The first comparative study of financial costs of treatment of venous ulcers at a dermatology one stop clinic followed up by specialized nurses in the community compared to standard care: A prospective pilot study
2 University of Twente, Drienerlolaan 5, 7522 NB Enschede, Netherlands
3 DermaTwente, Dr. Poelsstraat 63B, 7572 ZV Oldenzaal, Netherlands, Email: narcis@dans.knaw.nl
Received: 08-Jun-2020 Accepted Date: Jun 22, 2020; Published: 27-Jun-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: As our general population ages, the prevalence of venous leg ulcers is increasing. The disease consumes substantial healthcare resources and the financial burden of VLU care is increasing. Multiple implementations aimed at cost reduction have not yielded the expected results. Because we know that healthcare organisation can be an important target of cost reduction, we have created a new healthcare chain for diagnosing and treating venous leg ulcers.
Keywords
Chronic venous disease; Leg ulcers; Cost effectiveness; Wound care.
Introduction
Venous leg ulcers (VLU) are a major burden for health care systems around the world, especially with an ageing population and an increasing prevalence [1,2]. It is estimated that 1% of Western health care budgets are compromised by venous ulcer care [3,4]. VLU’s have a tendency to lead to chronic wounds [5] and therapy could take months [5,6]. Ulcers are invalidating and painful and could greatly reduce patient’s quality of life limiting daily activities, such as work. Ulcer healing has been shown to restore quality of life [7]. VLE are often caused by underlying venous insufficiency and accounts for 70% of all leg ulcers [1-8,9]. Treatment consists of compression therapy and local wound treatment such as various wound dressings, debridement, excision of the ulcer or skin grafting (9-12) and aim for faster wound healing. Early treating venous insufficiency as underlying cause by superficial venous surgery can reduce the chance of a recurrent ulcer and result in faster ulcer healing [13,14]. The nature of the wound, ulcer size and duration determines the healing chances and therefore the type of treatment. Diagnosing and treatment by experienced and trained healthcare professionals is required [15]. Establishing a quick and correct diagnosis and initiating proper treatment will result in a shorter time of wound healing, restoring of quality of life and simultaneously a cost reduction is expected.
Current study in broader context
At the end of the last century, specialized leg ulcer care clinics were introduced providing wound care. Studies investigating ulcer care already showed that diverse concepts such as centralizing ulcer care in a nurse-led clinic or an outpatient clinic improve time to wound healing an can reduce costs [16-18]. Though in these studies vital patients were included with a good ability to visits clinics, not representing the total population, which often suffer more comorbidity. Nevertheless, with increasing evidence that standardized based ulcer care is efficient in both financial as medical outcomes, primary ulcer care in the Netherlands, as within other countries, is still within the responsibility of the general practitioner (GP), who can delegate the actual treatment to districts nurses, medical assistants and other therapists and might refer to a specialist when an chronic ulcer is developing [19]. Other studies showed that the organisation rather than the location of care is most important; using proper evidence based treatment standards for home care organizations would lead to similar outcomes with hospital care with similar outcomes and this even led to cost reduction [20-22]. With the continuing ageing of the population the prevalence of VLE increases. In the Netherlands, government policy focuses on the independence and selfreliance of older patients in the home situation and therefore ulcer care too is preferably provided at home. In line with the aforementioned and the recognition of value-based medicine, we wanted to create an unique organisation structure in with both a centralized ulcer care clinic and a proper functioning home care treatment method were combined.
Aim of the Study
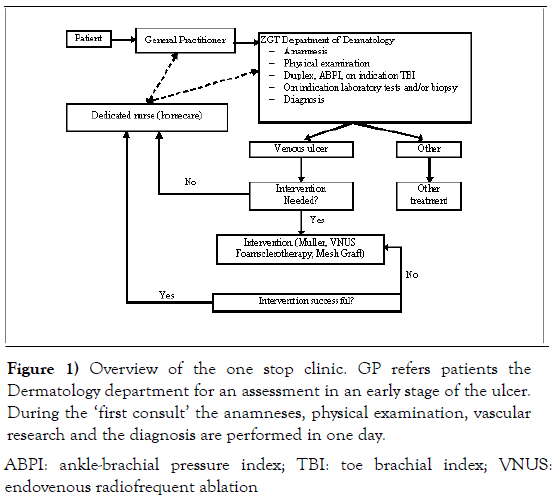
Despite aforementioned evidence of early treatment of underlying causes and attempts to chance ulcer care, the system of ulcer care has not been changed for years [16-22]. Therefore we set up a new system of uniting previously proven different healthcare concepts. In this situation, at an early stage of the disease, a diagnosis was made in one day in the hospital outpatient clinic and subsequently home care organizations delivered evidenced based (dedicated nurses) care at home and, if necessary, additional treatment was given at the hospital. The system is shown and explained in Figure 1.
Figure 1: Overview of the one stop clinic. GP refers patients the
Dermatology department for an assessment in an early stage of the ulcer.
During the ‘first consult’ the anamneses, physical examination, vascular
research and the diagnosis are performed in one day.
ABPI: ankle-brachial pressure index; TBI: toe brachial index; VNUS:
endovenous radiofrequent ablation
Supplementary 1 shows the system of dedicated nurses. At the Dermatology department of the ZGT hospital in the East of The Netherlands we investigated if implementation of the new set up would be cost-effective. Our hypothesis was that this new method would lead to cost reduction in comparison with the standard way of care in the Dutch system of venous ulcer care. With this pilot study we could furthermore explore which cost items exists, therefore creating a foundation for further research. The primary research question of this pilot study is: is there a difference in primary health-care costs (in euros) between the new method at the one stop clinic compared to the standard ulcer care?
Materials and Methods
Study design
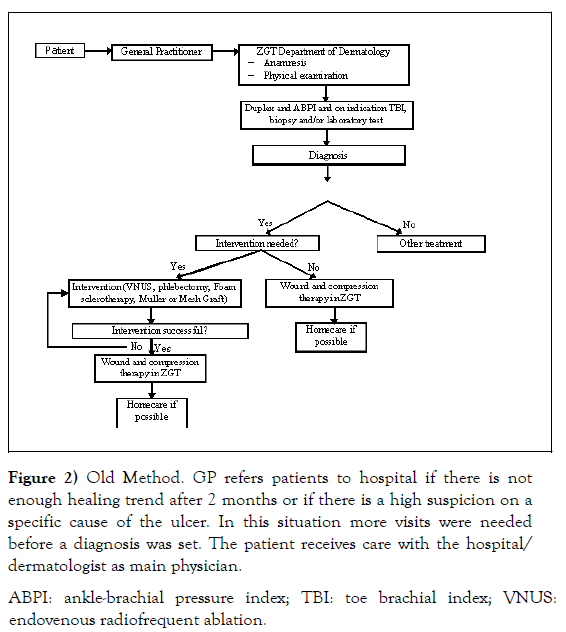
Little prior research has so far been conducted to investigate the financial costs of different systems of VLU care in terms of cost-effectiveness and efficiency. Hence, because of this, no weighted decision could be taken for required estimates for a power analysis research. So we conducted a small prospective pilot study to investigate our hypothesis and create a foundation for further research. Therefore we used the standard treatment design in the Deventer Hospital, which is representative for VLU care in the Netherlands. This system is shown in Figure 2.
Figure 2: Old Method. GP refers patients to hospital if there is not
enough healing trend after 2 months or if there is a high suspicion on a
specific cause of the ulcer. In this situation more visits were needed
before a diagnosis was set. The patient receives care with the hospital/
dermatologist as main physician.
ABPI: ankle-brachial pressure index; TBI: toe brachial index; VNUS:
endovenous radiofrequent ablation.
Secondary outcomes were number of visits, ulcer size, time to wound closure, time per visit, cost of supplies and general overhead cost per patient per visit. We used the CHEERS reporting guideline as a guiding principle for structure of this cost-effectiveness analysis [23].
Data collection
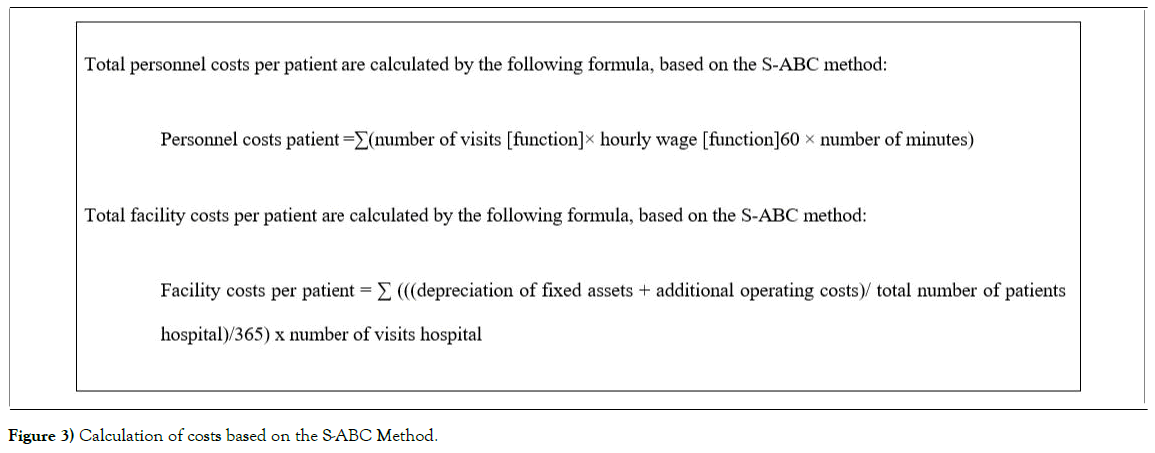
Financial costs were calculated through the Simplified Activity Based Costing (S-ABC) method to calculate actual costs per patient Figure 3.This method is known to be a more reliable method compared to volume based costing. Each event is an ‘activity’ and for each activity a specific cost item is created. The S-ABC uses less cost items compared to the ABC method and therefore is more valuable to implement in a pilot study. To determine the activities, all factors relating to financial cost of VLU care, were identified with both qualitative and quantitative research. For qualitative research health care professionals were interviewed to collect data as wages, total working hours and average unit costs for the funding of diagnosing and treating VLU. To calculate the actual costs per patient we first reviewed all patients’ records to collect data such as patient characteristics and data about wound size, time to wound closure, number of visits and time per visit [24]. Time for wound closure was the time between first visit up to last consult of any healthcare professional involved the treatment process. At last, facility (overhead) costs were identified using the annual reports of both hospitals, which were divided by all patients in the hospitals as in line with the S-ABC method. All costs were expressed in euros and no conversion to another currency was made. The value of all unit items was based on the value at the time of the trial. In this trial we focused only on costs of logistics and on organisational level, we did not add costs as bandaging and other wound care products as this was beyond the scope of this trial. However, these costs are known to be a major part of the total costs of VLE and are too subject of debate in reduction health care costs.
Patient selection
A random sample using a randomisation program was conducted from all patients with an VLE attending ZGT and Deventer Hospital in the period between January 2016 and February 2016. Due to the pilot study design this was not a formal randomized controlled trial and we included a limited amount of patients. The relatively small study period was chosen since the current study focussed on the new method in diagnosing and setting up a treatment plan of new venous ulcer and not on long term consequences. Patients in the research group all participated in the one-stop clinic. All included patients have had a new venous leg ulcer. We followed these patients till the wound was healed and did not require any further treatment. All patients were 18 or more years of age. Inclusion criteria for the research group include new ULV patients of the one stop clinic at the ZGT who were treated in the home setting by dedicated home care nurses from two local homecare organizations (CarrintReggeland and Zorgaccent) between January 2016 and February 2017. The control group consists of patients according to the standard of care for VLU in the Deventer Hospital. Patients were excluded if they had any other cause of the ulcer after additional investigation (e.g., Doppler, ankle-brachial pressure index; toe brachial index) such as mixed ulcer, arterial, decubitus, diabetic, vasculitis, oncological, pyoderma gangrenosum, arteriolar or erysipelas or a recurrent ulcer and multiple ulcers.
Statistics analysis
The groups were normally distributed, and while we did not know in advance which pathway would be less expensive, we used unpaired, two sided t-tests to compare both groups. Continuous variables are expressed as mean with standard deviation (SD) or median with interquartile range (IQR); categorical variables as counts with corresponding percentages. Descriptive data is shown in tables and charts. Since the small number of the sample sizes, we used the bootstrapping method as statistical analysis for a better understanding of the results.
Results
Twelve patients were included in the research group. Eight patients were included in the control group. All patients (100%) were referred to the clinic by a GP, none of the patients was admitted for in-hospital treatment. Therefore no invasive interventions were performed in any patient. Baseline characteristics of all individual and combined groups are shown in Table 1.
| Variable | CarrintReggeland | ZorgAccent | ZGT (CarintReggeland+ ZorgAccent)* | Deventer Hospital | P-value (ZGT vs. Deventer Hospital)** |
|---|---|---|---|---|---|
| Sex (M/F), n (%) | 5 (71)/2 (29) | 4(80)/1(20) | 9(75)/3(25) | 4(50)/4(50) | 0.296 |
| Mean age, years (SD) | 4(80)/1(20) | 67.16 (12.69) | 62.08 (13.81) | 69.88 (11.54) | 0.19 |
| Mean time of treatment, days (SD) | 73.00 (72.47) | 126.20 (135.97) | 95.17 (101.68) | 78.50 (38.96) | 0.615 |
| Mean ulcer size, cm2 (SD) | 2.07 (1.81) | 5.36(8.6) | 3.15 (4.19) | 4.6(3.84) | 0.414 |
Table 1: Baseline characteristics of all groups.
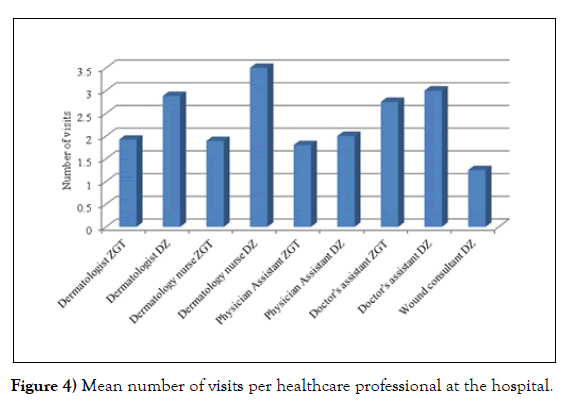
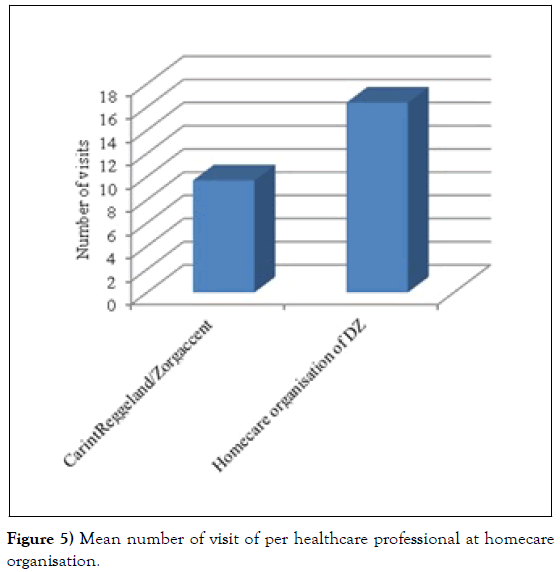
The groups did not alter significantly regarding baseline characteristics. In Figure 4 and 5 the mean number of visits per healthcare professional in the hospital and at home are described.
Figure 4: Mean number of visits per healthcare professional at the hospital.
Figure 5: Mean number of visit of per healthcare professional at homecare organisation.
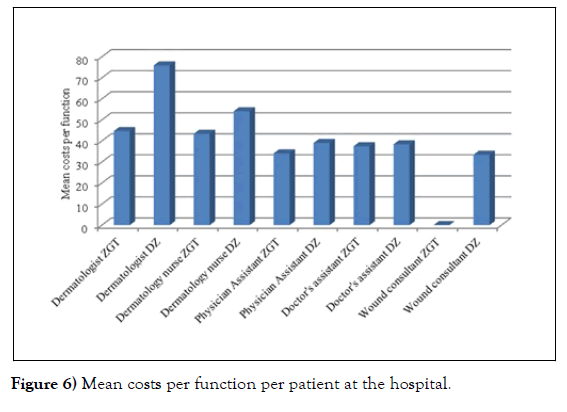
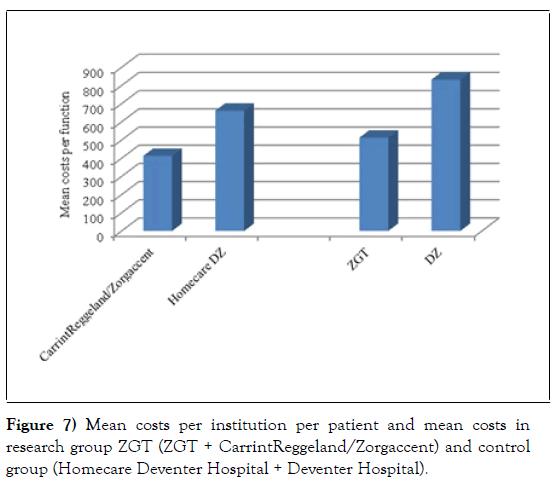
We converted all visits with the actual time per visit, per healthcare professional, with their corresponding wage and calculated the mean costs per function and per institution and eventually the mean total costs of each patient. The results are listed in Figure 6 and 7.
For almost each type of healthcare professional the mean costs per patient are more expensive in the control group in comparison with the research group, often due to less visits.
Facility costs per patients for each hospital were calculated for the year 2016 for the total number of visits for each hospital; €1.96 (research group)vs. €1.07 (control group). The mean total costs per patient with an VLU in this study were based on the total personnel costs and the facility costs.
The mean total health care cost of a treatment with the new method was € 522.85vs.€ 841.17 in the standard way of ulcer care (p=0.093) (Figure 4). The mean number of visit in the hospital was 5 in the research group and 9 in control group (p=0.177). The mean number of visits by nurses was 10 in the research group compared to 17 visits in the control group (p=0.236). The mean number of days of treatment was in the research group 96 days, whereas in the control group the mean number of days of treatment was 79.
Due to the small number of total sample size, we used the bootstrap method for extending the total sample size to a fictional 1000 patients in both groups. This method does not make up for the small sample size. However bootstrapping shows more reliable results as representation of the population instead of using the original sample size, since it accounts for different statistical errors and distortions since virtual larger population. Statistical analysis after bootstrapping the difference showed significant differences between the groups for mean total health care costs €618.97 (research group)vs.(€ 744.36 (control group), p<0.001.
Discussion
In this trial we compared the difference in costs between the new treatment pathway and the standard way of VLU care. The one-stop clinic was introduced to decrease the number of visits to the hospital by setting a fast and correct diagnosis, set up a treatment plan in the hospital and, if possible, continue the ulcer care in home setting by specially trained wound care nurses. After statistical analysis with bootstrapping method we found an absolute difference of €125.39 (€618.97 for one-stop clinic vs. €744.36 in usual care), which is more than 16% reduction, p<0.001. These number indicate that this innovative new concept of combining centralized care for VLE in combination with a standard and evidenced based treatment in home setting is cost effective and saves resources. In an ever increasing population with patients physically incapable of frequent visiting an outpatient clinic this is an important issue in organizing health care.
Since the design of this first unique pilot study, large-scale follow-up research in a prospective design can provide a better insight into the differences and correlations of all costs concerning VLU care. Our study showed that the absolute number of visits to the hospital and visits by dedicated wound care home care nurses at home was less compared to the standard care. The time for wound healing was longer compared to the control group, whereas we expected this to be less since the proper and fast initiation of treatment by the one stop clinic, however, this is a secondary outcome for which the study was not powered. There was not a difference in mean ulcer size between both groups which could explain the difference. However, prior research investigating time to wound healing showed that centered care would lead to less time to wound healing, which is not corresponding with our current results [22]. In the new method, the dedicated home care nurses are specifically trained to monitor and treat VLU, which could explain the smaller number of visits in the research group. In our study we determined the costs by using the S-ABC method by collecting all direct costs of personnel, overhead costs (including unit costs). Follow-up research should attempt to gather the costs of all domains, such as wound material and costs of additional invasive treatment. We calculated the personnel costs by multiplying total time of care with the wages of different types of health care professionals. In another study investigating the costs of VLU care, the total personnel costs were based on a total working hours per month (150 hours) and there was an additional increase of almost 30% for profit purposes [25]. We choose only to calculate the exact actual costs and not add any value for profit benefits. The purpose of this study was to evaluate methods for improving health care and cost effectiveness in wound care. Known factors, such as wound size, duration of the wound, prior history of ulcer are negatively reduction wound closure [26]. Other aspects as proper indications for and time till referral to a specialist, the amount and length of compression therapy and the use of various wound dressings are still topics of current research. Further research combining these aspects in ulcer care is necessary for gaining insight and indicate processes where improvement could be achieved.
Limitations
A large limitation is the small number of patients, however this is the first unique study combining an one stop clinic with an integrated specialized home care system. Since the pilot design of the study the results are indicative for a cost reduction by implementation of this system of ulcer care. While bootstrapping as methodologically method shows more reliable results for statistical purposes, is does not make up for the small sample size. Enlarging the sample size by bootstrapping gave us an insight in the costreduction that would be acquired in a larger population. We carefully calculated the costs items of each type of health care professional involved in VLU care. Separate costs of diagnostic investigation such as duplexgraphy were not taken into account as we assumed these costs were similar for patients during the diagnostic process and are covered under overhead costs. Since none of the patients was treated for underlying causes of VI, no cost of invasive treatment was collected. For practical reasons the overhead costs of the organization have been divided proportional to all patients in the hospital for the year 2016 for both hospitals as we think this was the most reliable way for inclusion of the hospital overhead cost in this pilot study. The relatively small study period was chosen since the current study focussed on the new method in diagnosing and setting up a treatment plan of new venous ulcer. Since the chronicity of the condition, further research should address long term outcomes concerning health care costs. Analysis of indirect costs such as travel time (both for nurses as patients), saved socioeconomics costs as saved working days etc. was beyond the scope of this trial. Although some (in) direct costs were missed out, we think this study shows an adequate overview of the logistics and organisation costs in both the one stop clinic and the standard way of care for venous ulcer care. Since this selection bias, these outcomes do not must generalized for all ulcer care, but are an indication that one-stop clinics and dedicated nurses could lead to cost saving and be beneficial in the context of financial reasons.
Conclusion
The prevalence of patients with venous leg ulcers is increasing with an ageing population with more comorbidity. VLU have a substantial economic impact on health care systems and are often a chronic condition with an invalidating impact on patients’ lives. We initiated a new innovative method of treating VLU by implementation of an one-stop clinic at the outpatient clinic of the Dermatology department. In one visit, the medical history, physical examination and additional (vascular) examinations were performed. Furthermore we trained dedicated wound care nurses supplying ulcer care at patients ’ homes. To evaluate the cost-effectiveness of new strategy, we conducted a cost analysis study. We investigated all personnel costs and facility costs in relation to the ulcer care. The average health care cost of a treatment with the new method was €522.85 vs. €841.17 in the standard way of ulcer care (p=0.093). After bootstrapping the sample size since the small initial number of patients, we found an absolute difference of €125.39 (€618.97 vs. € 744.36) (p<0.001), which is more than 16% costreduction. This first pilot study shows that cost reduction is possible by introduction of new health care concepts. These outcomes must not be generalized for all ulcer care, but are an indication that one-stop clinics and well organized specialized home ulcer care could lead both to health care improvements be beneficial in the context of and economic consequences by cost saving.
Declarations
Conflicting interest
No potential conflict of interest relevant to this article was reported.
Funding sources
None
Data sharing statement
The data that supported the finding of this study are available from the corresponding author upon reasonable request.
Ethical approval
The local feasibility committee of the ZGT Hospital and the Deventer Hospital both approved this study.
Guarantor
The guarantor of this research project is dr. E.B.M. Kroft, MD, PhD.
REFERENCES
- Agale SV. Chronic Leg Ulcers: Epidemiology, Aetiopathogenesis, and Management. Ulcers. 2013: 9.
- Anderson I, King B. Mixed aetiology leg ulcers. Nurs Times. 2006; 102(16);45-50.
- Guest JF, Ayoub N, McIlwraith T, et al. Health economic burden that different wound types impose on the UK’s National Health Service. Int Wound J. 2017; 14(2): 322–30.
- Ma H, O’Donnell Jr TF, Rosen NA, et al. The real cost of treating venous ulcers in a contemporary vascular practice. J VascSurg Venous LymphatDisord. 2014;2(4): 355-61.
- Nicolaides AN, Allegra C, Bergan J, et al. Management of chronic venous disorders of the lower limbs: guidelines according to scientific evidence. IntAngiol. 2008;27(1): 1-59.
- Bergan JJ, Schmid-Schonbein GW, Smith PDC, et al. Chronic venous disease. N Engl J Med. 2006; 355(5): 488–98.
- Kahle B, Hermanns HJ, Gallenkemper G. Evidence-based treatment of chronic leg ulcers. DtschArztebl Int.. 2011: 108(14): 231–37.
- Graham ID, Harrison MB, Nelson EA, et al. Prevalence of lower-limb ulceration: a systematic review of prevalence studies. Adv Skin Wound Care. 2003;16: (6): 305-16.
- Nelson EA, Adderley U. Venous leg ulcers. BMJ ClinEvid. 2016;2016: 1902.
- O’Meara S, Cullum N, Nelson EA. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012: 11(11): CD000265.
- Montfrans VC, De Boer EM, Jansma EP, et al. Behandeling van patiënten met eenveneusulcuscruris. Watalscompressietherapiealleennietmeerhelpt? NederlandsTijdschriftvoorGeneeskunde. 2013;157(12): A5647.
- Jones JE, Nelson EA, Al-Hity A. Skin grafting for venous leg ulcers. Cochrane Database Syst Rev. 2013; 2013(1): CD001737
- Gohel MS, Heatley F, Liu X, et al. A Randomized Trial of Early Endovenous Ablation in Venous Ulceration. N Engl J Med. 2018; 378(22): 2105-114.
- Howard DP, Howard A, Kothari A, et al. The role of superficial venous surgery in the management of venous ulcers: a systematic review. European Journal of Vascular and Endovascular Surgery. 2008; 36(4): 458-65.
- Van Mierlo-van den Broek PA, de Laat HE. Verkenningwondbehandeling in Nederland. In opdracht van CVZ. Nijmegen. 2012;1-204.
- Manu CA, Mustafa OG, Bates M, et al. Transformation of the Multidisciplinary Diabetic Foot Clinic Into a Multidisciplinary Diabetic Foot Day Unit. The International Journal of Lower Extremity Wounds. 2014; 13(3): 173-9.
- Gottrup F, Holstein P, Jørgensen B, et al. A new concept of a multidisciplinary wound healing center and a national expert function of wound healing. Arch Surg. 2001; 136(7): 765–72.
- Rondas AALM, Schols JMG, et al. Cost analysis of one of the first outpatient wound clinics in the Netherlands. J Wound Care. 2015; 24(9): 426–36.
- Van Hof N, Balak FSR, Apeldoorn L, et al. NHG-StandaardUlcuscrurisvenosum(Tweedeherziening). Huisarts Wet. 2010;53(6): 321-33.
- Harrison MB, Van Den Kerkhof E, Hopman WM, et al. Evidence-informed Leg Ulcer Care: A Cohort Study Comparing Outcomes of Individuals Choosing Nurse-led Clinic or Home Care. Ostomy Wound Manage. 2011; 57(8): 38-45.
- Harrison MB, Graham ID, Lorimer K, et al. Leg-ulcer care in the community, before and after implementation of an evidence-based service. CMAJ. 2005; 172(11): 1447–52.
- B. Rook, M. Wikkerink, E. Kroft. Evaluation of the introduction of the one-stop clinic and dedicated nurses for the ulcer crurisvenosum care in the east of the Netherlands. Phlebology. 2020; 35(1): 27-38.
- Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Value Health.2013;16(2): e1-5.
- Westerdijk M, Zuurbier J, Ludwig M, et al. Defining care products to finance health care in the Netherlands. Eur J Health Econ. 2012; 13(2): 203-21.
- Baptista CMC, Castilho V. Cost survey of procedure with Unna boot in patients with venous ulcer. Rev Lat Am Enfermagem. 2006; 14(6): 944-9.
- Margolis DJ, Berlin JA, Strom BL.Which venous leg ulcers will heal with limb compression bandages? Am J Med. 2000;109(1): 15–9.