The effect of weight loss surgery on the risk of colorectal cancer
Received: 04-Jan-2023, Manuscript No. pulpjsr- 23-6361 ; Editor assigned: 08-Jan-2023, Pre QC No. pulpjsr- 23-6361 (PQ); Accepted Date: Jan 27, 2023; Reviewed: 20-Jan-2023 QC No. pulpjsr- 23-6361 (Q); Revised: 25-Jan-2023, Manuscript No. pulpjsr- 23-6361 (R); Published: 30-Jan-2023
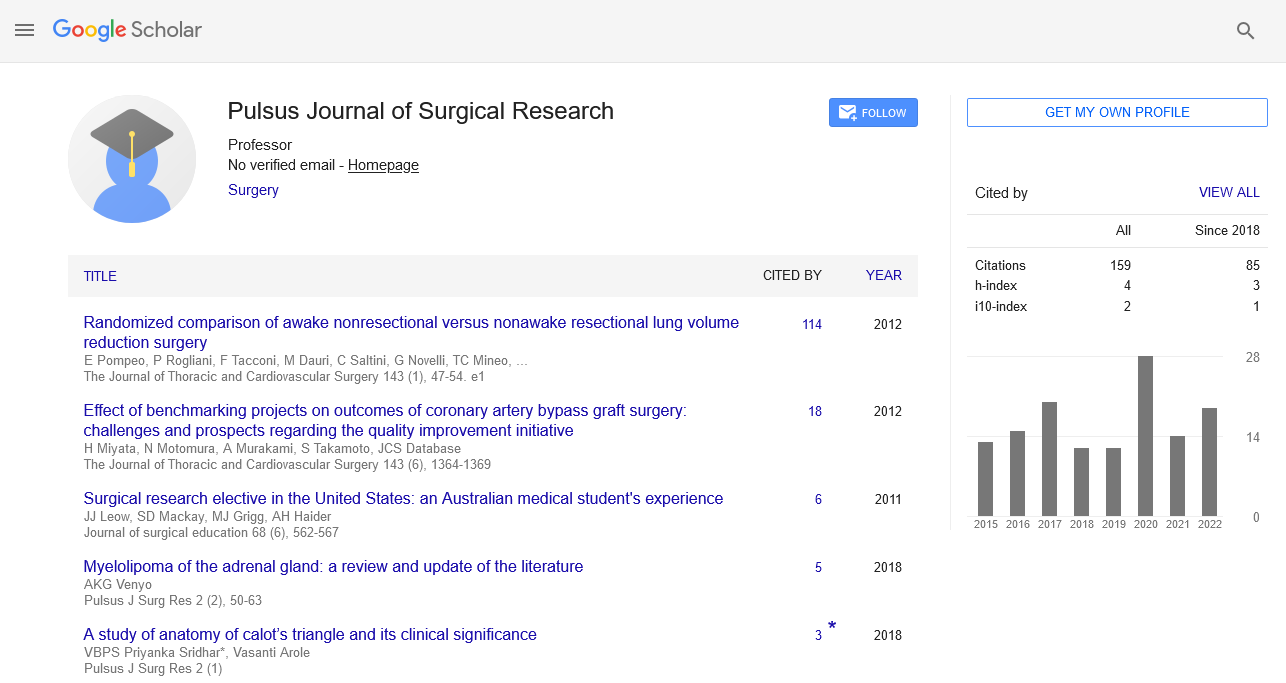
Citation: Johnson N . The effect of weight loss surgery on the risk of colorectal cancer. J surg Res. 2023; 7(1):10-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Obesity is thought to increase the chance of developing many cancers, including colorectal cancer (CRC). In addition to lowering overall cancer risk, bariatric surgery has been linked to improvements in co-morbidities brought on by obesity. However, the effect of bariatric surgery on CRC risk is debatable given the contradictory results of various cohort studies. Additionally, after Roux-en-Y gastric bypass (RYGB), evaluation of CRC biomarkers has shown hyperproliferation and elevated pro-inflammatory gene expression in the rectal mucosa. Alterations in the gut microbiota and exposure to high bile acid concentrations in the colorectum, both of which are brought on by RYGB-induced anatomical rearrangements, are the two hypothesised pathways for increased CRC risk. The parallels between the RYGB-induced microbial profiles and the gut microbiota seen in CRC have been noted in studies in both animals and humans.
Key Words
Surgical care; Cardiovascular disease; Colorectal surgery; Vascular surgery
Introduction
The global rate of obesity is significantly rising. In more than 20 countries, the prevalence of obesity doubled, and it rose in the majority of other nations. About of the adult population worldwide is obese, and this number is projected to rise. Because of the morbidity and mortality, it causes, obesity has become a serious public health problem. Type diabetes, cardiovascular conditions, nonalcoholic fatty liver disease, and various malignancies have all been linked to excess body weight. Medical care and bariatric surgery are two treatment options for obesity. When suitable nonsurgical treatment has failed to help a patient lose weight or keep it off over the long term, surgery is a viable alternative. Patients with a BMI of 30 or higher should think about having bariatric surgery if they have co-morbidities that are expected to improve with weight loss. This recommendation has increased dramatically in many nations and is expected to continue to rise as the prevalence of obesity rises. The International Federation for the Surgery of Obesity and Metabolic Disorders has reported that there has been a rise in the overall number of bariatric surgery procedures performed globally. Numerous studies have demonstrated that bariatric surgery is superior to nonsurgical treatment in encouraging long-term weight loss, as well as in resolving or improving type of diabetes, lowering the incidence of adverse cardiovascular events, and lowering the mortality rate.
Reduced cancer incidence and a better prognosis have been linked to bariatric surgeries through both weight loss-dependent and weight loss-independent pathways. These processes include reductions in oxidative stress and systemic inflammation as well as adjustments to gastrointestinal hormones, the gut flora, and the metabolism of fat, glucose, and bile.
Most obviously, obesity-related malignancies such hormonerelated and gastrointestinal tumors are protected from cancer risk and development by bariatric surgery. Contrarily, the impact of bariatric surgery on Colorectal Cancer (CRC) is unclear and debatable because some research indicates an elevated risk while others show a decreased risk. With an estimated million new cases and approximately fatalities globally, CRC is the third most often diagnosed disease and the second largest cause of cancer deaths. CRC is a complex illness caused by genetic, environmental, and lifestyle factors and is linked to a number of unchangeable risk factors. These include age, a history of IBD in the individual, and a history of CRC in the family. Lifestyle variables such as obesity, sedentary behavior, poor eating habits, drinking alcohol, and smoking are additional risk factors. Bariatric surgery-achieved weight loss is anticipated to lower the risk of CRC because obesity is a risk factor for this malignancy. The complicated and contentious nature of this association is reflected by the contradictory findings of numerous investigations. We therefore sought to assess whether bariatric surgery increases the risk of CRC and explore potential contributing pathways in this analysis.
Weight-loss procedures
Bariatric procedures are divided into major categories based on how they work to help people lose weight. Malabsorptive bariatric surgery reduces nutrient absorption by partially bypassing the small intestine. In restrictive operations, the stomach's volume is significantly decreased to help patients feel full sooner after eating. Another substantial group of bariatric surgeries combines malabsorptive and restrictive elements; these procedures entail a sizable reduction in the amount of gastric capacity that is available together with the bypassing of a portion of the proximal small intestine. The most often used bariatric procedure nowadays is laparoscopic sleeve gastrectomy (LSG), a restrictive procedure. In LSG, the greater curvature of the stomach is severed and removed, leaving just a small tube along the smaller curvature. This method is more common than malabsorptive ones since it encourages substantial weight loss, improves metabolic parameters, and carries a lower risk of consequences. The second most popular bariatric treatment today, Roux-en-Y gastric bypass (RYGB), combines malabsorptive and restrictive elements. In order to produce the Roux or alimentary limb, which is where ingested nutrients pass, a gastric pouch is formed from the upper stomach and is then anastomosed to the jejunum.
discovered a higher incidence of CRC in obese patients receiving surgery. For the obese surgical cohort, a standardized incidence ratio (SIR) for CRC was reported, and it grew with time. In contrast, the SIR remained steady throughout time in the obese no-surgery population. The protracted natural history of colorectal carcinogenesis, from normal mucosa to malignant lesions, is consistent with the increased risk of CRC occurring years or more after surgery. In all studies, bariatric surgery included both restrictive and malabsorptive techniques, including as vertical banded gastroplasty and adjustable gastric banding. A connection between increased CRC risk and RYGB was found in a large cohort research, however neither sleeve gastrectomy nor gastric banding had this association. Similarly, a Nordic cohort research showed that people who had undergone bariatric surgery had a greater risk of colon cancer, which increased further over time. In contrast, although it seemed to rise with longer follow-up periods, the risk of rectalcancer was not significantly elevated after bariatric surgery. These findings are consistent with those of a retrospective study. that looked at the possibility of colorectal polyp formation after RYGB. The authors compared colonoscopies conducted a year or more after surgery with presurgery colonoscopies in order to concentrate on the long-term effects of RYGB. Results showed a larger percentage of serrated polyps (precursors of CRC) one or more years after surgery, indicating a higher risk of developing precancerous lesions after RYGB.
In addition to affecting CRC incidence, bariatric surgery also seems to have an impact on prognosis. According to a cohort research by Tao et al., patients with CRC who had previously received bariatric surgery had greater mortality rates and a worse prognosis than those with CRC who had not had such surgery and had obesity. Separate analyses revealed a more than threefold rise in the mortality rate for patients with rectal cancer, but no statistically significant increase in the mortality rate for patients with colon cancer. The findings of a metaanalysis carried out. contradicted the unfavorable effects of bariatric surgery that were discovered in these investigations. Despite the small number of studies included in this meta-analysis and the short amount of follow-up, it was shown that bariatric surgery was linked to a decreased risk of CRC. Therefore, weight loss alone may have contributed to a lower CRC risk. Similarly, a retrospective observational research conducted in England found no link between obesity surgery and a higher incidence of CRC. The follow-up length and the small obese surgery group in this study, as opposed to the obese no-surgery population, were its weaknesses. Additionally, the Italian Society of Obesity Surgery's nationwide study of CRC incidence following LSG or RYGB indicated a low incidence of the disease years after surgery. Although data indicated that bariatric surgery had no effect on the development of CRC, the lack of no-surgery patients with obesity in the control group and the sparse number of cases observed made the evidence for this conclusion very poor, particularly when comparing LSG with RYGB. The characteristics and conclusions of the studies exploring the CRC risk after bariatric surgery are outlined in The need to probe more deeply into the mechanisms behind this relationship is highlighted by their inconsistent results. By performing complete crypt microdissection, mucosal biomarkers of proliferation such rectal epithelial cell mitosis, crypt area, and crypt branching were measured. Neocytokeratin immunohistochemistry was also used to assess apoptosis. Prior to surgery, obese patients showed higher rates of rectal epithelial cell proliferation than people of normal weight, supporting the association between obesity and the risk of CRC. Analysis of the same patients six months after RYGB showed a twofold increase in the number of mitoses per crypt in comparison to presurgery values. Following RYGB, there was an additional rise in rectal epithelial cell mitosis, which was followed by a decline in the proportion of apoptotic cells. Additionally, since the upper small intestine is bypassed during this treatment, some of the usual small intestine flora, like Enterobacteriaceae, may move to the large intestine.
The diminution of stomach size and associated pH adjustment are another significant RYGB modification
In fact, a smaller gastric capacity is linked to a large reduction in the amount of acid secreted in the gastrointestinal pouch, which raises pH levels. There is a dearth of research on LSG's impact on gastric acid secretion. As certain acid-producing cells are still present, it has been hypothesized that the structural changes related to this bariatric treatment may similarly lessen stomach acid output, albeit to a smaller amount than RYGB. Since it creates a more favorable environment for Bactericides and suppresses the growth of butyrate-producing bacteria, raising the pH in the gastrointestinal system causes significant changes in the gut bacterial communities. This proof is verified. They examined in vitro how microbial communities responded to a rise in pH and discovered a rise in the abundance of the genus Bactericides and a decline in Rosebery species and Faecalibacterium prausnitzii. The two main butyrate-producing bacteria in the human gut, Rosebery spp. and F. prausnitzii, are thought to have a protective function because to the advantageous and anti-inflammatory properties of butyrate. Decreased levels of both bacterial groupings (belonging to the Formicates phylum) have been seen in post-surgery patients.
An indirect consequence of RYGB is altered microbial catabolism, which generates alterations in metabolite levels. After RYGB, less gastric acid is secreted, which generally ensures that proteolytic enzymes are activated and that proteins are broken down. As a consequence, more incompletely digested proteins reach the colon, leading to increased microbial protein catabolism. In turn, putrescine and other hazardous polyamines are produced at higher levels. Given putrescine's detrimental effects on cell survival, it is likely that the highly cytotoxic faucal water from post-RYGB rats correlates with a postoperative rise in putrescine levels. Importantly, it has been observed that the levels of putrescine and other polyamines are raised in patients with cancer and are connected with tumor stage and progression. Relevant to this finding, putrescine appears capable of stimulating cell proliferation in a dose-dependent manner. Furthermore, the accumulation of putrescine has been related with colon inflammation, elevated levels of pro-inflammatory cytokines, and increased intestinal permeability. Various human investigations have documented, in the gut, the increased abundance of oral bacteria including Streptococcus spp., Villanelle spp., and Fusobacterial nucleate following RYGB. Intestinal colonization by the oral microbiota could be connected to higher pH and decreased acid secretion, which impair the efficacy of the gastric barrier, enabling the orofacial transit of bacteria.
Interestingly, there are significant parallels between the fecal microbial profiles reported following bariatric surgery (particularly RYGB) and those of patients diagnosed with CRC. Indeed, multiple studies have investigated and compared gut microbiota composition in patients with CRC and healthy persons, indicating enrichment of the phylum Fusobacterial and the genera Bactericides and Escherichia in the CRC group. furthermore, the results of these research reveal considerably decreased abundance of the butyrate-producing genera Faecalibacterium and Rosebery in patients with cancer, compared with controls. reported similar results using a murine model of CRC, observing increases in Proteobacteria, Fusobacterial, and Bactericides populations and significant reductions in Rosebery and Eubacteria abundance.
Therefore, the microbial symbiosis associated with CRC leads to both enrichments of pro-inflammatory microbes and depletion of butyrateproducing bacteria, resembling the consequences of RYGB. A key element linked to inflammation and carcinogenesis that appears to regulate CRC risk and development is altered microbiota makeup.