The social and health gender differences in patients companion in the family medicine consultation
Keywords
Companions; Gender differences; Family Practice; Family Members; Caregivers; Visit to Doctor’s Office
Introduction
All over the world women are the predominant providers of informal care for family members with chronic medical conditions or disabilities, including the elderly and adults with mental illnesses. It has been suggested that there are several societal and cultural demands on women to adopt the role of a family-caregiver [1]. So, spouses often serve as the primary caregivers to their ill or disabled partners [2].
The domain of health includes the entire range of issues which touch on illness, sickness, disease, wellness, as well as those activities of preventing, diagnosing, healing, caring and curing. Thus, questions about women’s participation in this domain profound and immediate concern to women, and involve roles and selves. Women have domestic activities which sustain, literally and symbolically, the way of life. As the providers of health, women are responsible for securing the domestic conditions necessary for the maintenance of health and for recovery from sickness. Women also serve as mediators of outside services. Their responsibilities with the domestic health service unavoidably bring them into contact with professional health service, among them the family doctor [3].
In practice, a third person (companion) frequently accompanies a patient during medical encounter. There is a high prevalence of the presence of a companion, who is in almost one of every 4 visits served in Family Medicine. Companions of the patients in the medical office are usually family members in near 100% of cases [4-9].
The major results of existing studies suggest that the regular presences of companions of the patients in consultations are often perceived as helpful. Accompaniment to medical visits is associated with better self-care maintenance and management, and this effect may be mediated through satisfaction with provider communication [10]. Also, companions provide company, emotional support, and they have a role in mobility and decision making of the patients [11,12]. However, their participation often poses challenges [13].
Despite all the above, the reports, reviews or investigations about the gender differences in patient’s companion are rather scarce in our environment. Very little research has examined the influence of the gender in companions who accompany patients on everyday visits to the doctor [5,14,15].
In this context, we present a study whose objectives were to describe gender differences in patient’s companion, and their social and health characteristics, in family medicine consultations.
Methods
An observational, descriptive, prospective study, which included patients of both sexes over 14 years of a family medicine office which has a quota of 2,000 patients, was carried out. The study was performed within a larger one about patient’s companion already published [8]. A random sample was chosen. Comparing retrospectively the percentages obtained from companion’s female (63%) and male (37%), assuming a confidence level of 90%, a power of 80%, and a male / female ratio of 0.5, it would be needed a sample of 67 companions female and 34 companions male [16].
From randomly chosen day for 15 consecutive days, from 26 November 2015 to 18 December 2015, the visited patients were included, and data from the companions with patients were collected. Companion was defined as any person who accompanied the patient in the consulting room or that consult instead the patient. Patients were included only one time. Thus, were excluded the repeated consultations of same patient, including only the first visit. If the patient had two companions only was included the data from the first of them in analysis.
For each patient and companion the following variables were collected: age, sex, chronic disease (defined as “any alteration or deviation from normal that have one or more of the following characteristics: is permanent, leaves residual impairment, is caused by a non-reversible pathological alteration, it requires special training of the patient for rehabilitation, and/or can be expected to require a long period of control, observation or treatment”) [17], and classified according to International Classification of Diseases (ICD-10) [18], taking medication, collecting the therapeutic drugs group, classified according to ATC code or system Anatomic Classification, Therapeutic, Chemical [19], sick leave of the patient, the problems in the family context (based on the genogram, and valued by the same family doctor who performed the genogram at the past time, by viewing the family scheme (the genogram was a schematic model of the structure and processes of a family, included the family structure, life cycle when that family is, the important life events, family resources, and family relational patterns) [20-22], social-occupancy class, according to the Registrar General’s classification of occupations and social status code [23,24], if the analytical or imaging test was requested for the patient, if the patient needs a consultation with the specialist, the companion relationship with the patient, and the social availability of companion in relation to the patient.
A Microsoft Excel® file was built, and the IBM SPSS Statistics for Windows, Version 18.0. Armonk, NY: IBM Corp software was used. Descriptive data, which were expressed by standard measures of central tendency and dispersion, were obtained. The bivariate comparisons were performed using the test of chi-square, with Yates correction when it was pertinent, for the percentages, the Student t test for the mean, exact probability Fischer, and the Mann-Whitney test for comparing means in variables with nonparametric distribution. The informed consent of all patients or their guardians for using of data in research was obtained.
Results
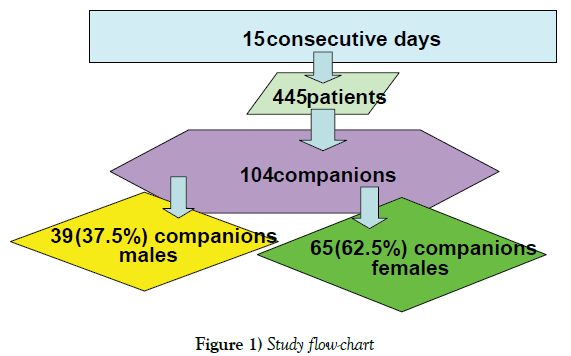
During the 15 days of data collection, a sample of 445 patients was obtained, of whom 104 were companions who accompanied to the patient in the office. 65 (62.5%) were female, and 39 (37.5%) male (Figure 1).
Results of the companions
In the female companions with regard to the male companions: there were 69% in the group of 40-64 years old vs. 49% (p = 0.02); were wife (34%), daughters (33%), and mothers (25%) vs. husband (56%), father (23%), and son (18%) (p=0.001); were unskilled workers in the 68% vs. el 43% (p=0.036); were workers in the 44%, housewife in the 40%, retired in the 8%, and unemployed in the 3% vs. workers 24%, retired in the 49%, and unemployed 19% (p=0.036); had more diseases of the musculoskeletal system and connective tissue (44% vs. 21% in male companions; p=0.024), and they were taking more medications of the musculoskeletal system (26.2% vs. 5.4% in male companions; p=0.014) (Table 1).
| Studied variables | Companion male (n=39) |
Companion female (n=65) |
Statistical significance |
|---|---|---|---|
| Age in years of companions | (n=39) | (n=62) | t=1.496 (p=0.138) |
| 54.54 ± 15.62 | 50.18 ± 13.35 | X2=8.173 | |
| < 40 years: 17.9% | < 40 years:20% | (p=0.02) | |
| 40-64 years: 48.7% | 40-64 years: 69.2% | ||
| = 65 years: 33.3% | = 65 years: 10.8% | ||
| The companion relationship with the patient | (n=39) | (n=64) | p=0.001 |
| Father: 23.1% | Mother: 25% | ||
| Brother: 2.6% | Brother: 0 | ||
| Another familiar: 0 | Another familiar: 4.7% | ||
| Friend: 0 | Friend: 1.6% | ||
| Son: 17.9% | Son: 32.8% | ||
| No family member: 0 | No family member: 1.6% | ||
| Husband 56.4% | Wife: 34.4% | ||
| Chronic disease in companions | (n=37) 1.97 ± 1.50 |
(n=61) 0 |
N.S. |
| Diseases of the musculoskeletal system and connective tissue* | 21.1% / 0.21 ± 0.41 | 43.6% / 0.54 ± 0.68 | p=0.024 (X2) / p=0.012 (U) |
| Medications taken by the companion of the Musculoskeletal system* | 5.4% / 0.05 ± 0.22 | 26.2% / 0.30 ± 0.52 | p=0.014 (X2) / p=0.012(U) |
| Potential problems familiar context of the companion based on the genogram | (n=37) 62.2% (44.75-77.54) |
(n=60) 38.3% (26.07-51.78) |
p=0.36 (X2) |
| Social-occupancy class of companions | (n=35) | (n=59) | p=0.036 (X2). |
| Higher managerial | 0 | 0 |
|
| - Intermediate occupations | 0 | 5.10% | |
| -Specialized whitecollar workers | 5.70% | 3.40% | |
| -Specialized worker’s manuals | 14.30% | 5.10% | |
| -Semiskilled workers | 34.30% | 13.60% | |
| -Unskilled workers | 42.90% | 67.80% | |
| -Students | 2.90% | 5.1% | |
| The social availability of companion in relation to the patient. | (n=37) | (n=63) | P<0.001 (X2) |
| Workers: 24.3% | Workers: 44.4% | ||
| Retired: 48.6% | Retired: 7.9% | ||
| Students: 2.7% | Students: 4.8% | ||
| Housewife: 5.4% | Housewife: 39.7% | ||
| Unemployed: 18.9% | Unemployed: 3.2% |
*In Chronic diseases and Medications taken only statistically significant comparisons are shown
Table 1:Comparisons of the companion female and companion male.
Results of the accompanying patients
Regarding patients accompanied by women, the 52% were male (vs. only 21% of patient’s males who were accompanied by male; p=0.003), and they were unskilled workers in the 53%, and students in the 16% (vs. 64% y 8% respectively in patients accompanied by male; p<0.001) (Table 2).
| Studied variables | Companion male (n=39) |
Companion female (n=62) |
Statistical significance |
|---|---|---|---|
| Age in years of patients | 54.53 ± 20.62 | 52.84 ± 23.64 | t=0.364 (p=0.717) (p=0.735) X2=0.56 |
| (n=38) | (n=63) | ||
| < 40 años 26.3% | < 40 años 32.8% | ||
| 40-64 años 31.6% | (n=64) | ||
| ≥ 65 años 42.1% | 40-64 años 31.3% | ||
| ≥ 65 años 35.9% | |||
| Sex of patients | (n=38) | (n=64) | p=0.003 |
| Males 21.05% (9.55-37.31) |
Males 51.56% (38.72-64.25) |
||
| Women 78.94% (62.68-90.44) |
Women 48.43% (35.75-61.27) |
||
| Number of Chronic diseases in patients | 2.55 ± 1.70 (n=38) |
2.23 ± 1.38 | N.S. |
| Diseases of the ear and mastoid process in patients* | 10.5% / 0.13 ±0.41 |
0 | p=0.017 (PeF) / p=0.017 (U) |
| Number of Medications taken by the patient | 3.16 ± 3.00 | 2.67 ± 2.89 | N.S. |
| Medications taken by the patient of the musculoskeletal system* | 5.3% / 0.05 ± 0.22 | 18.8% / 0.19 ± 0.39 | p=0.075 (X2) / p=0.075 (U) |
| Patients with sick leave | 13.15% (4.41-28.08) |
12.5% (5.55-23.15) |
N.S. |
| Potential problems familiar context of the patient based on the genogram | (n=36) 58.33% (40.75-74.48) |
(n=62) 40.32% (28.05-53.55) |
P=0.097 (χ2) |
| Social-occupancy class of patients | (n=36) | (n=62) | p<0.001 |
| -Higher managerial | 2.80% | 1.60% | |
| -Intermediate occupations | 0 | 0% | |
| -Specialized white-collar workers | 2.80% | 4.80% | |
| -Specialized-workers manuals | 0% | 11.30% | |
| -Semiskilled workers | 22.20% | 12.90% | |
| -Unskilled workers | 63.90% | 53.20% | |
| -Students | 8.30% | 16.30% | |
| Complaint of patient according to ICD-10 | (n=38) | (n=64) | N.S. |
| IX: 21.1% | IX: 17.2% | ||
| XIII: 15.8% | X: 15.6% | ||
| X: 13.2% | XIII: 14.1% | ||
| V y XIV: 10.5% | V: 10.9% | ||
| XI: 9.4% | |||
| Analytical test was requested for the patient | (n=38) 7.89% (1.65-21.37) |
(n=64) 1.56% (0.04-8.40) |
N.S. |
| The patient need a consultation with the specialist | (n=38) 13.15% (4.41-28.08) |
(n=64) 18.75% (10.08-30.46) |
N.S. |
*In Chronic diseases and medications taken only statistically significant comparisons are shown.
Table 2:Comparisons of the patients with companion female and companion male.
Discussion
It has been reported that visits in which one or more family members are present in the medical office are quite common, and their average frequency can be set at around 25% of visits to the doctor [8,9]. It is admitted that companions of the patients are usually family members [4], and predominantly female. Many studies, which have examined gender differences among family-caregivers, have concluded that women spend more time in providing care and carry out personal-care tasks more often than men. This gender bias influences women to assume more substantial caregiving duties [25].
Women are the overwhelming majority of health care providers. Them caring role places them at interface between the family and the state, as the go between linking the informal health-care system with the formal apparatus of the welfare state [3]. There are not one but two systems which determine health beliefs and practices: the lay referral system, which consists in a variable lay culture and a network of personal influences, and the professional referral system of medical culture and institutions. The lay referral system encompasses important features of informal health care. It has a role in the negotiation of health. This concept of referral system serves to highlight the economic contribution which women make in caring for their relatives. The lay accompanying system is located through its cultural and spatial proximity, and in terms of the social relations of gender and generation which underpin family life. We found that 62.5% were women (Figure 1), a figure slightly lower than that reported by Brown (73%) [13], but that study included children, who are usually accompanied by their mothers, whereas in our consultation the patients are attended from the age of 14 years old and greater than 59% reported by other authors [26].
Patient’s companions are typically female and they are part of a systematic informal health care. The provision of accompaniment continues to be organized on an informal individual and unpaid basis within the home. This style of mediation between the public and private domains is well documented in the field of prevention and community caregivers. Becoming a carer involves meeting the needs of those who fall victim to illness and invalidity [3].
We found that the female companions were younger than the male companions (69% in the group of 40-64 years old in female companions vs. 49% in male companions; p = 0.02) (Table 1). This gender gap in care (more caregiving burden among those women in middle age than among those in older age) has been reported (2,13). In our study, were wife (34%), daughters (33%), and mothers (25%) vs. husband (56%), father (23%), and son (18%) (p=0.001), which also broadly coincides with other authors, for whom are the most frequent the mother or wife [6-8].
We also found that female companion of the patient was predominantly worker, and of these, were unskilled workers in the 68% (vs. el 43% in male companion; p=0.036) (Table 1), contrary to published data that women caregivers were less likely to be working [27,28].
Many studies have also found that women and female family caregivers experience greater mental and physical strain, greater caregiver-burden, and higher levels of psychological distress while providing care. However, almost an equal number of studies have not found any differences between men and women on these aspects [1,25,28]. We found that companion female had more diseases of the musculoskeletal system and connective tissue (44% vs. 21% in male companions; p=0.024), and they were taking more medications of the musculoskeletal system (26.2% vs. 5.4% in male companions; p=0.014), but we found no difference in diseases or treatments about mental health (Table 1). Other authors have also noted that women caregivers reported significantly more physically unhealthy days than men, and more physical morbidity (lower physical health scores, poorer physical functioning, and loss of physical strength) [29,30].
The companion assumes the value as intermediary and caregiver. The accompanying person’s role most frequently described is of advocate for the patient [5]. The care of patients “very fragile”, the increasing dependence on their families of elderly patients and/or significant chronic problems, along with the complexity of health services, contributing to the perception that informal caregivers and companions have a role indispensable as “intermediaries between the health system and patient.” Therefore, it is desirable to emphasize the need to discuss further about the fragility of patients with their family companions, which are mainly women, who can be supported and trained to participate in decision-making on tasks for the care of the sick, so that meet the needs of the patient, the doctor and family [31].
This gender bias is particularly marked in the field of women health and child health [3] But, we found that patients accompanied by women were in the 52% male (vs. only 21% of patient’s males who were accompanied by male; p=0.003) (Table 2). So, the gender bias is extending beyond the health of women and children. In this context, two more interventions can be suggested (in addition to education): 1) support interventions for companions of patients should take gender-specific risk factors into account; and 2) this gender bias could be a way to humanize health care.
Patients with greater needs are most often come accompanied, which is positive. Those more likely to have a family member present include patients with a low level of health literacy, patients with chronic diseases, older patients, and women [32,33]. We find that Patients accompanied by women were more frequently male, with fewer ENT diseases, and took more drugs from the musculoskeletal group than male patients (Table 2), which can be globally interpreted as that there was no clinically significant differences between patients according to the gender of her or his companion.
Limitations of our study and future research
The outcomes of impact of gender on companion of the patient may be mediated by several other variables (in addition to those included in this study, such as patient related factors, socio-demographic variables, and effects of kinship status), as culture and ethnicity, but these have not been considered in our research on gender differences [1].
1) We have not studied possible geographical variations (our data refer only to the study area, and it should be prudent to extrapolate them to other geographical areas, which may imply, among other variables, different socio-economic level, beliefs and customs.
2) We have not studied possible gender differences in patient’s companion about information on the health situation and disease in the patient, prevention of anxiety, building of trust, promotes of family dialogue, or aid to decision making.
3) It was not collected the meaning or reason to be present companion.
4) The patients’ perceptions about gender differences of patient’s companion were not collected.
5) The relationships of the gender differences of the patient’s companion with the communication in the consultation have not been studied.
In consequence, future studies could include these topics.
Summary and Conclusion
Patient’s companions are predominantly women, of middle age, wives, mothers and daughters, with poor health, low social class, housewives and workers. Male companions are older, husbands and fathers, with better health than female companions, of middle class, and retirees. Patients accompanied either by women or by men have a similar health status. Patients accompanied by women are males, students, of middle class, vs. patients accompanied by men who are women of low social class. The companion “type” is a middle-aged woman, wife, with poor health, low social class, housewife or worker, who accompanying a patient male or student of middle class.
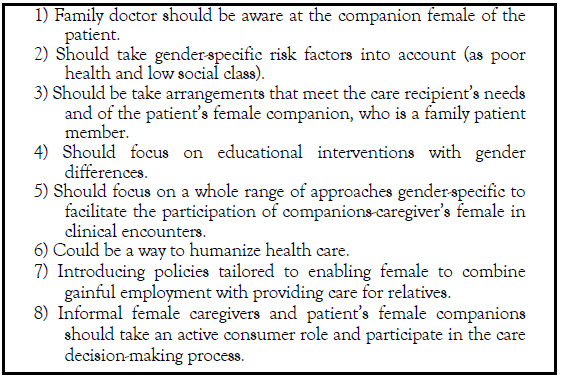
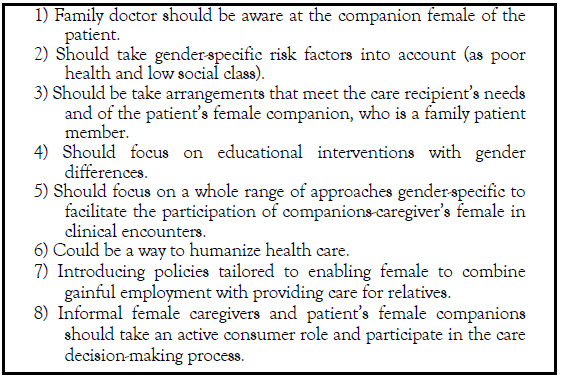
The presence of companion female of patient, usually family members, with the characteristics described above, creates unique opportunities for supporting interventions for this gender bias, which could have better outcomes for the health of family members (patient outcomes as depression, anxiety, relationship satisfaction, disability, and mortality, and family member outcomes as depression, anxiety, relationship satisfaction, and caregiving burden) [28,34,35] (Box 1). Companion seems to play a secondary role, but it can be the main actor [36]. And the gender differences should remind us take into accounts specially the companion female during assistance in individual patients. A female adult, usually the wife, accompanying to the patient in consultation, is always significant and deserves the attention of the doctor. So, it needs a gender oriented practice in relation to patient’s companion [37-47].
References
- Greenland P, Labree L, Azen SP, et al. Coronary artery calcium score combined withframinghamscore for risk prediction in asymptomatic individuals. JAMA 2004;291:210-15.
- Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: A 37-month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation 2003;107:2571-76.
- O’Malley PG, Taylor AJ, Jackson JL, et al.Prognostic value of coronary electron- beam computed tomography for coronary heart disease events in asymptomatic populations. Am J Cardiol 2000;85:945-48.
- Pletcher MJ, Tice JA, Pignone M, et al.Using the coronary artery calcium score to predict coronary heart disease events. Arch Intern Med 2004;164:1285-92.
- Shaw LJ, Raggi P, Schisterman E, et al. Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. Radiology 2003;228:826-33.
- Elias-Smale SE, Proença RV, Koller MT, et al. Coronary calcium score improves classification of coronary heart disease risk in the elderly: The Rotterdam study. J Am CollCardiol 2010;56:1407-14.
- Erbel R, Möhlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: The Heinz Nixdorf Recall study. J Am CollCardiol 2010;56:1397-06.
- Polonsky TS, Mcclelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010;303:1610-16.
- Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol 2010;56:e50-e103.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals : Arandomised placebo- controlled trial. Lancet2002;360:7-22.
- LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. NEJM2005;352:1425-35.
- The long-term intervention with pravastatin in ischaemic disease study group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. NEJM1998;339:1349-57.
- Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. NEJM1996;335:1001-09.
- Scandanavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease:The Scandinavian Simvastatin Survival Study (4S). Lancet1994;344:1383-89.
- Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. NEJM1995;333:1301-07.
- Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels. JAMA1998;279:1615-22.
- Pedersen TR, Faergeman O, Kastelein JJP, et al. High-dose atorvastatin vs. usual-dose simvastatin for secondary prevention after myocardial infarction. JAMA 2005;294:2437-46.
- Nissen SE, Nicholls SJ, Siphani I, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis. JAMA 2006;295:1556-65.
- Nicholls SJ, Ballantyne CM, Barter PJ, et al. Effect of two intensive statin regimens on progression of coronary disease. NEJM 2011;365:2078-87.
- Puri R, Nicholls SJ, Shao M, et al. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am CollCardiol 2015;65:1273-82.
- Yla-Herttuala S, Bentzon JF, Daemen M, et al. Stabilization of atherosclerotic plaques: an update. Eur Heart J 2013;34:3251-58.
- Callister TQ, Raggi P, Cooil B, et al. Effect of HMG-CoA reductase inhibitors on coronary artery disease as assessed by electron-beam computed tomography. NEJM1998;339:1972-78.
- Budoff MJ, Lane KL, Bakhsheshi H, et al. Rates of progression of coronary calcium by electron beam tomography. Am J Cardiol 2000;86:8-11.
- Achenbach S, Ropers D, Pohle K, et al. Influence of lipid-lowering therapy on the progression of coronary artery calcification: Aprospective evaluation. Circulation 2002;106:1077-82.
- Arad Y, Spadaro LA, Roth M, et al. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin c, and vitamin E. J Am CollCardiol 2005;46:166-72.
- Houslay ES, Cowell SJ, Prescott RJ, et al. Progressive coronary calcification despite intensive lipid-lowering treatment: a randomised controlled trial. Heart2006;92:1207-12.
- Terry JG, Carr JJ, Kouba EO, et al. Effect of simvastatin (80 mg) on coronary and abdominal aortic arterial calcium (from the coronary artery calcification treatment with zocor [CATZ] study). Am J Cardiol 2007;99:1714-17.
- Schmermund A, Achenbach S, Budde T, et al. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: A Multicenter, Randomized, Double-Blind Trial. Circulation2006;113:427-37.
- Raggi P, Davidson M, Callister TQ, et al. Aggressive versus moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: beyond endorsed lipid lowering with EBT scanning (BELLES). Circulation 2005;112:563-71.
- Plazak W, Gryga K, Dziedzic H, et al. Influence of atorvastatin on coronary calcifications and myocardial perfusion defects in systemic lupus erythematosus patients: A prospective, randomized, double-masked, placebo-controlled study. Arthritis Res Ther 2011;13:R117.
- Lemos MM, Watanabe R, Carvalho AB, et al. Effect of rosuvastatin and sevelamer on the progression of coronary artery calcification in chronic kidney disease: A pilot study. ClinNephrol 2013;80:1-8.
- Tenenbaum A, Shemesh J, Koren-Morag N, et al. Long-term changes in serum cholesterol level does not influence the progression of coronary calcification. Int J Cardiol2011;150:130-34.
- Goh VK, Lau C-P, Mohlenkamp S, et al.Outcome of coronary plaque burden: A 10-year follow-up of aggressive medical management. Cardiovasc Ultrasound 2010;8:5.
- Anand DV, Lim E, Darko D, et al. Determinants of progression of coronary artery calcification in type 2 diabetes. Role of glycemic control and inflammatory/vascular calcification markers. J Am CollCardiol 2007;50:2218-25.
- Burgstahler C, Reimann A, Beck T, et al. Influence of a lipid-lowering therapy on calcified and noncalcified coronary plaques monitored by multislice detector computed tomography: results of the New Age II Pilot Study. Invest Radiol 2007;42:189-95.
- Mohler ER, Wang H, Medenilla E, et al.Effect of Statin treatment on aortic valve and coronary artery calcification. J Heart Valve Dis 2007;16:378-86.
- Budoff MJ, Yu D, Nasir K, et al. Diabetes and progression of coronary calcium under the influence of statin therapy. Am Heart J 2005;149:695-00.
- Hecht HS, Harman SM. Evaluation by electron beam tomography of changes in calcified coronary plaque in treated and untreated asymptomatic patients and relation to serum lipid levels. Am J Cardiol 2003;91:1131-34.
- Lo J, Lu MT, Ihenachor EJ, et al. Effects of statin therapy on coronary artery plaque volume and high-risk plaque morphology in HIV-infected patients with subclinical atherosclerosis: Arandomised, double-blind, placebo-controlled trial. Lancet HIV 2015;2:e52-e63.
- Zeb I, Li D, Nasir K, et al. Effect of statin treatment on coronary plaque progression - a serial coronary CT angiography study. Atherosclerosis 2013;231:198-04.
- Hoffmann H, Frieler K, Schlattmann P, et al.Influence of statin treatment on coronary atherosclerosis visualized using multi-detector computed tomography. EurRadiol 2010;20:2824-33.
- Inoue K, Motoyama S, Sarai M, et al. Serial coronary CT angiography-verified changes in plaque characteristics as an end point: evaluation of effect of statin intervention. JACC Cardiovasc imaging 2010;3:691-98.
- Auscher S, Heinsen L, Nieman K, et al. Effects of intensive lipid-lowering therapy on coronary plaques composition in patients with acute myocardial infarction: Assessment with serial coronary CT angiography. Atherosclerosis 2015;241:579-87.
- Henein M, Granåsen G, Wiklund U, et al. High dose and long-term statin therapy accelerate coronary artery calcification. Int J Cardiol 2015;184:581-86.
- Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression. JAMA 2004;291:1071-80.
- Puri R, Libby P, Nissen SE, et al. Long-term effects of maximally intensive statin therapy on changes in coronary atheroma composition: Insights from SATURN. Eur Heart J Cardiovasc Imaging 2014;15:380-88.
- Eshtehardi PP, McDaniel MC, Dhawan SS, et al. Effect of intensive atorvastatin therapy on coronary atherosclerosis progression, composition, arterial remodeling, and microvascular function. J Invasive Cardiol 2012;24:522.
Abstract
OBJECTIVES: The purpose of this study is to describe gender differences in patient’s companion, and their characteristics, in family medicine consultations. METHODS: A descriptive and prospective study in a family medicine office (Toledo, Spain) was carried out. For each patient and companion, the following variables were collected: age, gender, chronic illness, chief complaint, medications taken, social class, request for additional tests, kinship, social status and availability of companion. The bivariate comparisons were performed using the test of Chi squared, the Student t test, and the Mann- Whitney test. RESULTS: 104 companions to the patient in the family medicine office were obtained. Of these, 65 (62.5%) were female, and 39 (37.5%) male. In the female companions with regard to the male companions: there were 69% in the group of 40-64 years old vs. 49% (p = 0.02); were wife (34%) vs. husband (56%) (P=0.001); were unskilled workers in the 68% vs. el 43% (p=0.036); were workers in the 44% vs. 24% (p=0.036); had more diseases of the musculoskeletal system and connective tissue (44% vs. 21%; p=0,024) and were taking more medications of the musculoskeletal system (26,2% vs. 5,4% in male companions; p=0.014). CONCLUSION: There is a gender bias in the patient’s companion: she is a middle-aged woman, wife, with poor health, low social class, housewife or worker, accompanying a middle-class patient, male or student. Implicit stereotypes associating to female gender with providers of health continue to express themselves in accompany the sick in the family medicine office. Support interventions for companions of patients should take gender specific risk factors into account
-Keywords
Companions; Gender differences; Family Practice; Family Members; Caregivers; Visit to Doctor’s Office
Introduction
All over the world women are the predominant providers of informal care for family members with chronic medical conditions or disabilities, including the elderly and adults with mental illnesses. It has been suggested that there are several societal and cultural demands on women to adopt the role of a family-caregiver [1]. So, spouses often serve as the primary caregivers to their ill or disabled partners [2].
The domain of health includes the entire range of issues which touch on illness, sickness, disease, wellness, as well as those activities of preventing, diagnosing, healing, caring and curing. Thus, questions about women’s participation in this domain profound and immediate concern to women, and involve roles and selves. Women have domestic activities which sustain, literally and symbolically, the way of life. As the providers of health, women are responsible for securing the domestic conditions necessary for the maintenance of health and for recovery from sickness. Women also serve as mediators of outside services. Their responsibilities with the domestic health service unavoidably bring them into contact with professional health service, among them the family doctor [3].
In practice, a third person (companion) frequently accompanies a patient during medical encounter. There is a high prevalence of the presence of a companion, who is in almost one of every 4 visits served in Family Medicine. Companions of the patients in the medical office are usually family members in near 100% of cases [4-9].
The major results of existing studies suggest that the regular presences of companions of the patients in consultations are often perceived as helpful. Accompaniment to medical visits is associated with better self-care maintenance and management, and this effect may be mediated through satisfaction with provider communication [10]. Also, companions provide company, emotional support, and they have a role in mobility and decision making of the patients [11,12]. However, their participation often poses challenges [13].
Despite all the above, the reports, reviews or investigations about the gender differences in patient’s companion are rather scarce in our environment. Very little research has examined the influence of the gender in companions who accompany patients on everyday visits to the doctor [5,14,15].
In this context, we present a study whose objectives were to describe gender differences in patient’s companion, and their social and health characteristics, in family medicine consultations.
Methods
An observational, descriptive, prospective study, which included patients of both sexes over 14 years of a family medicine office which has a quota of 2,000 patients, was carried out. The study was performed within a larger one about patient’s companion already published [8]. A random sample was chosen. Comparing retrospectively the percentages obtained from companion’s female (63%) and male (37%), assuming a confidence level of 90%, a power of 80%, and a male / female ratio of 0.5, it would be needed a sample of 67 companions female and 34 companions male [16].
From randomly chosen day for 15 consecutive days, from 26 November 2015 to 18 December 2015, the visited patients were included, and data from the companions with patients were collected. Companion was defined as any person who accompanied the patient in the consulting room or that consult instead the patient. Patients were included only one time. Thus, were excluded the repeated consultations of same patient, including only the first visit. If the patient had two companions only was included the data from the first of them in analysis.
For each patient and companion the following variables were collected: age, sex, chronic disease (defined as “any alteration or deviation from normal that have one or more of the following characteristics: is permanent, leaves residual impairment, is caused by a non-reversible pathological alteration, it requires special training of the patient for rehabilitation, and/or can be expected to require a long period of control, observation or treatment”) [17], and classified according to International Classification of Diseases (ICD-10) [18], taking medication, collecting the therapeutic drugs group, classified according to ATC code or system Anatomic Classification, Therapeutic, Chemical [19], sick leave of the patient, the problems in the family context (based on the genogram, and valued by the same family doctor who performed the genogram at the past time, by viewing the family scheme (the genogram was a schematic model of the structure and processes of a family, included the family structure, life cycle when that family is, the important life events, family resources, and family relational patterns) [20-22], social-occupancy class, according to the Registrar General’s classification of occupations and social status code [23,24], if the analytical or imaging test was requested for the patient, if the patient needs a consultation with the specialist, the companion relationship with the patient, and the social availability of companion in relation to the patient.
A Microsoft Excel® file was built, and the IBM SPSS Statistics for Windows, Version 18.0. Armonk, NY: IBM Corp software was used. Descriptive data, which were expressed by standard measures of central tendency and dispersion, were obtained. The bivariate comparisons were performed using the test of chi-square, with Yates correction when it was pertinent, for the percentages, the Student t test for the mean, exact probability Fischer, and the Mann-Whitney test for comparing means in variables with nonparametric distribution. The informed consent of all patients or their guardians for using of data in research was obtained.
Results
During the 15 days of data collection, a sample of 445 patients was obtained, of whom 104 were companions who accompanied to the patient in the office. 65 (62.5%) were female, and 39 (37.5%) male (Figure 1).
Results of the companions
In the female companions with regard to the male companions: there were 69% in the group of 40-64 years old vs. 49% (p = 0.02); were wife (34%), daughters (33%), and mothers (25%) vs. husband (56%), father (23%), and son (18%) (p=0.001); were unskilled workers in the 68% vs. el 43% (p=0.036); were workers in the 44%, housewife in the 40%, retired in the 8%, and unemployed in the 3% vs. workers 24%, retired in the 49%, and unemployed 19% (p=0.036); had more diseases of the musculoskeletal system and connective tissue (44% vs. 21% in male companions; p=0.024), and they were taking more medications of the musculoskeletal system (26.2% vs. 5.4% in male companions; p=0.014) (Table 1).
| Studied variables | Companion male (n=39) |
Companion female (n=65) |
Statistical significance |
|---|---|---|---|
| Age in years of companions | (n=39) | (n=62) | t=1.496 (p=0.138) |
| 54.54 ± 15.62 | 50.18 ± 13.35 | X2=8.173 | |
| < 40 years: 17.9% | < 40 years:20% | (p=0.02) | |
| 40-64 years: 48.7% | 40-64 years: 69.2% | ||
| = 65 years: 33.3% | = 65 years: 10.8% | ||
| The companion relationship with the patient | (n=39) | (n=64) | p=0.001 |
| Father: 23.1% | Mother: 25% | ||
| Brother: 2.6% | Brother: 0 | ||
| Another familiar: 0 | Another familiar: 4.7% | ||
| Friend: 0 | Friend: 1.6% | ||
| Son: 17.9% | Son: 32.8% | ||
| No family member: 0 | No family member: 1.6% | ||
| Husband 56.4% | Wife: 34.4% | ||
| Chronic disease in companions | (n=37) 1.97 ± 1.50 |
(n=61) 0 |
N.S. |
| Diseases of the musculoskeletal system and connective tissue* | 21.1% / 0.21 ± 0.41 | 43.6% / 0.54 ± 0.68 | p=0.024 (X2) / p=0.012 (U) |
| Medications taken by the companion of the Musculoskeletal system* | 5.4% / 0.05 ± 0.22 | 26.2% / 0.30 ± 0.52 | p=0.014 (X2) / p=0.012(U) |
| Potential problems familiar context of the companion based on the genogram | (n=37) 62.2% (44.75-77.54) |
(n=60) 38.3% (26.07-51.78) |
p=0.36 (X2) |
| Social-occupancy class of companions | (n=35) | (n=59) | p=0.036 (X2). |
| Higher managerial | 0 | 0 |
|
| - Intermediate occupations | 0 | 5.10% | |
| -Specialized whitecollar workers | 5.70% | 3.40% | |
| -Specialized worker’s manuals | 14.30% | 5.10% | |
| -Semiskilled workers | 34.30% | 13.60% | |
| -Unskilled workers | 42.90% | 67.80% | |
| -Students | 2.90% | 5.1% | |
| The social availability of companion in relation to the patient. | (n=37) | (n=63) | P<0.001 (X2) |
| Workers: 24.3% | Workers: 44.4% | ||
| Retired: 48.6% | Retired: 7.9% | ||
| Students: 2.7% | Students: 4.8% | ||
| Housewife: 5.4% | Housewife: 39.7% | ||
| Unemployed: 18.9% | Unemployed: 3.2% |
*In Chronic diseases and Medications taken only statistically significant comparisons are shown
Table 1:Comparisons of the companion female and companion male.
Results of the accompanying patients
Regarding patients accompanied by women, the 52% were male (vs. only 21% of patient’s males who were accompanied by male; p=0.003), and they were unskilled workers in the 53%, and students in the 16% (vs. 64% y 8% respectively in patients accompanied by male; p<0.001) (Table 2).
| Studied variables | Companion male (n=39) |
Companion female (n=62) |
Statistical significance |
|---|---|---|---|
| Age in years of patients | 54.53 ± 20.62 | 52.84 ± 23.64 | t=0.364 (p=0.717) (p=0.735) X2=0.56 |
| (n=38) | (n=63) | ||
| < 40 años 26.3% | < 40 años 32.8% | ||
| 40-64 años 31.6% | (n=64) | ||
| ≥ 65 años 42.1% | 40-64 años 31.3% | ||
| ≥ 65 años 35.9% | |||
| Sex of patients | (n=38) | (n=64) | p=0.003 |
| Males 21.05% (9.55-37.31) |
Males 51.56% (38.72-64.25) |
||
| Women 78.94% (62.68-90.44) |
Women 48.43% (35.75-61.27) |
||
| Number of Chronic diseases in patients | 2.55 ± 1.70 (n=38) |
2.23 ± 1.38 | N.S. |
| Diseases of the ear and mastoid process in patients* | 10.5% / 0.13 ±0.41 |
0 | p=0.017 (PeF) / p=0.017 (U) |
| Number of Medications taken by the patient | 3.16 ± 3.00 | 2.67 ± 2.89 | N.S. |
| Medications taken by the patient of the musculoskeletal system* | 5.3% / 0.05 ± 0.22 | 18.8% / 0.19 ± 0.39 | p=0.075 (X2) / p=0.075 (U) |
| Patients with sick leave | 13.15% (4.41-28.08) |
12.5% (5.55-23.15) |
N.S. |
| Potential problems familiar context of the patient based on the genogram | (n=36) 58.33% (40.75-74.48) |
(n=62) 40.32% (28.05-53.55) |
P=0.097 (χ2) |
| Social-occupancy class of patients | (n=36) | (n=62) | p<0.001 |
| -Higher managerial | 2.80% | 1.60% | |
| -Intermediate occupations | 0 | 0% | |
| -Specialized white-collar workers | 2.80% | 4.80% | |
| -Specialized-workers manuals | 0% | 11.30% | |
| -Semiskilled workers | 22.20% | 12.90% | |
| -Unskilled workers | 63.90% | 53.20% | |
| -Students | 8.30% | 16.30% | |
| Complaint of patient according to ICD-10 | (n=38) | (n=64) | N.S. |
| IX: 21.1% | IX: 17.2% | ||
| XIII: 15.8% | X: 15.6% | ||
| X: 13.2% | XIII: 14.1% | ||
| V y XIV: 10.5% | V: 10.9% | ||
| XI: 9.4% | |||
| Analytical test was requested for the patient | (n=38) 7.89% (1.65-21.37) |
(n=64) 1.56% (0.04-8.40) |
N.S. |
| The patient need a consultation with the specialist | (n=38) 13.15% (4.41-28.08) |
(n=64) 18.75% (10.08-30.46) |
N.S. |
*In Chronic diseases and medications taken only statistically significant comparisons are shown.
Table 2:Comparisons of the patients with companion female and companion male.
Discussion
It has been reported that visits in which one or more family members are present in the medical office are quite common, and their average frequency can be set at around 25% of visits to the doctor [8,9]. It is admitted that companions of the patients are usually family members [4], and predominantly female. Many studies, which have examined gender differences among family-caregivers, have concluded that women spend more time in providing care and carry out personal-care tasks more often than men. This gender bias influences women to assume more substantial caregiving duties [25].
Women are the overwhelming majority of health care providers. Them caring role places them at interface between the family and the state, as the go between linking the informal health-care system with the formal apparatus of the welfare state [3]. There are not one but two systems which determine health beliefs and practices: the lay referral system, which consists in a variable lay culture and a network of personal influences, and the professional referral system of medical culture and institutions. The lay referral system encompasses important features of informal health care. It has a role in the negotiation of health. This concept of referral system serves to highlight the economic contribution which women make in caring for their relatives. The lay accompanying system is located through its cultural and spatial proximity, and in terms of the social relations of gender and generation which underpin family life. We found that 62.5% were women (Figure 1), a figure slightly lower than that reported by Brown (73%) [13], but that study included children, who are usually accompanied by their mothers, whereas in our consultation the patients are attended from the age of 14 years old and greater than 59% reported by other authors [26].
Patient’s companions are typically female and they are part of a systematic informal health care. The provision of accompaniment continues to be organized on an informal individual and unpaid basis within the home. This style of mediation between the public and private domains is well documented in the field of prevention and community caregivers. Becoming a carer involves meeting the needs of those who fall victim to illness and invalidity [3].
We found that the female companions were younger than the male companions (69% in the group of 40-64 years old in female companions vs. 49% in male companions; p = 0.02) (Table 1). This gender gap in care (more caregiving burden among those women in middle age than among those in older age) has been reported (2,13). In our study, were wife (34%), daughters (33%), and mothers (25%) vs. husband (56%), father (23%), and son (18%) (p=0.001), which also broadly coincides with other authors, for whom are the most frequent the mother or wife [6-8].
We also found that female companion of the patient was predominantly worker, and of these, were unskilled workers in the 68% (vs. el 43% in male companion; p=0.036) (Table 1), contrary to published data that women caregivers were less likely to be working [27,28].
Many studies have also found that women and female family caregivers experience greater mental and physical strain, greater caregiver-burden, and higher levels of psychological distress while providing care. However, almost an equal number of studies have not found any differences between men and women on these aspects [1,25,28]. We found that companion female had more diseases of the musculoskeletal system and connective tissue (44% vs. 21% in male companions; p=0.024), and they were taking more medications of the musculoskeletal system (26.2% vs. 5.4% in male companions; p=0.014), but we found no difference in diseases or treatments about mental health (Table 1). Other authors have also noted that women caregivers reported significantly more physically unhealthy days than men, and more physical morbidity (lower physical health scores, poorer physical functioning, and loss of physical strength) [29,30].
The companion assumes the value as intermediary and caregiver. The accompanying person’s role most frequently described is of advocate for the patient [5]. The care of patients “very fragile”, the increasing dependence on their families of elderly patients and/or significant chronic problems, along with the complexity of health services, contributing to the perception that informal caregivers and companions have a role indispensable as “intermediaries between the health system and patient.” Therefore, it is desirable to emphasize the need to discuss further about the fragility of patients with their family companions, which are mainly women, who can be supported and trained to participate in decision-making on tasks for the care of the sick, so that meet the needs of the patient, the doctor and family [31].
This gender bias is particularly marked in the field of women health and child health [3] But, we found that patients accompanied by women were in the 52% male (vs. only 21% of patient’s males who were accompanied by male; p=0.003) (Table 2). So, the gender bias is extending beyond the health of women and children. In this context, two more interventions can be suggested (in addition to education): 1) support interventions for companions of patients should take gender-specific risk factors into account; and 2) this gender bias could be a way to humanize health care.
Patients with greater needs are most often come accompanied, which is positive. Those more likely to have a family member present include patients with a low level of health literacy, patients with chronic diseases, older patients, and women [32,33]. We find that Patients accompanied by women were more frequently male, with fewer ENT diseases, and took more drugs from the musculoskeletal group than male patients (Table 2), which can be globally interpreted as that there was no clinically significant differences between patients according to the gender of her or his companion.
Limitations of our study and future research
The outcomes of impact of gender on companion of the patient may be mediated by several other variables (in addition to those included in this study, such as patient related factors, socio-demographic variables, and effects of kinship status), as culture and ethnicity, but these have not been considered in our research on gender differences [1].
1) We have not studied possible geographical variations (our data refer only to the study area, and it should be prudent to extrapolate them to other geographical areas, which may imply, among other variables, different socio-economic level, beliefs and customs.
2) We have not studied possible gender differences in patient’s companion about information on the health situation and disease in the patient, prevention of anxiety, building of trust, promotes of family dialogue, or aid to decision making.
3) It was not collected the meaning or reason to be present companion.
4) The patients’ perceptions about gender differences of patient’s companion were not collected.
5) The relationships of the gender differences of the patient’s companion with the communication in the consultation have not been studied.
In consequence, future studies could include these topics.
Summary and Conclusion
Patient’s companions are predominantly women, of middle age, wives, mothers and daughters, with poor health, low social class, housewives and workers. Male companions are older, husbands and fathers, with better health than female companions, of middle class, and retirees. Patients accompanied either by women or by men have a similar health status. Patients accompanied by women are males, students, of middle class, vs. patients accompanied by men who are women of low social class. The companion “type” is a middle-aged woman, wife, with poor health, low social class, housewife or worker, who accompanying a patient male or student of middle class.
The presence of companion female of patient, usually family members, with the characteristics described above, creates unique opportunities for supporting interventions for this gender bias, which could have better outcomes for the health of family members (patient outcomes as depression, anxiety, relationship satisfaction, disability, and mortality, and family member outcomes as depression, anxiety, relationship satisfaction, and caregiving burden) [28,34,35] (Box 1). Companion seems to play a secondary role, but it can be the main actor [36]. And the gender differences should remind us take into accounts specially the companion female during assistance in individual patients. A female adult, usually the wife, accompanying to the patient in consultation, is always significant and deserves the attention of the doctor. So, it needs a gender oriented practice in relation to patient’s companion [37-47].
References
- Greenland P, Labree L, Azen SP, et al. Coronary artery calcium score combined withframinghamscore for risk prediction in asymptomatic individuals. JAMA 2004;291:210-15.
- Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: A 37-month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation 2003;107:2571-76.
- O’Malley PG, Taylor AJ, Jackson JL, et al.Prognostic value of coronary electron- beam computed tomography for coronary heart disease events in asymptomatic populations. Am J Cardiol 2000;85:945-48.
- Pletcher MJ, Tice JA, Pignone M, et al.Using the coronary artery calcium score to predict coronary heart disease events. Arch Intern Med 2004;164:1285-92.
- Shaw LJ, Raggi P, Schisterman E, et al. Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. Radiology 2003;228:826-33.
- Elias-Smale SE, Proença RV, Koller MT, et al. Coronary calcium score improves classification of coronary heart disease risk in the elderly: The Rotterdam study. J Am CollCardiol 2010;56:1407-14.
- Erbel R, Möhlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: The Heinz Nixdorf Recall study. J Am CollCardiol 2010;56:1397-06.
- Polonsky TS, Mcclelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010;303:1610-16.
- Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol 2010;56:e50-e103.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals : Arandomised placebo- controlled trial. Lancet2002;360:7-22.
- LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. NEJM2005;352:1425-35.
- The long-term intervention with pravastatin in ischaemic disease study group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. NEJM1998;339:1349-57.
- Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. NEJM1996;335:1001-09.
- Scandanavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease:The Scandinavian Simvastatin Survival Study (4S). Lancet1994;344:1383-89.
- Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. NEJM1995;333:1301-07.
- Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels. JAMA1998;279:1615-22.
- Pedersen TR, Faergeman O, Kastelein JJP, et al. High-dose atorvastatin vs. usual-dose simvastatin for secondary prevention after myocardial infarction. JAMA 2005;294:2437-46.
- Nissen SE, Nicholls SJ, Siphani I, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis. JAMA 2006;295:1556-65.
- Nicholls SJ, Ballantyne CM, Barter PJ, et al. Effect of two intensive statin regimens on progression of coronary disease. NEJM 2011;365:2078-87.
- Puri R, Nicholls SJ, Shao M, et al. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am CollCardiol 2015;65:1273-82.
- Yla-Herttuala S, Bentzon JF, Daemen M, et al. Stabilization of atherosclerotic plaques: an update. Eur Heart J 2013;34:3251-58.
- Callister TQ, Raggi P, Cooil B, et al. Effect of HMG-CoA reductase inhibitors on coronary artery disease as assessed by electron-beam computed tomography. NEJM1998;339:1972-78.
- Budoff MJ, Lane KL, Bakhsheshi H, et al. Rates of progression of coronary calcium by electron beam tomography. Am J Cardiol 2000;86:8-11.
- Achenbach S, Ropers D, Pohle K, et al. Influence of lipid-lowering therapy on the progression of coronary artery calcification: Aprospective evaluation. Circulation 2002;106:1077-82.
- Arad Y, Spadaro LA, Roth M, et al. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin c, and vitamin E. J Am CollCardiol 2005;46:166-72.
- Houslay ES, Cowell SJ, Prescott RJ, et al. Progressive coronary calcification despite intensive lipid-lowering treatment: a randomised controlled trial. Heart2006;92:1207-12.
- Terry JG, Carr JJ, Kouba EO, et al. Effect of simvastatin (80 mg) on coronary and abdominal aortic arterial calcium (from the coronary artery calcification treatment with zocor [CATZ] study). Am J Cardiol 2007;99:1714-17.
- Schmermund A, Achenbach S, Budde T, et al. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: A Multicenter, Randomized, Double-Blind Trial. Circulation2006;113:427-37.
- Raggi P, Davidson M, Callister TQ, et al. Aggressive versus moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: beyond endorsed lipid lowering with EBT scanning (BELLES). Circulation 2005;112:563-71.
- Plazak W, Gryga K, Dziedzic H, et al. Influence of atorvastatin on coronary calcifications and myocardial perfusion defects in systemic lupus erythematosus patients: A prospective, randomized, double-masked, placebo-controlled study. Arthritis Res Ther 2011;13:R117.
- Lemos MM, Watanabe R, Carvalho AB, et al. Effect of rosuvastatin and sevelamer on the progression of coronary artery calcification in chronic kidney disease: A pilot study. ClinNephrol 2013;80:1-8.
- Tenenbaum A, Shemesh J, Koren-Morag N, et al. Long-term changes in serum cholesterol level does not influence the progression of coronary calcification. Int J Cardiol2011;150:130-34.
- Goh VK, Lau C-P, Mohlenkamp S, et al.Outcome of coronary plaque burden: A 10-year follow-up of aggressive medical management. Cardiovasc Ultrasound 2010;8:5.
- Anand DV, Lim E, Darko D, et al. Determinants of progression of coronary artery calcification in type 2 diabetes. Role of glycemic control and inflammatory/vascular calcification markers. J Am CollCardiol 2007;50:2218-25.
- Burgstahler C, Reimann A, Beck T, et al. Influence of a lipid-lowering therapy on calcified and noncalcified coronary plaques monitored by multislice detector computed tomography: results of the New Age II Pilot Study. Invest Radiol 2007;42:189-95.
- Mohler ER, Wang H, Medenilla E, et al.Effect of Statin treatment on aortic valve and coronary artery calcification. J Heart Valve Dis 2007;16:378-86.
- Budoff MJ, Yu D, Nasir K, et al. Diabetes and progression of coronary calcium under the influence of statin therapy. Am Heart J 2005;149:695-00.
- Hecht HS, Harman SM. Evaluation by electron beam tomography of changes in calcified coronary plaque in treated and untreated asymptomatic patients and relation to serum lipid levels. Am J Cardiol 2003;91:1131-34.
- Lo J, Lu MT, Ihenachor EJ, et al. Effects of statin therapy on coronary artery plaque volume and high-risk plaque morphology in HIV-infected patients with subclinical atherosclerosis: Arandomised, double-blind, placebo-controlled trial. Lancet HIV 2015;2:e52-e63.
- Zeb I, Li D, Nasir K, et al. Effect of statin treatment on coronary plaque progression - a serial coronary CT angiography study. Atherosclerosis 2013;231:198-04.
- Hoffmann H, Frieler K, Schlattmann P, et al.Influence of statin treatment on coronary atherosclerosis visualized using multi-detector computed tomography. EurRadiol 2010;20:2824-33.
- Inoue K, Motoyama S, Sarai M, et al. Serial coronary CT angiography-verified changes in plaque characteristics as an end point: evaluation of effect of statin intervention. JACC Cardiovasc imaging 2010;3:691-98.
- Auscher S, Heinsen L, Nieman K, et al. Effects of intensive lipid-lowering therapy on coronary plaques composition in patients with acute myocardial infarction: Assessment with serial coronary CT angiography. Atherosclerosis 2015;241:579-87.
- Henein M, Granåsen G, Wiklund U, et al. High dose and long-term statin therapy accelerate coronary artery calcification. Int J Cardiol 2015;184:581-86.
- Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression. JAMA 2004;291:1071-80.
- Puri R, Libby P, Nissen SE, et al. Long-term effects of maximally intensive statin therapy on changes in coronary atheroma composition: Insights from SATURN. Eur Heart J Cardiovasc Imaging 2014;15:380-88.
- Eshtehardi PP, McDaniel MC, Dhawan SS, et al. Effect of intensive atorvastatin therapy on coronary atherosclerosis progression, composition, arterial remodeling, and microvascular function. J Invasive Cardiol 2012;24:522.