The Thyroid ima Artery: A Cadaveric Study
2 Edward Via College of Osteopathic Medicine- Virginia Campus (VCOM-VA), United States
Received: 29-Jul-2021 Accepted Date: Aug 17, 2021; Published: 25-Aug-2021, DOI: 10.37532/1308-4038.14(8).123-124
Citation: Smith T, Carpenetti T, Swaak A. The Thyroid IMA Artery: A Cadaveric Study. Int J Anat Var. 2021;14(8):123-124.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
In the operating theater, it is of the upmost importance that the surgeon has a comprehensive knowledge of the anatomy within their surgical field. For the otolaryngologist, intimate knowledge of the neurovascular anatomy of the neck is required, especially during surgical procedures relating to the thyroid gland. Along with knowledge of the typical anatomy, the otolaryngologist should also be aware of specific anatomical variants. One such variant is the thyroid ima artery, commonly located inferior to the thyroid gland. In the study presented, 26 cadavers at Edward Via College of Osteopathic Medicine were carefully dissected, and it was determined that two of 26 (further identified as donor 121 and 303) displayed the variant ima artery. For donor 303, the artery was located supplying a pyramidal lobe on the inferior portion of the thyroid gland, and originated from the brachiocephalic artery. It is the authors hope that this case study lends to further knowledge of the thyroid ima and its characteristics, and ultimately improved surgical awareness.
Keywords
Thyroidectomy; Otolaryngologist
Introduction
The common otolaryngologist procedure, the thyroidectomy, is performed over 50,000 times per year. Despite its frequency, various complications are still known to occur. These complications include post-operative bleeding, recurrent laryngeal nerve injury, and iatrogenic hypocalcaemia. Hypocalcaemia can be secondary to interruption of the parathyroid vascular supply or unintended removal of the four glands during the thyroidectomy. As such, it is important that the otolaryngologist has a comprehensive understanding of head and neck anatomy as well as the potential neurovascular variants faced within the surgical field.
The parathyroid glands are supplied by the left and right inferior thyroid arteries which arise from their respective thyrocervical trunk, a branch of the subclavian artery. This is the more common arterial branching pattern that the otolaryngologist takes care to preserve during thyroidectomy. However, favorable outcomes can be complicated by anatomical variants, such as the aberrant thyroid ima artery (TIA), which has a rare and unpredictable presentation [1].
The TIA, when present, traverses the superior mediastinum to reach the thyroid gland, acting as additional blood supply to the thyroid isthmus, pyramidal lobe and inferior parathyroid glands. It also acts as a compensatory if one or bilateral inferior thyroid arteries are absent [2]. A remnant of the thyrocervical duct, the pyramidal lobe can be present in over 50% of patients [3].
Materials and Methods
26 donors were dissected using standard methods at the Edward Via College of Osteopathic Medicine in Blacksburg, VA. All donors were dissected to the level of the thyroid gland.
Results
The Of the 26, two displayed a TIA and are represented here as donors 121, and 303.
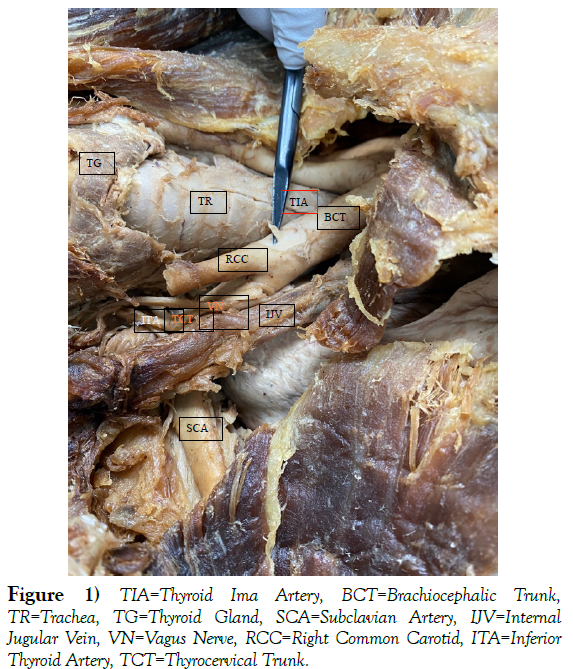
Donor 121 appeared to possess a TIA; however, at the time the study occurred partial dissection of the neck had already been performed. Due to this, the full course of the possible TIA could not be studied further. The trunk of the TIA in donor 121 can be seen in (Figure 1) as originating from the brachiocephalic trunk. It should be noted that this donor does not display a pyramidal lobe, a common finding in patients with a TIA.
Figure 1: TIA=Thyroid Ima Artery, BCT=Brachiocephalic Trunk, TR=Trachea, TG=Thyroid Gland, SCA=Subclavian Artery, IJV=Internal Jugular Vein, VN=Vagus Nerve, RCC=Right Common Carotid, ITA=Inferior Thyroid Artery, TCT=Thyrocervical Trunk.
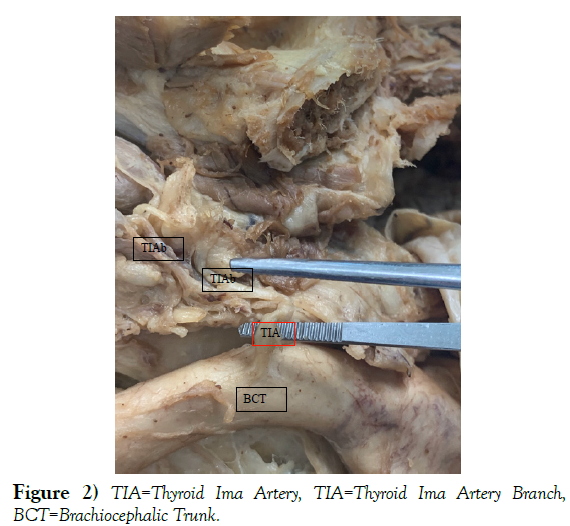
Donor 303 was dissected until the thyroid gland was exposed, and a midline pyramidal lobe was noted just inferior to the thyroid gland. It was also noted that the inferior thyroid arteries to the gland were reduced in size compared to normal. As seen in (Figure 2), the course of the artery supplying the pyramidal lobe and inferior thyroid gland was exposed, revealing its origin from the brachiocephalic trunk, rather than the thyrocervical trunk, thus confirming the presence of TIA.
Discussion
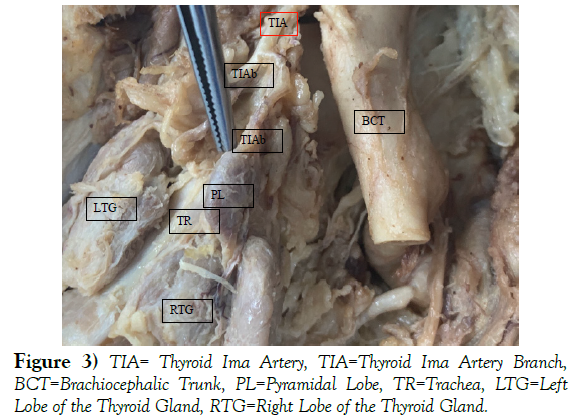
The The incidence of the thyroid ima artery varies within the literature from 0.4 to 12.2%. At Touro College of Osteopathic Medicine, dissections of 94 cadavers were performed with only one demonstrating a thyroid ima artery. This suggested a prevalence of 1.06 percent within the cadaveric population (Figure 3). Within our study population, a total of 2 out 26 displayed the TIA and as such, a prevalence of 7.7% was demonstrated. While this is not consistent with Touro College of Osteopathic Medicine’s findings, it still within the range noted in the literature as mentioned above.
Cadaveric and radiological case studies note variation in origin site, most commonly arising from the brachiocephalic trunk (43.3-86.7%) but also from the common carotid (2-50%) and aortic arch (0-66.7%) [4]. Both donors 121 and 303 branched off the brachiocephalic trunk, the more common branching location.
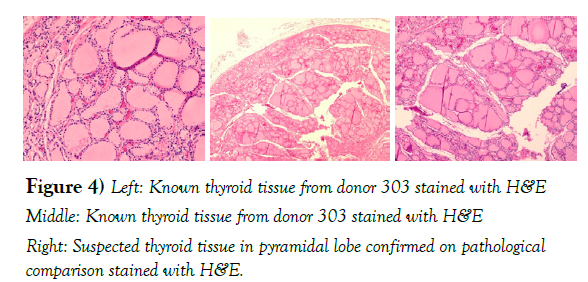
One such study of the pyramidal lobe suggested that over 90% of lobes were primarily supplied by a single artery that was a variant of normal arising from the superior thyroid artery. With such a strong correlation between the pyramidal lobe and aberrant blood supply, this study reiterates the importance of intraoperative identification of a pyramidal lobe and its blood supply. In the case of donor 303, the pyramidal lobe was histologically proven to be thyroid tissue by histological comparison to tissue harvested directly from the thyroid gland (Figure 4).
Conclusion
The TIA is a rare variant of normal, having a significant association with the pyramidal lobe, and as such, should be carefully avoided. Pre-operative scans can be useful in the identification of this variant. The study performed at VCOM reproduces statistical data consistent with current published data, and further lends to the pool of data of a relatively rare variant. Proper knowledge of potential anatomical variants is vital for the operating surgeon. In the setting of a pyramidal lobe, especially if the lobe is inferior to the thyroid gland, noting the presence of the TIA could significantly reduce the risk of complication.
REFERENCES
- Chin J, Zhou Y, Wan P et al. The prevalence of thyroid ima artery and its clinical significance. Int J Otorhinolaryngol Head Neck Surg. 2019; (5): 845.
- Steward WB, Rizzolo LJ. Embryology and Surgical Anatomy of the Thyroid and Parathyroid Glands. Surg Clin North Am. 2012
- Mangalgiri A, Mahore D, Kapre M. Pyramidal Artery: An Artery to Pyramidal Lobe-A New Nomenclature. Int J Otolaryngol Head Neck Surg. 2018;70:313-318.
- Yohannan DG, Rajan R, Chandran AB, et al. An unusual origin and course of the thyroidea ima artery, with absence of inferior thyroid artery bilaterally. Anatomia clinica. 2019; 41(2): 235-237.