The Up-folded Mammary Gland For Free-nipple-graft Reduction Mammoplasty
2 Department of Plastic Surgery, College of Medicine, Zhejiang University, Hangzhou, Zhejiang Province, P.R. China
Received: 09-Sep-2017 Accepted Date: Sep 27, 2017; Published: 29-Sep-2017
Citation: Tan WQ, Zhang MX, Chen CY, et al. The up-folded mammary gland for free-nipple-graft reduction mammoplast. Surg Case Rep. 2017;1(1):2-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Free-nipple-graft reduction mammoplasty (RM) is the procedure of choice in patients with major hypertrophy and ptosis. The limitations of most free-nipple-graft reduction techniques include insufficient breast projection and various complications. The authors have designed a method of free-nipple-graft RM with the mammary tissue folded upward to provide a conical breast with adequate projection.
Methods: Based on the principle of breast reduction, preoperative markings were made. After the planned tissue was excised, breast remodeling was done, followed by folding the mammary tissue upward to be sutured to the pectoral fascia. The entire nipple-areola complex (NAC) was removed to a new position as a graft. The evaluation included the amount of resection, complications, and postoperative breast shape.
Results: Two patients underwent free-nipple-graft reduction with the modified technique. The inclusion criteria specified major breast hypertrophy and ptosis larger than 1500-cc volume per side, and nipple-areola transposition greater than 15 cm. An average tissue of 1,498 g for one person and 1,313 g for the other per breast was excised. There were no complications and the patients were both satisfied with the relief of symptoms as well as with the shape and projection of their breasts.
Conclusion: The up-folded mammary gland yields a conical breast with adequate projection, leaving no complications. Parenchyma sutures to the pectoral fascia provide favorable projection. The inverted T creates a dog-ear, which greatly enhances nipple projection. This operative method is a simple and effective technique for patients with major hypertrophy and ptosis, especially whose nipple-areola transposition is greater than 15 cm.
Keywords
Hypertrophy; Ptosis; Reduction mammoplasty; Free nipple graft
Reduction mammoplasty (RM) can not only improve the appearance, but also reduce the symptoms from breast hypertrophy. Free-nipple-graft RM is one of the procedures used to treat patients with major hypertrophy and ptosis. In 1922, Thorek et al. first described a standard free nipple RM for gigantomastia [1], which yielded a wide, flat breast but resulted in insufficient projection. A great number of modifications to the technique have been described to solve the problem [2,3]. However, these techniques are frequently criticized for irretentive breast projection due to the central and inferior resection of the glandular tissue that has sagged down.
We have designed a new method of free-nipple-graft RM with the mammary tissue folded upward for patients with major hypertrophy and ptosis, especially whose nipple-areola transposition is greater than 15 cm. Our modification results in a well-contoured breast with no complications.
Materials and Methods
Study population
Our research had been approved by the ethics committee of the first affiliated hospital, college of medicine, Zhejiang University. The informed consents of patients to participate in the study were obtained.
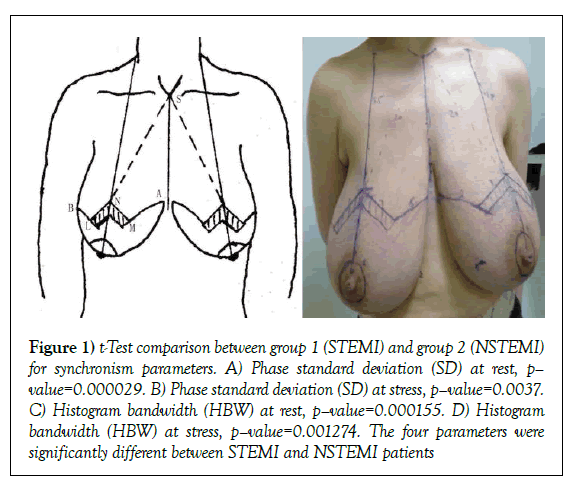
We applied our new method on two patients who had large breasts (minimum, 1500-cc volume), aged 28 and 40 years on October 2008 and March 2011 separately. The two patients were both non-obese ones (BMI<30 kg/m2), with no history of radiation therapy and smoking. The evaluation included the amount of resection, complications, and postoperative breast shape. The two patients’ clinical symptoms and signs were as follows: [1] neck, back or shoulder pain, [2] inframammary maceration, (3) difficulty with breathing during exercise, and [4] great psychological burden because of unaesthetic appearance. Inclusion criteria were (1) major hypertrophy and ptosis with nipple-areola transposition greater than 15 cm, [2] a strong desire to shrink her breasts, and [3] willing to give up breast-feeding postoperatively. Preoperative markings were made with the patient in the standing position. The suprasternal notch (S), sternal midline, and clavicle-nipple line were marked. We assigned N, on the clavicle-nipple line, as the new nipple position according to the SN line (SN=body length × (12%–12.5%) ± 1 cm). Based on the breast tissue to be excised, we designated an angle M-N-L of about 60°–110° (NM=NL=7 cm, which is the distance from the new nipple to the inframammary fold). Then we positioned A and B, 2 cm above the inside and outside the inframammary fold, respectively (Figure 1) for location of landmarks). These points can be adjusted to ensure that MA+LB=AB. Two parallel lines were drawn 2 cm below NM and NL, forming the deepithelialized area. Nipple-areola was planned to be 4.2 cm in diameter (Figures 1A-1D).
Figure 1: t-Test comparison between group 1 (STEMI) and group 2 (NSTEMI) for synchronism parameters. A) Phase standard deviation (SD) at rest, p– value=0.000029. B) Phase standard deviation (SD) at stress, p–value=0.0037. C) Histogram bandwidth (HBW) at rest, p–value=0.000155. D) Histogram bandwidth (HBW) at stress, p–value=0.001274. The four parameters were significantly different between STEMI and NSTEMI patients
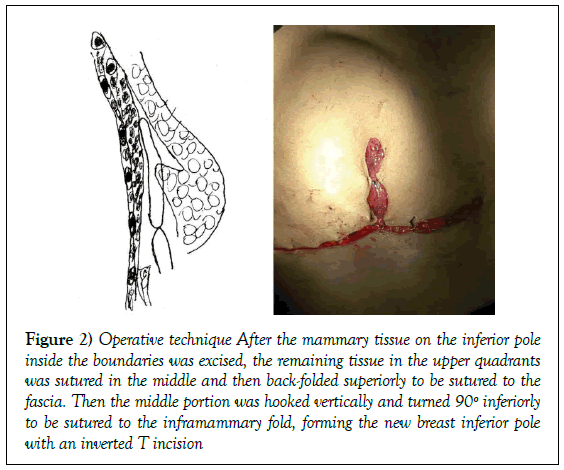
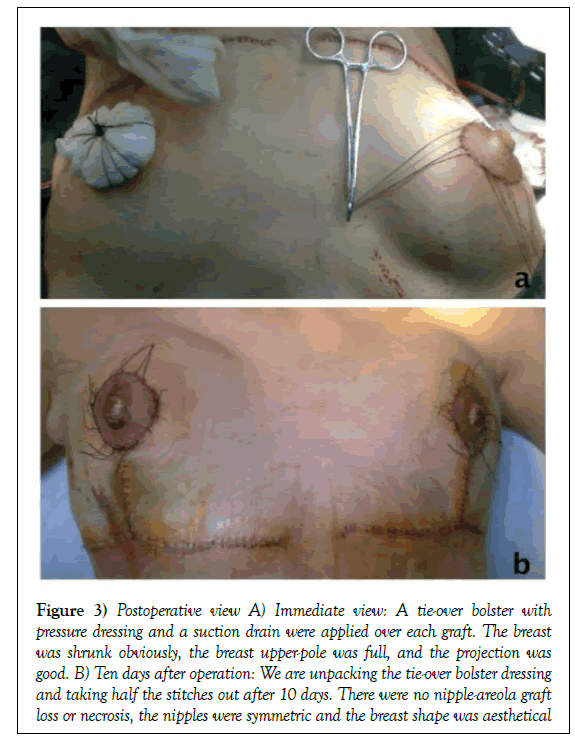
After the nipple-areola complex (NAC) was harvested from the deep dermal layer as a full-thickness skin graft, the two rectangles in M-N-L were deepithelialized. A keel-shaped section of mammary tissue on the inferior pole inside the boundaries demarcated by the pattern was vertically excised after it was separated from the pectoral fascia by blunt dissection. The bilateral excised tissue was evaluated to ensure that the remainder was equal on both sides. The remaining tissue in the upper outer and inner quadrants continued to be separated over the second intercostal space, passed, and sutured in the middle and then back-folded superiorly to be sutured to the fascia of the pectoralis major muscle. This procedure increased upper-pole fullness and produced adequate projection. Then the middle portion was hooked vertically and turned 90º inferiorly to be sutured to the inframammary fold, forming the new breast inferior pole with an inverted T incision (Figure 2). Finally, the NAC was sutured in the new nipple-areola position, which was marked off at 3.8 cm in diameter. A tie-over bolster with pressure dressing was applied over each graft (Figure 3A). Postoperative drainage was performed. We removed the drains after 2 or 3 days, unpacking the tie-over bolster dressing and taking half the stitches out after 10 days (Figure 3B). Finally, the remaining stitches were taken out after 14 to 21 days.
Figure 2: Operative technique After the mammary tissue on the inferior pole inside the boundaries was excised, the remaining tissue in the upper quadrants was sutured in the middle and then back-folded superiorly to be sutured to the fascia. Then the middle portion was hooked vertically and turned 90º inferiorly to be sutured to the inframammary fold, forming the new breast inferior pole with an inverted T incision
Figure 3: Postoperative view A) Immediate view: A tie-over bolster with pressure dressing and a suction drain were applied over each graft. The breast was shrunk obviously, the breast upper-pole was full, and the projection was good. B) Ten days after operation: We are unpacking the tie-over bolster dressing and taking half the stitches out after 10 days. There were no nipple-areola graft loss or necrosis, the nipples were symmetric and the breast shape was aesthetical
Results
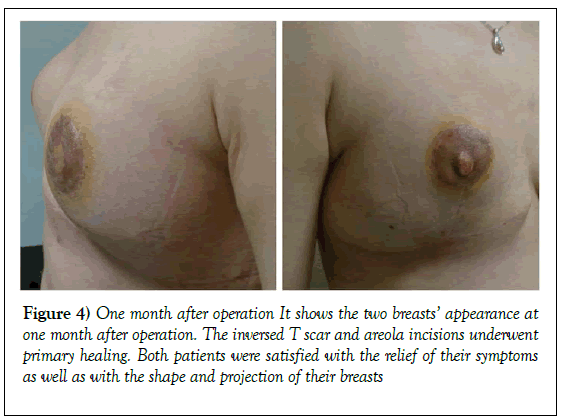
The average resection weight was 1,498 g for one patient and 1,313 g for the other, the distance from the sternal notch to the new nipple position was 21 cm and 20 cm, and the distance from the new nipple to the original was 16.5 cm and 15 cm. We evaluated the complications on ten days and one month after operation, neither of them experienced nipple-areola graft loss, nipple necrosis, infection or wound dehiscence (Figures 3B and 4). The inverted T scar and areola incisions at the level of the inframammary fold medially and laterally underwent primary healing and became inconspicuous gradually. Both patients were satisfied with the relief of their symptoms as well as with the shape and projection of their breasts (Figure 4).
Discussion
For women with major or gigantic mammary hypertrophy and ptosis, freenipple- graft RM is usually recommended. In Ahmed’s opinion, there is good recovery of sensation and erotic function in free nipple-areolar grafts, and that free nipple grafting is a good procedure in selected patients. Accordingly, he recommended it as a safe alternative when pedicle techniques were relatively contraindicated [4]. Marshall et al. [5] advocated to use free nippleareola graft based on the technique of vertical incisions on patients whose nipple-areola transposition greater than 15 cm. However, breasts that have undergone free-nipple-graft RM usually cannot maintain projection because of lacking in central breast tissue that forms the anatomic projection. Several modifications have been described to achieve aesthetically desirable results. Spear et al. [6] had ever used the middle portion of the breast to increase the breast projection. However, folding the middle portion upward and fixing it to the fascia are not used, that adequate projection cannot be maintained.
Two steps in our technique were the most important for further increasing breast projection. The first was to suture the middle portion and fold it upward to greatly enhance breast projection. The second was to suture the folded tissue to the fascia to maintain the projection. Creating a dog-ear at the tip of the new nipple like Casas et al. [7] is very useful for the conical shape and stable nipple projection. Unsatisfactory breast shape due to improper gland and skin firmness during suturing incisions used in other methods can be avoided in our technique. Fernandez et al. [8] put forward that better scarring was associated with inverted T scar pattern versus vertical pattern. So, in our technique with inverted T scar pattern, the incision scar will be seen but it is covert, and the scar usually regresses inconspicuously within 3 months, which will not be patient’s trouble.
Besides the satisfied breast shape, the evaluation of postoperative complications was also favorable using our new technique. Once we had got the conclusion that BMI ≥ 30 kg/m2 and radiation therapy showed a statistically higher incidence of infection and smokers acquired higher significant rates of wound dehiscence [9]. However, age ≥ 50 years and tissue resection weight ≥ 1000 g is not associated with post-RM complications [9]. The two patients’ BMI in our study were 26 and 24 kg/m2, and they had not suffered radiation therapy previously, which reduced the infection chance. Similarly, being far away from smoking made no rates of wound dehiscence. Age and tissue resection weight did not have influence on complications. Apart from the risk factors above, do the surgical technique influence the postoperative complications? It is still unknown because the searched data of different surgical techniques from the existing studies cannot be merged [9]. What we do know is that there are numerous alternatives to RM and different complications are occurred along with different reported techniques. For example, the short scar periareolar inferior pedicle reduction can lead to delayed wound healing, widened or unattractive scar, and shape distortion as Dennis et al. [10] reported. Derby et al. [11] once drew a conclusion that superomedial pedicle increased rates of postoperative fat necrosis. If we understood why the complication occurred in specific technique, we could choose the most suitable one. Zhao et al. [12] suggested that the complications may be related to destroyed blood supply, which was due to excess excision of tissue. We suppose that blood supply was well reserved in our freenipple graft RM, which was the reason that there were no complications postoperatively. Therefore, free-nipple-graft RM with mammary gland upfolded is a good choice for patients with major hypertrophy and ptosis versus other techniques with various complications. Of course, further large-scale studies are needed to verify the conclusion.
To ensure to create projecting nipples and breasts of excellent contour with no complications, there are many points in our reported technique as follows:
1. Patients who have major or gigantic breast hypertrophy and ptosis should give up breast-feeding postoperatively.
2. Patients should be encouraged to lose weight and stop smoking before surgery if their BMI ≥ 30 kg/m2 or they are smokers.
3. Preoperative markings should be made with the patient in the standing position.
4. According to the degree of breast hypertrophy and ptosis, the preoperative angle (M-N-L) is designed between 60°–110°. More tissue will be removed by widening the angle; by narrowing the angle, more tissue can be retained. To avoid high tension, the angle should not be too large.
5. A tie-over bolster with pressure dressing is needed. It can not only facilitate hemostasis and avoid cavitation, but also prevent subcutaneous effusion. More importantly, a pressure dressing can generate skin shrinkage to help create an excellent breast contour.
We recognized several limitations in our study. First, there are only two patients with four breasts using our new technique that large-scale studies are needed to confirm the satisfied results. Second, the follow-up time is 18 months for one patient and 3 months for the other. Although we got acquaint with the two patients five years after the operation, they refused being photographed that we could not provide picture evidence. It is necessary to prolong the follow-up time if possible to get the enough postoperative data, which is required for our further study.
Conclusion
Our modified technique of the up-folded mammary gland for free-nipplegraft RM creates an aesthetic breast with adequate shape and projection, as well as with no complications. We consider it may be a safe and effective technique for patients with major hypertrophy and ptosis, especially whose nipple-areola transposition is greater than 15 cm.
Acknowledgement
The authors thank all subjects involved in this study.
Conflict of Interest
None.
REFERENCES
- Karsidag S, Akcal A, Karsidag T, et al. Reduction mammaplasty using the free-nipple-graft vertical technique for severe breast hypertrophy: improved outcomes with the superior dermaglandular flap. Aesthetic Plast Surg. 2011;35(2):254-61.
- Ozerdem OR, Anlatici R, Maral T, et al. Modified free nipple graft reduction mammaplasty to increase breast projection with superior and inferior dermoglandular flaps. Ann Plast Surg. 2002;49(5):506-10.
- Eggert E, Schuss R, Edsander-Nord A. Clinical outcome, quality of life patients’ satisfaction, and aesthetic results, after reduction mammoplasty. Scand J Plast Reconstr Surg Hand Surg. 2009;43(4):201-6.
- Ahmed OA, Kolhe PS. Comparison of nipple and areola sensation after breast reduction by free nipple graft and inferior pedicle techniques. Br J Plast Surg. 2000;53(2):126-29.
- Marshall WR, Notma KR, Camille K. The US health system origin and functions (M). (5th ed). New York, USA: Delmar Thomson Learning. 2002;180.
- Spear SL. Breast reduction: inverted-T technique. In: Thorne C, Grabb WC, Smith JW (eds) Grabb and Smith’s plastic surgery. Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia, USA. 2007.
- Casas LA, Byun MY, Depoli PA, et al. Maximizing breast projection after free-nipple-graft reduction mammaplasty. Plast Reconstr Surg. 2001;107(4): 961-64.
- Fernandez S, Coady L, Cohen-Shohet R, et al. Comparative outcomes and quality analysis of inverted-T and pure vertical scar techniques in superomedial pedicle reduction mammaplasty. Ann Plast Surg. 2016;76Suppl 4: S328-31.
- Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: A meta-analysis. PLoS One. 2016;11(12): e0167746
- Dennis C, Hammond, Kuylhee K. The short scar periareolar inferior pedicle reduction mammaplasty: management of complications. Clin Plast Surg 2016;43(2):365-72.
- Derby BM, Grotting JC, Redden DT. Vertical sculpted pillar reduction mammaplasty in 317 patients: Technique, complications, and Breast-Q outcomes. Aesthet Surg J. 2016;36(4):417-30.
- Zhao R, Qiao Q. Analysis of the complications of two kinds reduction mammaplasty. Zhonghua Zheng Xing Wai Ke Za Zhi. 2007;23(5):375-77.