The role of point of care ultrasonography
Received: 24-Oct-2017 Accepted Date: Nov 20, 2017; Published: 28-Nov-2017
Citation: Peguero A, Lamarche J, Courville C, et al.. The role of point of care ultrasonography. Clin Nephrol Res. 2017;1(1):12-16.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
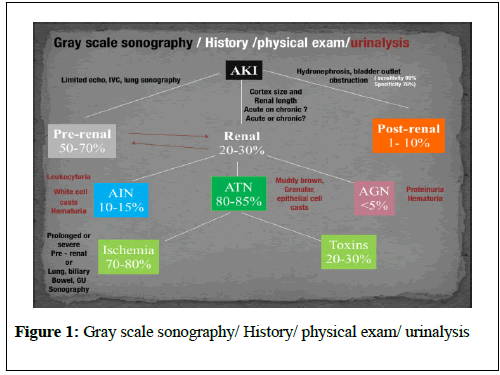
The evaluation of renal failure often starts with the classical pre-renal, renal and post renal causalities delineating a practical workable approach in its differential diagnosis. Accordingly the history, physical exam, urinalysis and kidney-bladder sonography are standard resources in the initial approach of renal diseases. Indeed, ultrasonography have very well established role as an important adjuvant for post renal diagnosis of renal failure. Nevertheless, in the clinical setting most of the causes of kidney failure are pre-renal and renal. In addition some renal causes of kidney failure are manifestations of systemic diseases in which sonography can be diagnostically analogous to the history and physical examination. In this paper we explore the point of care (POC) sonographic contributory signs in the evaluation and management of renal failure extending beyond the traditional kidney biopsy, placement of central lines or screening of hydronephrosis.
Introduction
Two main important elements may possible in our nephrological practice to incorporate POC sonography [1,2]. First, the development of handheld reliable and portable ultrasounds and second its derived capacity to obtain objective signs of the extracellular volume status. The latter clinical application is realized through the Incorporation of POC protocols of the modified Focus Assessment Sonography for Trauma (FAST) exam in conjunction with limited echocardiography and lung sonography (Figure 1).
The detection of changes of the extracellular volume is cardinal in the diagnosis and management of renal diseases. The evaluation of lung water by POC ultrasonography in ESRD is emerging as a promising tool. In a recent study among patients with moderate to severe detection of alveolar water 71% were asymptomatic. Two years of follow up of these patients were associated with 3 to 4 times risk of heart attack and death respectively [3-5].
Acute renal failure
Pre-renal
The physical exam indirect evaluation of the renal blood flow as surrogate of effective arterial circulatory flow (EACF) is clinically useful in the evaluation of pre-renal azotemia. The utility is more obvious in the extremes of EACF. However, in the case of less than 5-10% of blood volume losses or physiologic equivalent, heart rate, blood pressure, skin turgor, urinary output and capillary refill maybe within normal limits. These parameters derived from the physical exam are relative late manifestations following endocrine-neurohormonal activation after sensed by arterial baroreceptors [6-9]. Therefore, is understandable why prerenal renal failure is frequently diagnosed retrospectively after correction of the EACF through use of crystalloids, blood products, vasopressors, inotropic agents, discontinuation of agents or treatment of its causes.
We found ultrasonographic signs for acute renal failure at bedside useful in the majority of the patients either as negative or positive findings to rule out prerenal causes:
• Pre renal ultrasonographic signs
• Pre-renal azotemia- dehydration-bleeding
Inferior vena cava luminal diameter and inspiratory collapsibility ultrasonographic image is a surrogate marker of preload venous return and right side heart function. Is been shown to be more accurate than jugular venous distension on physical exam, but only modestly helpful as a surrogate for central venous pressure (CVP) with more accuracy the lower the CVP [10]. However, can be repeated frequently after volume resuscitation to achieve 1.5-2.5 cm diameter dimension and less than 25% inspiratory collapsibility as a goal. Beyond 2.5 cm is more likely that hypovolemia secondary to heart failure is present with the caveat that pulmonary hypertension may induce false positives [11,12]. Hepatic vein dilation is another sign of congestion in the latter scenario. Furthermore, ultrasonography in the evaluation and management of the inferior vena cava syndrome in the pregnancy and intra-abdominal compartment seems to have a solid evidence for further clinical testing [13].
Sonographic image of left ventricle either as parasternal long axis or subxiphoid approach can identify supra-normal left ventricular ejection fraction (LVEF) or hyper dynamic heart as an important clue of the absolute or relative decrease of EACF. Conversely, a decrease in EACF in patients with low LVEF can be qualitatively assess at bedside in patients with systolic heart failure [14]. Supporting evidence of prerenal azotemia as the result of heart failure can be suggested by the presence of pleural effusions and bilateral comet rockets or B lines in lung sonography [15]. The easily recognizable hypoechoic ascitic fluid in the presence of small, hyperechoic , gross changes in the echo texture of liver may indicated a hepatorenal component as the cause of pre renal failure.
An small increase of less than 20% in the diameter of the portal vein with deep inspiration indicates portal hypertension with a sensitivity of 80% and specificity of 100%. In the critically ill patient with acute kidney injury and arterial hypotension ultrasonographic signs can identified the cause as cardiac tamponade, tension pneumothorax, right ventricular dysfunction (as a surrogate of pulmonary embolism), or an acute coronary event [16-18]. Likewise in the sepsis syndrome with acute kidney injury rapid exploration of the biliary tree, presence of anterior wall thickening, and stone/sludge, common bile duct dilation with peri-gallbladder inflammation suggest acute cholecystitis or cholangitis as the cause. The presence of dyspnea in association with hypotension and hemithorax signs of increase comet tails or consolidation suggest pneumonia. Quick differentiation between ARDS and pulmonary edema from heart failure is possible with ultrasonography. When pleural lines abnormalities are seen ARDS is favored. This will be key in management as it will avoid the use of excessive diuretics in ARDS [19]. In trauma patients the ultrasound exam will identify free fluid (bleeding) as the source of the prerenal failure and frequently the cause of the lesions (aneurysm, liver or spleen, ectopic pregnancy) will be revealed. Sonographic free air view in the abdomen can provide the clue of perforated viscus [20,21]. The ultrasonographic image of inflamed pancreas can aim to pancreatitis as the cause of the systemic inflammatory hypotensive condition. Intravascular losses in the hypoechoic edematous bowel wall in obstruction, ileus, pseudomembranous, infectious or autoimmune entero colitis can induce significant decreases in the extracellular volume and pre renal failure.
In this category belongs acute tubular necrosis, glomerulonephritis and interstitial nephritis. More often than not there is no specific signs to identify the causes. Nevertheless, poor corticomedullary differentiation, kidney size less than 9 cm and cortex size less than 1 cm help to classified in chronic versus acute renal failure, especially if no previous serum creatinine values are available. The early diagnosis of acute tubular necrosis( ATN) continue to be a clinically relevant situation for management of acute renal failure. Despite not currently a practical tool for POC the use of bed side Doppler repetitive renal vasculature measures of resistive index predict occurrence and severity of ATN in the critical care setting and is an independent risk factor for poor survival in arterial hypertension and heart failure. A role in hepatorenal syndrome was explore recently. The incorporation to the point of care of this promising tool is yet undefined [22-27].
The additional ultrasonographic sign of sinusitis in the context of nephritic sediment and rapid progression of creatinine values suggest ANCA related vasculitis. Likewise, nephritic sediment and bilateral sonographic lung interstitial fluid in the absence of infection or normal POC echocardiogram without significant edema elsewhere in younger adults suggest glomerulonephritis in the category of pulmonary lung syndrome as anti glomerular basement membrane. In the elderly suggest ANCA vasculitis. Pleural effusion, synovitis, proteinuria and/or hematuria will aim to lupus nephritis. The diagnostic validity of ultrasonography is well established in the ADPKD. The bedside visualization of a parathyroid adenoma may be an important clue for a patient with CKD echogenic kidneys, nephrolithiasis with or without hypercalcemia to diagnosed primary hyperparathyroidism. The radiologist ultra sonographic performance compared to parathyroid surgical exploration have a sensitivity, specificity, and positive predictive value of sonography for identifying abnormal parathyroid glands of 74%, 96%, and 90%, respectively [28].
In the absolute or relative severe hypertensive patient with headaches ultrasonography at bedside can provide a valuable diagnostic and risk assessment information of increase endocranial hypertension measuring optic nerve sheath. Sensitivity and specificity of papilledema was 90% and 79% respectively when 3.3 mm was the cutoff of the nerve sheath with a 30 degrees sign [29]. The recognition of severe left ventricular hypertrophy in POC ultrasonography in a patient with normal or low normal blood pressure may alert to the diagnosis of normotensive renal failure with renal hypoperfusion in a patient with previously unrecognized severe hypertension. In the same context but sepsis may be prudent to keep the MAP higher than usual with pressors to decrease renal failure and dialysis needs in the critical care setting [30-33].
The sonographic carotid medial intimal index dimension correlate with atherogenesis, LVH and cognition, in the context of arterial hypertension and/or CKD increase to more than 1.1 mm is the harbinger of cardiovascular mortality arguably prompting consideration for early initiation of antihypertensive medications [31,33,34]. The size and contour (smooth or irregular) of kidneys may provide clues to reflux nephropathy, dysplastic kidneys, radiation nephritis or chronic pyelonephritis. The presence of nephrotic syndrome and abnormal free light chains ratio, bedside echo showing the typical refractile myocardial walls with a peculiar speckled pattern is strongly suggestive of amyloidosis [35]. The initial imaging of choice in nephrocalcinosis and specially the medullary type is ultrasonography, preferred to x ray and perhaps CAT scan. Conditions associated with chronic hypercalcemia, medullary sponge kidney, milk alkali syndrome, sarcoidosis, distal Renal tubular acidosis are causes of nephrocalcinosis. Some degree of Chronic kidney disease is a constant in nephrocalcinosis [36].
In rhabdomyolysis with acute renal failure the there is a non-specific hypo echogenic muscle and enlargement of the muscle volume. The sensitivity is low and the role in this clinical context is undefined [37-39]. Another important cause of acute renal failure in the critical care setting is intraabdominal compartment syndrome. Here, the bladder pressure measurement protocols are the standard of care. A human model evaluate the predictive value of intra-abdominal compartment syndrome pressures using the Inferior vena cava (IVC) square surface. In this study normalized surface area of the IVC of more than 1 cm2/m2 was able to exclude the presence of intra-abdominal hypertension 87.5%, however, the sensitivity of detection of the intrabdominal hypertension was only 67.5% when IVC was less than 1 cm2/m2 [40].
In peritoneal dialysis with exit site infection the presence of more than one millimeter radiolucent rim around the exit cuff catheter after antibiotics have a bad prognosis and suggest catheter removal. This sonographic sign has a positive and negative predictive value for exit site infection of 84.6 and 94.1 percent respectively [41,42]. Another risk factor for peritonitis in peritoneal dialysis is air in the peritoneum which can be seen in a third of the patients. The latter category of individuals have 2.4 times more risk of peritonitis as compare to the non-pneumoperitoneum patients. The sensitivity and specificity of ultrasonographic detection of pneumoperitoneum is 94% and 100% respectively using the scissor technique [43,44]. Has been suggested that proper training should avoid pneumoperitoneum on these patients.
Is possible but not yet tested that patient education and change in procedure may decrease incidence of pneumoperitoneum and peritonitis. The use of pre laparoscopic ultrasonography in the insertion of peritoneal dialysis catheter in the diagnosis patient of adhesions ( visceral slide sign) have a sensitivity of 90-92 percent. There is a need of further studies in the sensitivity and specificity of ultrasonography in this area.
History and physical is frequently helpful in the diagnosis of malfunction arteriovenous fistulas for inflow or outflow disturbances with sensitivity ranging 70-100% and specificity 71-93% as compare with angiography. POC limited ultrasound can be frequently helpful in a problematic arteriovenous fistula, either for cannulation or diagnosis. The congruence of duplex sonography with arteriogram is 85-96%. In addition diagnostic accuracy of a dysfunctional fistula causes (pseudo or true aneurysm, poor development, stenosis, thrombi or accessory veins) can be observed in the dialysis units through limited sonography [45-48]. After placement of dialysis catheter using real time ultrasonography pneumohemothorax can be reliably and rapidly diagnosed. Misplacement of catheter outside of the right atrium was detected by thoracic echocardiogram with a sensitivity of 96%, a specificity of 83% and a positive predictive value of 98% [49,50]. Taking altogether, ultrasonography seems to be able to replace chest x ray in the large majority of the cases after central vein dialysis catheters placement in the critical care setting.
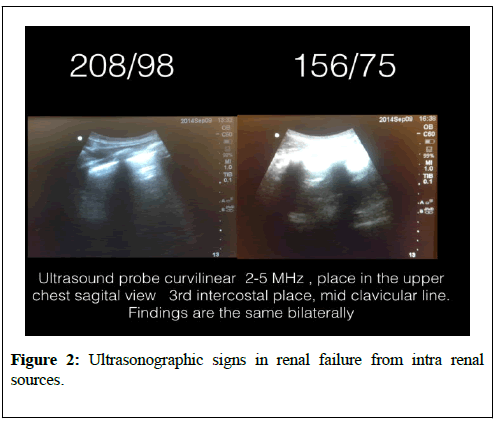
In a patient with ESRD with severe hypertension, worsening dyspnea after fluid removal on dialysis and negative auscultation of the lungs at physical exam we demonstrated a ultrasonographic lung fluid with remarkable improvement in symptoms only after blood pressure control. Reverberation horizontal artifacts (normal) beneath the pleura are replaced by laser rays or rocket tails in the presence of pulmonary edema. See Figure 2, before and after blood pressure control changes in the lungs. In post kidney biopsy bedside ultrasonography may explained elevations of creatinine, decreases in hemoglobin or arterial hypertension by detecting arteriovenous fistula, hematoma or page kidneys. Color flow utrasonography can also be used to avoid hitting vessels prior to biopsy an to predict early discharge documenting lack of hematoma shortly after kidney biopsy [51,52].
Ultrasonographic signs in post renal failure
The ultrasonographic sensitivity to detect dilation to hydronephrosis of pelvico calyceal system is well established. Is the method of choice in pregnancy and initial screening test for the non-pregnant. CAT scan in nephroureterolithiasis is the preferred imaging studies, however, due to radioinizing issues and cost ultrasonography is gaining popularity for initial and/or follows up evaluation. The ureteral jet is a relatively unexplored color and Doppler sonographic methodology that can provide insight of the pelvico-calyceal peristalsis garnishing evidence of functional obstruction [53-58]. Post void bladder residual, bladder wall hypertrophy may provide important clues as the cause of the obstructive uropathy.
Telenephrology and ultrasonography
We found that evaluation of IVC, lung and focus kidney sonography is helpful POC telemedicine with the probe handle by nurses at a distance. See Figures 3-6 within clinico video teleconferencing.
Cardiac arrest in ESRD
Patients on End Stage Renal Disease have sudden cardiac arrest of several etiologies. During the Advance cardiac life support events after the two minutes of cardio pulmonary resuscitation there is a brief period of evaluation of electrical rhythm in which echocardiography can be helpful in the diagnosis. Enlarge right ventricular (>2/3) of the left ventricle may provide the clues for pulmonary embolism. (see below picture few seconds after CPR with pulse). Bedside sonography have the potential of alter the current recommendation of CPR management. Pulse less electrical activity is more common in ESRD, the presence of hyper contractile myocardium in absence of pulse would suggest the need of fluids or blood instead of the usual epinephrine and CPR (Figure 7).
Conclusion
Point of care ultrasonography provides an important and continuously expanding tool to improve nephrological diagnostic accuracy in concert with history and physical exam. Acute kidney injury categorization continues to be a challenging issue both in the treatment and diagnosis. Extracellular fluid evaluation is paramount in all kidney diseases conditions. Recent clinical studies in lung ultrasonography suggest that the learning curve to the medical provider is quicker than other organs. Discriminatory signs of pneumonia, cardiogenic versus non cardiogenic pulmonary edema in POC sonography in association with limited bedside echocardiography maybe important as cost effective strategies in the management of dyspnea. Incorporation to clinical practice will require that medical schools, residency and nephrology fellowship programs designed teaching strategies in the curriculum. Research studies with hard outcomes in regard to diagnosis, morbidity and mortality are necessary in these areas.
REFERENCES
- Remer EM, Papanicolaou N, Casalino DD, et al. ACR Appropriateness Criteria(®) on renal failure. Am J Med. 2014;127:1041-8.e1.
- Rumack C, Wilson S, Charboneau JW, et al. The kidney and urinary tract. Diagnostic ultrasound 4 ed. 2011;chapter 9.
- Mallamaci F, Benedetto FA, Tripepi R, et al. Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging. 2010;3:586-94.
- Enia G, Torino C, Panuccio V, et al. Asymptomatic pulmonary congestion and physical functioning in hemodialysis patients. Clin J Am Soc Nephrol. 2013;8:1343-8.
- Zoccali C, Torino C, Tripepi R, et al. Pulmonary congestion predicts cardiac events and mortality in ESRD. J Am Soc Nephrol. 2013;24:639-46.
- Fortes MB, Owen JA, Raymond-Barker P, et al. Is this Elderly Patient Dehydrated? Diagnostic Accuracy of Hydration Assessment Using Physical Signs, Urine, and Saliva Markers. J Am Med Dir Assoc. 2015;16:221-8.
- Jauregui J, Nelson D, Choo E, et al. The BUDDY (Bedside Ultrasound to Detect Dehydration in Youth) study. Crit Ultrasound J. 2014;6:15.
- McGee S, Abernethy WB 3rd, Simel DL. The rational clinical examination. Is this patient hypovolemic? JAMA. 1999;281:1022-9.
- Chung HM, Kluge R, Schrier RW, et al. Clinical assessment of extracellular fluid volume in hyponatremia. Am J Med. 1987;83:905-8.
- Guarracino F, Ferro B, Forfori F, et al. Jugular vein distensibility predicts fluid responsiveness in septic patients. Crit Care. 2014;18:647.
- Stawicki SP, Adkins EJ, Eiferman DS, et al. Prospective evaluation of intravascular volume status in critically ill patients: does inferior vena cava collapsibility correlate with central venous pressure? J Trauma Acute Care Surg. 2014;76:956-63.
- Thanakitcharu P, Charoenwut M, Siriwiwatanakul N. Inferior vena cava diameter and collapsibility index: a practical non-invasive evaluation of intravascular fluid volume in critically-ill patients. J Med Assoc Thai. 2013;96:S14-22.
- Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care. 2014;4:1.
- Fields JM, Catallo K, Au AK, et al. Resuscitation of the pregnant patient: What is the effect of patient positioning on inferior vena cava diameter? Resuscitation. 2013;84:304-8.
- Gustafsson M, Alehagen U, Johansson P. Pockwwet-sized ultrasound examination of fluid imbalance in patients with heart failure: A pilot and feasibility study of heart failure nurses without prior experience of ultrasonography. Eur J Cardiovasc Nurs. 2015;14:294-302.
- Bolondi L, Mazziotti A, Arienti V, et al. Ultrasonographic study of portal venous system in portal hypertension and after portosystemic shunt operations.Surgery. 1984;95:261-9.
- Al-Nakshabandi NA. The role of ultrasonography in portal hypertension. Saudi J Gastroenterol 2006;12:111-117.
- Peguero et al. # SCU16: Lung Ultrasound for the Renal Doctor. National Kidney Foundation Meeting. 2016.
- Copetti R, Soldati G, Copetti P. Chest Sonography; A useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovascular Ultrasound. 2008;6:16.
- ProCESS Investigators, Yealy DM, Kellum JA, et al. A Randomized Trial of Protocol-Based Care for Early Septic Shock. N Engl J Med. 2014;370:1683-93.
- Hefny AF, Abu-Zidan FM. Sonographic diagnosis of intraperitoneal free air. J Emerg Trauma Shock. 2011;4:511-13.
- Meola M, Petrucci I. Ultrasound and color Doppler in nephrology. Acute kidney injury. G Ital Nefrol. 2012;29:599-615.
- Corradi F, Brusasco C, Vezzani A, et al. Hemorrhagic shock in polytrauma patients: early detection with renal Doppler resistive index measurements. Radiology. 2011;260:112-8.
- Viazzi F, Leoncini G, Derchi LE, et al. Ultrasound Doppler renal resistive index: a useful tool for the management of the hypertensive patient. J Hypertens. 2014; 32:149-53.
- Marty P, Szatjnic S, Ferre F, et al. Doppler renal resistive index for early detection of acute kidney injury after major orthopaedic surgery. Eur J Anaesthesiol. 2015;32:37-43.
- Kastelan S, Ljubicic N, Kastelan Z, et al. The role of duplex-doppler ultrasonography in the diagnosis of renal dysfunction and hepatorenal syndrome in patients with liver cirrhosis. 2004;51:1408–1412.
- Capotondo L, Nicolai GA, Garosi G. The role of color Doppler in acute kidney injury. Arch Ital Urol Androl. 2010;82:275-9.
- Tublin ME, Pryma DA, Yim JH, et al. Localization of parathyroid adenomas by sonography and technetium tc 99m sestamibi single-photon emission computed tomography before minimally invasive parathyroidectomy: are both studies really needed? J Ultrasound Med. 2009;28:183-90.
- Carter SB, Pistilli M, Livingston KG, et al. The role of orbital ultrasonography in distinguishing papilledema from pseudopapilledema. Eye (Lond). 2014;28:1425-30.
- Abuelo JG. Normotensive ischemic acute renal failure. N Engl J Med. 2007;357:797-805.
- Messerli FH. Clinical determinants and consequences of left ventricular hypertrophy. Am J Med. 1983;75:51-6.
- Chen SC, Su HM, Hung CC, et al. Echocardiographic parameters are independently associated with rate of renal function decline and progression to dialysis in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:2750-8.
- Helfand M, Buckley DI, Freeman M, et al. Emerging risk factors for coronary heart disease: a summary of systematic reviews conducted for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151:496–507.
- Greenland P, Alpert JS, Beller GA, et al.2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults. J Am Coll Cardiol. 2010;56:e50-103.
- Huang Y, Zhan J, Wei X, et al. Clinical characteristics of 42 patients with cardiac amyloidosis. Zhonghua Nei Ke Za Zhi. 2014;53:546-9.
- Boyce AM, Shawker TH, Hill SC, et al. Ultrasound is superior to computed tomography for assessment of medullary nephrocalcinosis in hypoparathyroidism. J Clin Endocrinol Metab. 2013;98:989-94.
- Su BH, Qiu L, Fu P, et al. Ultrasonic appearance of rhabdomyolysis in patients with crush injury in the Wenchuan earthquake. Chin Med J (Engl). 2009;122:1872-6.
- Steeds RP, Alexander PJ, Muthusamy R, et al. Sonography in the diagnosis of rhabdomyolysis. J Clin Ultrasound. 1999;27:531-3.
- Lamminen AE, Hekali PE, Tiula E, et al. Acute rhabdomyolysis: evaluation with magnetic resonance imaging compared with computed tomography and ultrasonography. Br J Radiol. 1989;62:326-30.
- Cavaliere F, Cina A, Biasucci D, et al. Sonographic assessment of abdominal vein dimensional and hemodynamic changes induced in human volunteers by a model of abdominal hypertension. Crit Care Med. 2011;39:344-8.
- Kwan TH, Tong MK, Siu YP, et al. Ultrasonography in the management of exit site infections in peritoneal dialysis patients.Nephrology (Carlton). 2004;9:348-52.
- Karahan OI, Taskapan H, Yikilmaz A, et al. Ultrasound evaluation of peritoneal catheter tunnel in catheter related infections in CAPD. Int Urol Nephrol. 2005;37:363-6.
- Karahan OI, Kurt A, Yikilmaz A, et al. New method for the detection of intraperitoneal free air by sonography: scissors maneuver.J Clin Ultrasound. 2004;32:381-5.
- Okamoto T, Ikenoue T, Matsui K, et al. Free air on CT and the risk of peritonitis in peritoneal dialysis patients: a retrospective study. Ren Fail. 2014;36:1492-6.
- Arshad FH, Sutijono D, Moore CL. Emergency Ultrasound Diagnosis of a Pseudoaneurysm Associated With an Arteriovenous Fistula ACAD Emerg Med. 2010;17:e43-5.
- Teodorescu V, Gustavson S, Schanzer H. Duplex Ultrasound Evaluation of Hemodialysis Access: A Detailed Protocol. Int J Nephrol. 2012;2012:7.
- Coentrão L, Turmel-Rodrigues L. Monitoring dialysis arteriovenous fistulae: it’s in our hands. J Vasc Access 2013;14:209-215.
- Chandra AP, Dimascio D, Gruenewald S, et al. Colour duplex ultrasound accurately identifies focal stenoses in dysfunctional autogenous arteriovenous fistulae. Nephrology (Carlton). 2010;15:300-6.
- Bedel J, Vallée F, Mari A, et al. Guidewire localization by transthoracic echocardiography during central venous catheter insertion: a periprocedural method to evaluate catheter placement. Intensive Care Med. 2013;39:1932-7.
- Vezzani A, Brusasco C, Palermo S, et al. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med. 2010;38:533-8.
- Granata A, Floccari F, Ferrantelli A, et al. Does Systematic Preliminar Colour Doppler Study Reduce Kidney Biopsy Complication Incidence? Int J Nephrol. 2011;2011:419093.
- European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J. Hypertens. 2003;21:1011–53.
- Celik S, Altay C, Bozkurt O, et al. Association Between Ureteral Jet Dynamics and Nonobstructive Kidney Stones: A Prospective-controlled Study. Urology. 2014;84:1016-20.
- Tullus K. Does the ureteric jet Doppler waveform have a role in detecting vesicoureteric reflux? Pediatr Nephrol. 2013;28:1719-21.
- Jandaghi AB, Falahatkar S, Alizadeh A, et al. Assessment of ureterovesical jet dynamics in obstructed ureter by urinary stone with color Doppler and duplex Doppler examinations. Urolithiasis. 2013;41:159-63.
- Pepe P, Motta L, Pennisi M, et al. Functional evaluation of the urinary tract by color-Doppler ultrasonography (CDU) in 100 patients with renal colic. Eur J Radiol. 2005;53:131-5.
- Leung VY, Metreweli C. Ureteric jet in renal transplantation patient. Ultrasound Med Biol. 2002;28:885-8.
- Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685-713.