: NYHA IV: 76 patients (66.08%), cardiogenic shock 24.34%), EF: 35.7 ± 5.2% Timing of cardiogenic shock after myocardial infarction was 8.5 (1-75) hours, this result is similar to some authors, recording cardiogenic shock usually occurs 5-10 hours after MI (14,16,21,22).
In the study, there were 29/45 patients accounted for 64.5% who received PCI in combination with IABP during treatment. This ratio varies depending on the views and capabilities of each medical center. There are 5-10% in patients with acute myocardial infarction with cardiogenic shock complications. However, it is difficult to accurately assess the frequency of cardiogenic shock due to myocardial infarction because many patients have died before coming to the hospital and have not been diagnosed[2,21].
Report SHOCK on 1160 patients with cardiogenic shock: 74.5%; 8.3% of 2-leaf openings; 4.6% perforation of the ventricular septum; 3.4% due to failure of the right ventricle; 1.7% suffered from cardiac/cardiac tamponade and 8% shock due to other causes[22]. Our study, 35.5% had arrhythmic complications and 2/45 patients (4.4%) had mechanical complications.
Efficacy of intra-aortic balloon pump counter-pulsation (IABP) in hemodynamic support to patients with cardiogenic shock after myocardial infarction
Time to place the ball, time to use the ball (save the ball): In the study, we recorded the difference in time to place IABP in different groups of patients: the result of Table 3 shows the time from the time of cardiac shock to when the ball is set to 12.62 ± 11.37 hours, patients were placed IABP before 12 hours: 60% (27/45 patients), in the survival group: patients placed the ball earlier than the mortality group (6.96 ± 7.4 hours vs. 20.37 ± 11.36 hours, p<0.05); mortality group - the number of patients who placed the ball after 12 hours was 73.6% compared to the survival group: 15.35%.
Change heart rate after placing the ball: After IABP,the heart rate gradually decreased and changed significantly from 72hours, from 125.1 ± 15.2 to 97.1 ± 5.6 beats/minute (p<0.01), survival group: heart rate changes earlier than the mortality group, significant after 6 hours of placing the ball (124.1 ± 16.5 to 110.1 ± 7.0 beats/minute), p<0.05. According to Patel et al. determining the hemodynamic factors affecting the consumption of myocardial oxygen and the efficacy of IABP in reducing cardiac loading in the confidant period suggested that IABP reduced heart rate, this change is statistically different from the 3rd and 4th days onwards[23].
Arterial blood pressure changes: Arterial blood pressure improves rapidly after placing the balloon and changes significantly after 24 hours: increasing from 56.1 ± 18.2 to 77.5 ± 12.6 mmHg (p<0.01), MAP of the two survival and mortality groups differed at the sixth hour after placing the ball (78.2 ± 12.1 compared to 70.4 ± 14.2 mmHg).
Changing of Cardiac output and EF%: IABP increased cardiac output by 0.5-1 liters/ minute[24]. Bregman et al. showed a correlation graph of pressure and volume (Frank-Starling) shifted to the left, indicating that the function of left ventricular ejection was significantly improved[25]. Our study showed that EF improved from 24 hours after placing the balloon and increased significantly after 72 hours (EF% from 26.5 ± 13.5% to 34.6 ± 14.1%, p<0.05), cardiac output index (CI) improved after placing the ball 48 hours: 2.05 ± 0.5 to 3.9 ± 0.8/minute/m2; The survival group improved better than the mortality group after 24 hours of placing the ball: 32.1 ± 12.2% compared with 28.2 ± 12.6% (p<0.05), CI increased after 24 hours: 4.0 ± 1.5 compared with 2.2 ± 0.5 l/min/m2 (p<0.05).
Changing of SVR: SVR has been used in the treatment of cardiogenic shock after MI in many European countries (Germany, Austria), SVR value: 800-1000, MBP: 65-75 mmHg, CI>2.5 is the desired target in the treatment of cardiogenic shock after MI. In the study, SVR after 72 hours: 986.7 ± 89.5 compared with 1316.3 ± 112.8; the difference between the survival and mortality groups at 24 hours after placing the ball (926.7 ± 90.1 compared to 1185.1 ± 101.5, p<0.05).
Changing of lactate concentration and urine output: Results showed that lactate concentration decreased significantly after 24 hours: 7.9 ± 4.2 mmol/l decreased to 3.1 ± 1.1 mmol/l, the difference between the survival and mortality groups in the 24th hour after placing the ball (2.2 ± 1.5 against 3.9 ± 1.4). The amount of urine increased significantly after 24 hours: 15.1 ± 10.3 compared to 91.5 ± 15.3 ml/hour. The difference between the two groups: survival and mortality at the 12th hour after placing the ball (98.5 ± 15.9 vs. 80.1 ± 15.1).
Vasopressors and inotropes dose: In our study, the dose of dobutamine was significantly reduced from 14.8 ± 5.5 to 14.6 ± 5.5 μg/kg/min, noradrenaline from 0.68 ± 0.89 decreased down to 0.026 ± 0.03μg/kg/min after 48 hours of putting the ball and adrenaline from 0.91 ± 0.17 to 0.12 ± 0.33 μg/kg/min. The results of the study were similar to the conclusions in previous studies[26].
Differences in hemodynamic indicators of subgroups: The group was placed the ball before 12 hours, at the time of withdrawing: the heart rate, MAP, urine, lactate significantly improved compared to the group placed the ball after 12 hours, respectively: 99.2 ± 20.4 compared to with 105.2 ± 7.1 beats/ minute, 82.9 ± 12.4 compared with 77.6 ± 11.2 mmHg, 107.3 ± 24.2 compared to 100.5 ± 39.6 ml/hour, 1.3 ± 0.6 vs. 4.0 ± 2.3 mmol/l. The group that placed the ball before 12 hours of the hemodynamic indexes (EF%, CO, CI, SVR) improved better than the group who placed the ball after 12 hours.
In this study, there were 29/45 patients (64.4%) who received PCI in combination with IABP (IABP + PCI), in this group, heart rate, MAP, urine, lactate improved markedly compared to the group that placed the ball only, respectively: 97.6 ± 20.8 compared with 114.1 ± 8.1 beats/minute, 86.4 ± 11.1 compared with 78.5 ± 11.5 mmHg, 105.1 ± 22.1 compared to 90.4 ± 35.1 mmol/hour, 1.5 ± 0.8 compared with 4.4 ± 2.2 mmol/l. The group (IABP + PCI) has hemodynamic indexes that improve markedly compared to the group that only places the ball.
Efficacy of treatment and complication of intra-aortic balloon pump counter-pulsation (IABP) in the treatment of cardiogenic shock after myocardial infarction
Duration of treatment and time of shock release: The study showed that the average time of cardiogenic shock was: 8.5 ± 55.37 hours, average resuscitation days: 5.81 ± 8.21 days, average ventilation time: 121,1 ± 102.2 hours. The time from cardiogenic shock to the placement of IABP was 12.62 ± 11.37 hour, the number of hours saved is 58.33 ± 40.14 hours, the shortest was 4 hours, the longest time was 10 days, in which the percentage of patients were placed the ball early before 12h is 60%. The duration of shock escape was: 24, 1 ± 6.2 hours, the time for recovery of systolic blood pressure ≥90 mmHg of the groups: IABP + PCI, the group without acute renal failure, the EF group>40% and the group with the degree of Killip I-II at ICU is significantly faster than other groups.
The level of hemodynamic improvement after treatment: Hemodynamic indexes improved immediately after placing IABP and changed at 24-hour periods (MAP, lactate concentration, urine output), 48 hours (CI, vasopressor), 72 hours (heart rate); At the time of shadow withdrawal, hemodynamic indicators improved markedly: heart rate decreased to 89.2 ± 3.9 beats/minute compared with 125.1 ± 15.2 beats/ minute, MAP was 81.6 ± 16.1 mmHg, EF% 40,9 ± 10.8 compared with 26,5 ± 13,5%, CI: 3,9 ± 0.9 compared with 2,0 ± 0,5 L/min/m2, lactate decreased to 2.4 ± 0.8 mmol/l (p<0.05).
Efficacy of treatment and mortality: In this study, the survival rate was 64.4% (26/45 patients), the mortality rate was 35.5% (19/45 patients), this result was also consistent with AnvarBabaev (1994 - 2004) found that mortality rate significantly decreased (60.3% to 47.9%, p<0.001) (13).
In this study, the incidence of infection was 8.8% (infection at the balloon placement point was 6.6% and systemic infection 2.2%), 8.8% thrombocytopenia, local bleeding 4, 4%, anemia accounts for 4.44%. Limb ischemia 3% to 42% according to each study. We encountered 2 cases (4.44%) with mild Limb ischemic and patients had to be withdrawn ball earlier. The study did not record any thromboembolism that could lead to infarction and impaired function of other organs.
Conclusion
Intra-aortic balloon pump counter-pulsation is a minimally invasive, safe and effective hemodynamic support method for patients with cardiogenic shock after myocardial infarction, which has been successfully applied at the 108 Military Central Hospital, Hanoi Heart Hospital... should expand the application of this technique in the field of cardiopulmonary resuscitation to improve the effectiveness of emergency and treatment for patients with cardiogenic shock after myocardial infarction. Futureresearch need to be routinely applied in medical facilities, while evaluating the effectiveness and safety, stabilizing the Intra-aortic balloon pump counter-pulsation on many different indications with a large number of patients, follow-up for a long time, divided into different subgroups of patientsto optimize the effect of Intra-aortic balloon pump counter-pulsation in circulating resuscitation.
REFERENCES
- Aissaoui N. Improved outcome of cardiogenic shock at the acute stage of myocardial infarction: A report from the USIK 1995, USIC 2000, and FAST-MI French Nationwide Registries. Eur Heart J 2012;33:2535-43.
- Goldberg RJ, Spencer FA, Gore JM, et al. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction a population-based perspective. Circulation 2009;119:1211-19.
- Udith J. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. N Engl J Med 1999;341:625-34.
- Robert JG, Navid AS, Jorge Y, et al. Temporal trends in cardiogenic shock compicating acute myocardial infarction. N Engl J Med 1999;340:1162-68.
- Hasdai D, Topol EJ, Califf RM, et al. Cardiogenic shock complicating acute coronary syndromes. Lancet 2000;356:749-56.
- Thiele H, Ohman EM, Desch S, et al. Management of cardiogenic shock. European Heart Journal 2015;36:1223-30.
- Lee KW, Norell MS. Cardiogenic shock complicating myocardial infarction and outcome following percutaneous coronary intervention. Acute Cardiac Care 2008;10(3):131-43.
- Thiele H, Allam B, Chatellier G, et al. Shock in acute myocardial infarction: The Cape Horn for trials? Eur. Heart J 2010;31:1828-35.
- Fishberg M, Hitzig M. Circulatory dynamics in myocardial infarction. Arch Intern Med 2020;54:997-1019.
- Duvernoy CS, Bates ER. Management of cardiogenic shock attributable to acute myocardial infarction in the reperfusion era. Journal of Intensive Care Medicine 2005;20:188-98.
- Kantrowitz A. Mechanical intraaortic cardiac assistance in cardiogenic shock: Hemodynamic effects. Arch Surg 1968;97:1000-04.
- Mathey DG, Schofer J, Kuck KH, et al. Transmural, haemorrhagic myocardial infarction after intracoronary streptokinase. Clinical angiographic, and necropsy findings. Br Heart J 1982;48:546-51.
- Iakobishvili Z, Hasdai D. Cardiogenic Shock: Treatment. Medical Clinics of North America 2007;91:713-27.
- Cheung AW, White CW, Davis MK, et al. Short-term mechanical circulatory support for recovery from acute right ventricular failure: Clinical outcomes. J Heart Lung Transplant. 2014;33 (8):794-9.
- Cotter G, Kaluski E, Milo O, et al. LINCS: L-NAME (a NO synthase inhibitor) in the treatment of refractory cardiogenic shock: A prospective randomized study. Eur Heart J 2003;24:1287-95.
- Jacobs AK, Leopold JA, Bates E, et al. Cardiogenic shock caused by right ventricular infarction: A report from the SHOCK registry. J Am Coll Cardiol 2003;41:1273-9.
- Cheng JM, Valk SD, den-Uil CA, et al. Usefulness of Intra-Aortic Balloon Pump Counter-pulsation in Patients With Cardiogenic Shock from Acute Myocardial Infarction. Am J Cardiol 2009;104:327-332.
- Bregman D, Casarella WJ. Percutaneous Intraaortic Balloon Pumping: Initial Clinical Experience. Ann Thorac Surg 1980;29(2):153-5.
- Ibanez B, James S, Agewall S. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal 2018;33(20):2569-619.
- Diepen SV, Katz JN, Albert NM, et al. Contemporary management of cardiogenic shock: A scientific statement from the American Heart Association. Circulation 2017;136:232-68.
- Holmes DR, Bates ER, Kleiman NS, et al. Contemporary reperfusion therapy for cardiogenic shock: The GUSTO-I trial experience. J Am Coll Cardiol 1995;26(3):668-74.
- Hochman JS, Sleeper LA, Webb JG, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock. N Engl J Med 1999;341(9):625-34.
- Patel MR, Smalling RW, Thiele H, et al. Intra-aortic balloon counter-pulsation and infarct size in patients with acute anterior myocardial infarction without shock: The CRISP AMI randomized trial. JAMA – J Am Med Assoc 2011;306 (12):1329-37.
- Ghali WA, Ash AS, Hall RE, et al. Variation in hospital rates of intraaortic balloon pump use in coronary artery bypass operations. Ann Thorac Surg 1999;67(2):441-45.
- Bregman D, Nichols AB, Weiss MB, et al. Percutaneous intraaortic balloon insertion. Am J Cardiol 1980;46(2):261-4.
- Hollenberg SM, Kavinsky CJ, Parrillo JE. Cardiogenic Shock. Ann Intern Med 1999;131(1):47-59.