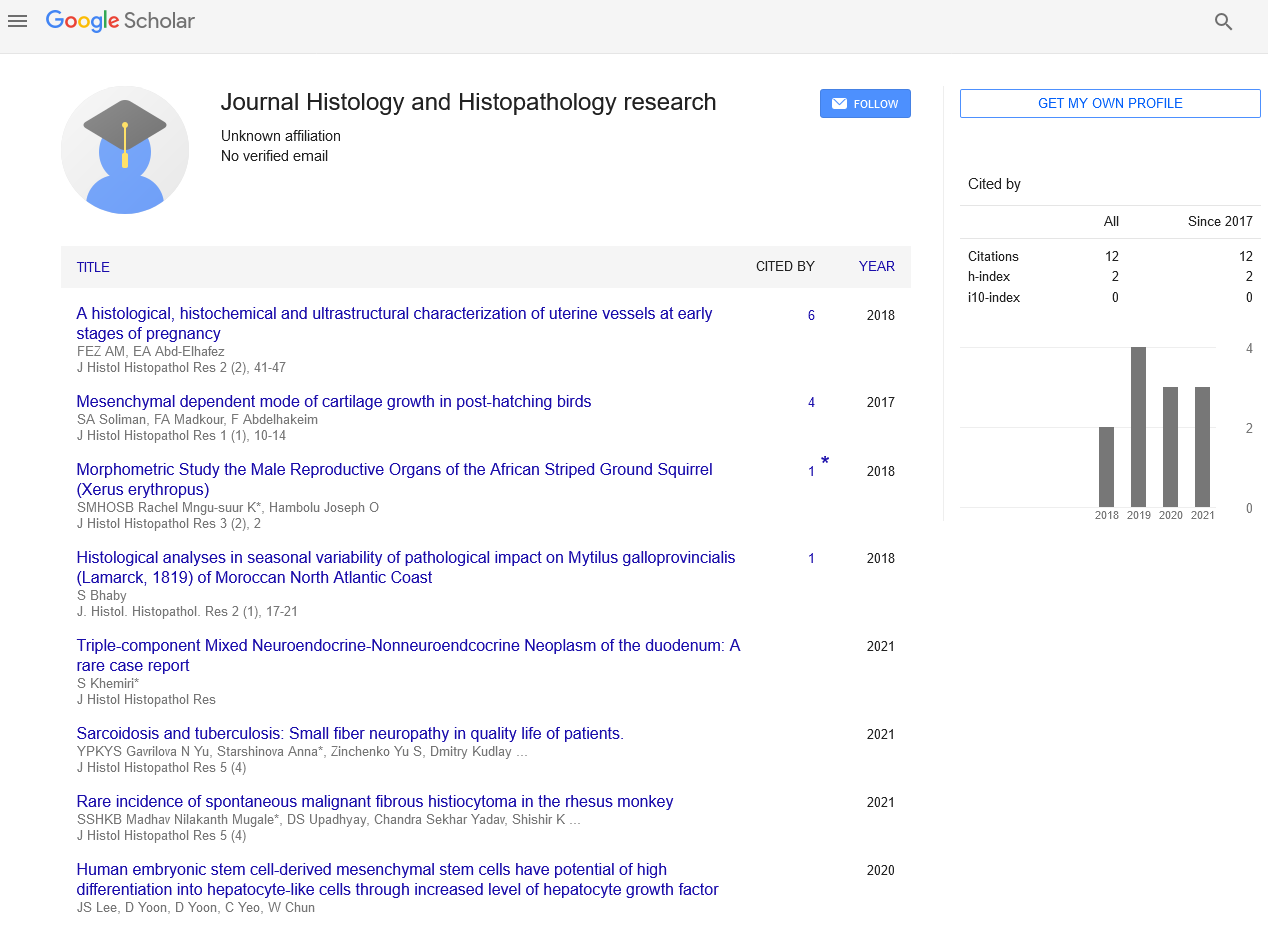
The pathological categorization of breast cancer: an update
Received: 01-Mar-2023, Manuscript No. pulhhr-23-6343; Editor assigned: 03-Mar-2023, Pre QC No. pulhhr-23-6343 (PQ); Accepted Date: Mar 22, 2023; Reviewed: 13-Mar-2023 QC No. pulhhr-23-6343 (Q); Revised: 15-Mar-2023, Manuscript No. pulhhr-23-6343 (R); Published: 27-Mar-2023, DOI: 10.37532/pulhhr.23.7 (1).1-2
Citation: Quinn S. The pathological categorization of breast cancer: An update. J Histol Histopathol Res 2023;7(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Breast Cancer (BC) is a heterogeneous condition that affects a wide range of tumours with various morphological, biochemical, and clinical characteristics. Although there may be phenotypic similarities across tumors, their biological behaviour and therapeutic response frequently differ. With the identification of distinct molecular subclasses, improvements in high-throughput molecular methods and bioinformatics have contributed to a better knowledge of BC biology and to the refining of molecular taxonomy. Although the traditional pathological morphological categorization of BC is crucial and offers diagnostic and prognostic information, the use of single gene and multigene tests to stratify BC into different groups to inform decisions about systemic therapy is now of interest. This study examines methods for categorising BC, along with their drawbacks, and places special focus on the critical significance of morphology in making a precise diagnosis of primary invasive cancer of the breast.
Introduction
Breast Cancer (BC) is a heterogeneous illness that encompasses a wide range of tumours with different morphological, biochemical, and clinical characteristics. Tumors frequently exhibit diverse biological behaviours and responses to treatment, despite the fact that their phenotypic characteristics may occasionally overlap. A better knowledge of BC biology and a more precise molecular taxonomy with the identification of distinct molecular subclasses have been made possible by advancements in high-throughput molecular methods and bioinformatics. Although the traditional pathological morphological categorization of BC is crucial and offers diagnostic and prognostic information, the current emphasis is in the use of single gene and multigene tests to stratify BC into different groups to inform decisions about systemic therapy. This study takes into account several BC categorization strategies, along with their drawbacks, and places special focus on the basic significance of morphology in determining a precise diagnosis of primary invasive cancer of the breast.
The normal existence of humans has been seriously threatened by the recent progressive rise in the prevalence of Breast Cancer (BC) across the world. Affected individuals tend to be younger, gender-neutral, and racially ambiguous. The International Agency of the World Health Organization projected that 2.1 million new cases of BC among women—or nearly 25% of all cancers occurred in 2018.In both rich and developing nations, there were significantly more female instances of cancer than any other type. For women between the ages of 20 and 60, BC is the most common malignancy that kills them. Effectively lowering risk and stopping cancer development are early detection and therapy. Breast B ultrasonography, dynamic enhanced magnetic resonance, pathological biopsy, and mammography are all used in the conventional diagnosis of BC.
In order to test and analyse sample data for cancer diagnosis and treatment strategy, pathologists often need to integrate the input from medical equipment with their own diagnostic experience. Diagnostic procedures are time-consuming, expensive, and arbitrary. Furthermore, it is challenging to provide patients in rural locations and developing nations with prompt and efficient medical care because of the unequal distribution of pathologists and medical resources worldwide. Therefore, an effective, affordable, and objective diagnostic approach has significant scientific value as well as societal relevance.
Breast Cancer (BC) is made up of a varied collection of tumours that differ significantly in terms of their clinical presentation, shape, molecular characteristics, biological behavior, and therapeutic response. Despite tremendous improvements in our knowledge of and approaches to treating BC, the disease continues to pose serious difficulties for global public health. BC was first identified 3500 years ago1, when it was categorised based on the disease's outward symptoms and indicators. Early surgical excision of a breast tumour before it had progressed to the axillary lymph nodes was proposed in the middle of the 18th century as a result of the discovery that cancer is a local illness that develops in phases rather than an ade novo systemic disease.
The identification of intrinsic molecular subtypes and the development of multigene signatures in the early 2000s marked a significant advancement in our understanding of BC and introduced the idea of molecular categorization of BC. Despite the importance of the established morphological prognostic factors in BC, this focus has dominated BC research over the past two decades due to the development of high-throughput molecular techniques like microarrays and next-generation sequencing. This focus is now rapidly expanding in response to the growing availability of targeted therapy and the shift towards precision and personalised medicine.
BC comes in two flavours benign and malignant. Early on, benign cancer has a high propensity to develop into malignant cancer. Adenosis, phyllodes tumor, fibroadenoma, and tubular adenoma are the primary benign cancers. Papillary carcinoma, ductal carcinoma, lobular cancer, and mucinous cancer are the four primary types of malignant cancer. More than 95% of them were ductal carcinoma and lobular cancer.
In order to diagnose the body in the traditional categorization of the BC, clinicians must combine feedback from medical equipment with their own expertise, which is sometimes arbitrary and ineffective. In addition, issues like missed diagnoses and misdiagnoses are more likely to happen due to the rising frequency of BC and the lack of available medical services.
Classification based on differentiation of tumor
Despite the clinical significance of BC staging, the histomorphological categorization is the foundation for all other classification schemes and is crucial for BC diagnosis. The performance and knowledge of pathologists are heavily relied upon in this categorization approach, with minimal contribution from molecular testing. Differentiating between in situ and invasive illness, grading and classifying tumors, and separating primary breast cancers from their mimics are just a few of the daily challenges. Without the histological confirmation of BC and the accuracy of the diagnosis, no staging or molecular categorization method is useful.
The evaluation of specific features, both individually and collectively, such as the cytological and architectural characteristics of the proliferating cells, tumour-associated stroma, and the demonstration of the presence or absence of myoepithelial cells at the epithelial stroma interface using H&E-stained slides, supported by the use of IHC and other molecular assays in certain situations, is the basis for the histological diagnosis of BC. The evaluation of tumour differentiation comes after the confirmation of invasive BC of primary breast origin. The grade and type of tumour histology can be used to morphologically quantify differentiation in BC. While tumour type shows the kind of differentiation, histological grade, which assesses how comparable a tumour is to the normal breast terminal ductlobular units, 20 reflects the degree of differentiation.