The use of benzodiazepines in bipolar disorders
2 Department of Psychiatry, Mohamed V Military Hospital, Rabat, Morocco, Email: Dr.yassine.otheman@gmail.com
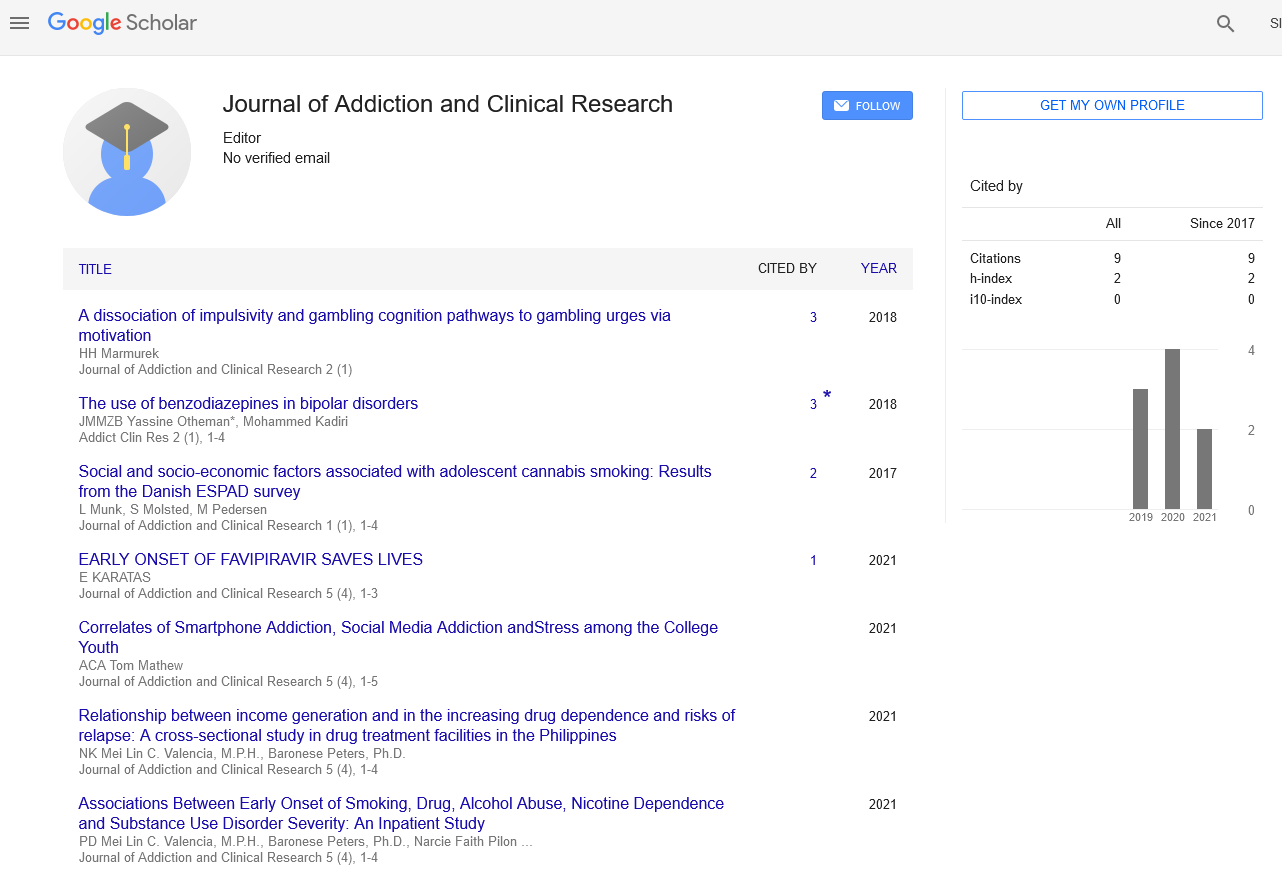
Citation: Otheman Y, Kadiri M, Mehsanni J, et al. The use of benzodiazepines in bipolar disorders. Addict Clin Res 2018;2(1):1-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
INTRODUCTION: Benzodiazepines are widely prescribed for patients with bipolar disorders, especially in episodes of mood disturbances. However, comorbid anxiety, sleep problems and substance abuse are frequent in these patients, and may lead to more prescription of benzodiazepines in inter-critic period. DISCUSSION: While acute anxiety/sleep problems and substance withdrawal syndromes are potential indications for short-term benzodiazepines use, the long-term use may aggravate the outcome of bipolar disorders, clinically and functionally, and lead to poor prognosis in general. The lack of studies about the management strategies, in patients coming with bipolar disorders and one of these particular situations, is the reason why the use of benzodiazepines may still be a solution for many practitioners, but that must be done with a lot of caution. This situation highlights the need to explore more deeply this important question. CONCLUSION: Although benzodiazepines have many benefits for patients with bipolar disorders, their use must be very cautious, because of the associated risk of misuse and other possible consequences, especially in some particular clinical situations. Concerns remain about efficacious alternatives to manage comorbid anxiety, sleep disturbances and substance use disorders. Despite the clinical importance of that issue, there is a lack of randomized studies. Due to ethical reasons, this situation highlights the need to explore more deeply this question, by naturalistic studies and neurobiological research, to better understand the role of BZD and GABAergic mechanisms in the pathophysiology of BD, anxiety and sleep disturbances.
Keywords
Benzodiazepines; Bipolar disorders; Anxiety; Sleep disturbances; Substance abuse
Benzodiazepines
Benzodiazepines (BZD) are one of the most prescribed pharmacological agents in the world [1,2], despite the risks of dependence, abuse and other concerns [3]. They are widely prescribed for patients with mental disorders such as schizophrenia, major depressive disorder, opioids detoxification, anxiety disorders and bipolar disorders (BD) [4,5].
Because of the high prevalence of anxiety and insomnia in patients with BD, benzodiazepines are commonly used by these patients [6,7], prevalence of BZD use among bipolar patients is varying from 58% to 75% [5,8].
Prescribing BZD in patients with BD must be weighed depending on the clinical presentation, and individual story of substance abuse. The variety of mood state and the frequency of comorbidity in BD, especially with anxiety disorders, sleep disturbances and substance abuse, make it difficult to have a unique strategy of BZD prescription. In this article, after a brief presentation of BZD and BD, we will address different situations where BZD may be used in bipolar patients and the problems they may pose.
Benzodiazepines are psychoactive drugs that were discovered accidentally by Leo Sternbach in 1955. They were first greeted by practitioners and patients, and were among the most prescribed drugs in the 1970s. This popularity has since been slowed down by many shortcomings, like abuse, dependence and cognitive impairment [9].
The mechanism of action of BZD is based on the enhancement of GABA (gamma-amino-butyric acid) at the GABAA receptor. GABA is the major inhibitory neurotransmitter in the central nervous system. BZD have many properties: anticonvulsant, hypnotic, muscle relaxant, amnesic and anxiolytic. However, they are more used by physicians to reduce anxiety and insomnia [3].
Benzodiazepines are indicated for short-term treatment of severe anxiety, occurring alone or in association with insomnia or short term organic or psychiatric disorders; while only severe or disabling insomnia should be treated by BZD for a short period [3,10]. Many side effects may occur with BZD, especially paradoxical excitement that may have possible legal implications due to aggressive impulses or hostility [3].
Discontinuation maybe accompanied by a withdrawal syndrome that can include a rebound of anxiety and insomnia, with a prolonged sleep onset, nightmares, irritability and muscle spasms. These symptoms are usually reversible in few days, but the patient often resumes medication and becomes dependent to it [11,12].
Moreover, BZD are widely misused, especially in the context of recreational or addictive behaviors [13]. There is also a lot of evidences, suggesting cognitive impairment in the long term users of BZD [14,15], and an exacerbation of cognitive dysfunction in patients with bipolar disorders who have BZD dependence [16,17]. Recent data show that even low usage of BZD was associated with increased risk of mortality [18,19].
Literature Review
Bipolar disorders
Bipolar disorders are common, chronic and of variable severity. They are characterized by recurrent episodes of mania with or without episodes of major depression (bipolar I disorder), or episodes of hypomania and major depression (bipolar II disorder) [20]. The presence of at least four mood episodes that meet the criteria for manic, hypomanic, or major depressive episode, in the last year, define rapid cycling BD [20]. The lifetime prevalence is 1% for bipolar I and 0.5 to 1.57% for bipolar II disorders [21,22]. Bipolar disorders are highly linked to suicide, approximately 25 to 50% will attempt suicide at least once over their lifetime [23,24], with 10 to 20% completing suicide [23,25,26]. They are also a disabling condition with loss of productivity, reduced occupational functioning and medical comorbidity leading to billions of dollars in healthcare costs [27-29].
The main treatment of these disorders are mood stabilizers, such as lithium, anticonvulsants, and antipsychotics, that should be continued indefinitely because of the risk of relapse [30,31]. Other symptomatic medication, like BZD, maybe prescribed to deal with acute psychiatric disturbances. While psychotherapy is of an important contribution, especially by educating patients and their relatives about relapse, suicidal thoughts, and the necessity of early intervention to prevent complications [32,33].
However, even with important advances in research about BD, many patients remain symptomatic in inter-critic period (between the episodes), with social and functional impairments [34,35]; and a lot of progress is expected to overcome these difficulties.
Benzodiazepines in bipolar disorders
Benzodiazepines are frequently prescribed for patients with BD. The use of BZD as adjunctive treatment in depressive episodes is common, especially to reduce associated anxiety, insomnia, and risk of suicide during the first days of treatment [36,37]. Benzodiazepines have also demonstrated efficacy for the acute management of mania [38,39] as adjuncts to mood stabilizers or antipsychotic drugs, to improve sleep and control anxiety, restlessness, agitation and aggressiveness [40,41]. However, there is less evidence supporting their adjunctive use in other situations, and during longer-term treatment of patients with BD [42]. Prescribing BZD is more frequent for patients with residual manic symptoms in bipolar I disorder, and BZD are usually used in difficult-to-treat, complex patients, with severe forms [42,43].
Few studies looked at the general effect of using BZD in patients with BD. Bipolar choice was a 6-month, randomized, multi-site comparison of a sample of 482 patients with bipolar I or II disorder. Authors found 138 (28.6%) BZD are users at baseline or follow-up. The researchers compared clinical measures, in BZD users and nonusers, including the Bipolar Inventory of Signs and Symptoms (BISS), Clinical Global Impressions-Bipolar scale (CGIBP) and Clinical Global Impression Efficacy Index (CGI-EI). Although both groups demonstrated improvement, BZD users experienced significantly less improvement in BISS and CGI-BP scores than non-users did. Moreover, the outcome measure in patients with comorbid anxiety or substance use disorders was not affected by BZD use [44].
Another study on the effect of BZD on BD had demonstrated that Patients, whose state requires BZD, may be at particularly high risk for recurrence of a mood episode. The Benzodiazepine use was linked to greater hazard of recurrence that persisted after adjustment for potential confounding variables, like anxiety comorbidity, anxiety symptoms and residual mood symptoms. Authors concluded that the need for BZD treatment in these patients may simply be a marker for severe form of illness, rather than indicating an effect of benzodiazepines on the outcome [42]. These findings highlight the fact that Practitioners use benzodiazepines to overcome the lack of alternatives in some difficult clinical situations.
Discussion
Benzodiazepines in bipolar inter – Critic period
As we reported earlier, BZD are often used in the handling of acute period of mood episodes, and their use in other situations is not clearly established. In inter-critic period, the use of BZD is generally the same as in non-bipolar patients. However, anxiety, sleep disturbances and substance use problems, which are frequent in patients with BD, may pose some particular problems with the use of these molecules.
Anxiety
Anxiety is very common in BD, nearly one in two patients has an anxiety disorder in their lifetime [45], elevated rates of anxiety disorders were found in patients with BD [46], increasing adverse outcomes such as suicidal behavior, impaired functioning, substance and alcohol misuse [47,48].
While using BZD to manage acute anxiety in patients with BD is accepted, their use is not recommended, as in general, to treat long-term anxiety. A major problem posed by the comorbidity of anxiety and BD is that antidepressants, used as core treatment for anxiety disorders, are known to induce manic switch and cycle acceleration in bipolar patients, especially if used without mood stabilizers [49]. In fact, there are few options to treat established anxiety disorders in this case, with scarce research in this area [50]. Some reports suggest the efficacy of the combination of olanzapine (Second generation antipsychotic) and fluoxetine (Selective serotonin reuptake inhibitor) [51], as well as quetiapine (atypical antipsychotic) [52,53], to reduce anxiety symptoms in bipolar patients. The limited proof for pharmacological treatment in this comorbidity has led to recommendations that psychotherapy, such as cognitive behavioral therapy, must be tried as first-line treatments [54]. However, it has not been shown to be of major effect [53].
The management of anxiety symptoms in BD is not well studied [55], and more investigation is needed to adopt an optimal approach for this comorbidity.
Sleep disturbances
Bipolar disorders and sleep disturbances are strongly linked. Reduced need for sleep is the most frequent symptom of mania, while insomnia or hypersomnia are common during depression episodes. Sleep may also be disturbed in the inter-critic period, with implications in both prodromal and syndromal phases of BD [56]. Insomnia is generally reported by 70% of BD patients [57,58].
Although depressive and manic episodes and inter-critic mood disturbances are thought to be linked to most of medical and social burden, recent evidences suggest that sleep disturbances play also a major role in these repercussions. In addition to being an important factor contributing to outbreak of BD [59], they are also responsible, at least in part, of functional and medical outcomes [60], especially by enhancing the risk for relapse and suicide attempts [61].
Sleep disturbances persist at high rates, despite adequate pharmacological and psychological interventions for BD [62].
The use of sedative antipsychotics, like chlorpromazine and levomepromazine, is frequent, but may lead to poorer functional improvement and to depressive mood [63,64]. Benzodiazepines are not a good solution for persistent sleep problems; nevertheless, they are efficacious for acute sleep disturbances in all the phases: mania, depression and inter-critic period [62]. In our practice, we have noticed that BZD may help to prevent relapse by handling acute sleep problems in stabilized bipolar patients, but studies are needed to confirm this clinical impression.
Psychological and lifestyle interventions may be preferred for their safety in term of side effects, for their durable action and the absence of abuse potential [62].
Substance abuse
Another situation, where BZD use may be problematic in BD, is substance abuse comorbidity. Bipolar disorders are associated with the highest rate of substance abuse among mood disorders [65]. In patients with BD, substance use disorders are related to an increased risk of relapse, rapid cycling and other negative consequences, including increased symptom severity [66] and poor treatment compliance [67,68], resulting in poor prognosis, and higher rates of utilization of acute services, leading to more costly care [69].
Studies have found that alcohol use disorder is present in about half of patients with BD, while 41% of this population present any other substance use disorder [70,71]. Concerning illegal drugs, cannabis is the most commonly used among patients with BD [72,73] estimates of use vary from 8% to 22%, and the life-time prevalence of its use is 30% to 64% [74]. Both alcohol and cannabis are known for their sedative and anxiolytic effects, therefore, bipolar patients in manic and depressive period may use them as self-medication [75]. Alcohol affects the GABA-benzodiazepine-chloride complex and has an agonist-like action [76].
Prescribing BZD in this population of patients, with bipolar and substance use disorders, must be done carefully, because of the high risk of misuse. On one hand, being addictive to a substance is a marker of susceptibility for other addictions, and in the other hand, the high prevalence of anxiety and sleep problems, that characterize people with substance use problems, may lead to long-term consumption of BZD [8,77].
The misuse of BZD, in combination with alcohol or other sedative substance, may create an additive effect, increasing central nervous system suppression, and causing physical and psychological repercussions [4,78-80]. Avoiding the use of benzodiazepines (or other sedative-hypnotics) in patients with alcohol problems should prevent many potential complications [81].
Conclusion
Although benzodiazepines have many benefits for patients with bipolar disorders, their use must be very cautious, because of the associated risk of misuse and other possible consequences, especially in some particular clinical situations. Concerns remain about efficacious alternatives to manage comorbid anxiety, sleep disturbances and substance use disorders. Despite the clinical importance of that issue, there is a lack of randomized studies due to ethical reasons. This situation highlights the need to explore more deeply this question, by naturalistic studies and neurobiological research, to better understand the role of BZD and GABAergic mechanisms in the pathophysiology of BD, anxiety and sleep disturbances.
Conflict of Interest
None.
REFERENCES
- Donoghue J, Lader M. Usage of benzodiazepines: A review. Int J Psychiatry Clin Pract. 2010 Jun;14(2):78-87.
- Lader M. Benzodiazepines revisited-Will we ever learn? Addiction 2011;106(12): 2086-109.
- Lader M. Benzodiazepine harm: How can it be reduced?. Br J Clin Pharmacol 2014;77(2):295-301.
- Lin SC, Chen CC, Chen YH, et al. Benzodiazepine prescription among patients with severe mental illness and co-occurring alcohol abuse/dependence in Taiwan. Hum Psychopharmacol 2011;26(3):201-207.
- Piparva KG, Parmar DM, Singh AP, et al. Drug utilization study of psychotropic drugs in outdoor patients in a teaching hospital. Indian J Psychol Med 2011;33(1): 54–58.
- Plante DT, Winkelman JW. Sleep disturbance in bipolar disorder: therapeutic implications. Am J Psychiatry 2008;165(7):830–843.
- Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Am J Psychiatry 2004;161(12): 2222-2229.
- Clark RE, Xie H, Brunette MF. Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry 2004;65(2):151–155.
- Wick JY. The history of benzodiazepines. Consult Pharm 2013;28(9):538-48.
- Kurko TA, Saastamoinen LK, Tähkäpää S. Long-term use of benzodiazepines: Definitions, prevalence and usage patterns - a systematic review of register-based studies. Eur Psychiatry 2015;30(8):1037-47.
- Poyares D, Guilleminault C, Ohayon MM, et al. Chronic benzodiazepine usage and withdrawal in insomnia patients. J Psychiatr Res 2004; 38: 327-34.
- Dikeos DC, Soldatos CR. The pharmacotherapy of insomnia: efficacy and rebound with hypnotic drugs. Primary Care Companion. J Clin Psychiatry 2002;4: (Suppl 1): 27-32.
- UK Department of Health and the Devolved Administrations. Drug misuse and dependence: UK Guidelines on Clinical Management. Department of Health, London, UK. 2007.
- Bourgeois J, Elseviers MM, Van Bortel L, et al. The impact of chronic benzodiazepine use on cognitive evolution in nursing home residents. Hum Psychopharma. 2015 Mar; 30(2):85-93.
- Lugoboni F, Mirijello A, Faccini M, et al. Quality of life in a cohort of high-dose benzodiazepine dependent patients. Drug Alcohol Depend. 2014 1;142:105-9
- Mur M, Portella MJ, Martínez-Arán A, et al. Long-term stability of cognitive impairment in bipolar disorder: A 2-year follow-up study of lithium-treated euthymic bipolar patients. J Clin Psychiatry 2008;69(5):712-719.
- Simonsen C, Sundet K, Vaskinn A, et al. Neurocognitive profiles in bipolar I and bipolar II disorder: differences in pattern and magnitude of dysfunction. Bipolar Disord 2008;10(2):245-255.
- Kripke DF, Langer RD, Kline LE. Hypnotic association with mortality or cancer; a matched cohort study. BMJ Open 2012; 2: e000850.
- Charlson F, Degenhardt L, McLaren J, et al. A systematic review of research examining benzodiazepine-related mortality. Pharmacoepidemiol Drug Saf 2009;18: 93–10
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC. 2013.
- Fassassi S, Vandeleur C, Aubry JM, et al. Prevalence and correlates of DSM-5 bipolar and related disorders and hyperthymic personality in the community. J Affect Disord 2014;167:198-205.
- Clemente AS, Diniz BS, Nicolato R, et al. Bipolar disorder prevalence: a systematic review and meta-analysis of the literature. Rev Bras Psiquiatr 2015;37(2):155-61.
- Latalova K, Kamaradova D, Prasko J. Suicide in bipolar disorder: A review. Psychiatr Danub 2014;26(2):108-14.
- Schaffer A, Isometsä ET, Tondo L, et al. Epidemiology, neurobiology and pharmacological interventions related to suicide deaths and suicide attempts in bipolar disorder: Part I of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. Aust N Z J Psychiatry 2015;49(9):785-802.
- Abreu LN, Lafer B, Baca-Garcia E, et al. Suicidal ideation and suicide attempts in bipolar disorder type I: an update for the clinician. Rev Bras Psiquiatr 2009;31(3):271-80.
- Parmentier C, Etain B, Yon L, et al. Clinical and dimensional characteristics of euthymic bipolar patients with or without suicidal behavior. Eur Psychiatry 2012;27(8):570-6.
- Kleine-Budde K, Touil E, Moock J, et al. Cost of illness for bipolar disorder: a systematic review of the economic burden. Bipolar Disord. 2014;16(4):337-53.
- Ekman M, Granström O, Omérov S, et al. The societal cost of bipolar disorder in Sweden. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1601-10.
- Somaiya M, Grover S, Chakrabarti S, et al. Comparative study of cost of care of outpatients with bipolar disorder and schizophrenia. Asian J Psychiatr 2014;12:125-33.
- Bellivier F, Delavest M, Coulomb S, et al. Therapeutic management of bipolar disorder in France and Europe: A multinational longitudinal study (WAVE-bd). Encephale 2014;40(5):392-400.
- Sachs GS. Decision tree for the treatment of bipolar disorder. J Clin Psychiatry 2003;64 Suppl 8:35-40.
- Zaretsky A. Targeted psychosocial interventions for bipolar disorder. Bipolar Disord 2003; 5 Suppl 2:80-87.
- Miklowitz DJ. A review of evidence-based psychosocial interventions for bipolar disorder. J Clin Psychiatry 2006;67 Suppl 11:28-33.
- Temmerman A, Sabbe B, Morrens M. Social cognition in bipolar disorder. Tijdschr Psychiatr 2015;57(6):405-14.
- Braw Y, Erez G, Sela T, et al. A longitudinal study of cognition in asymptomatic and mildly symptomatic bipolar disorder patients. Psychiatry Res. 2013;210(3):842-849.
- Morishita S. Clonazepam as a therapeutic adjunct to improve the management of depression. Nihon Shinkei Seishin Yakurigaku Zasshi. 2004;24(2):75-78.
- Tiller JW. Depression and anxiety. Med J Aust. 2013;199(6 Suppl):S28- S31.
- Bradwejn J, Shriqui C, Koszycki D, et al. Double-blind comparison of the effects of clonazepam and lorazepam in acute mania. J Clin Psychopharmacol 1990;10(6):403-408.
- Edwards R, Stephenson U, Flewett T. Clonazepam in acute mania: A double blind trial. Aust N Z J Psychiatry 1991;25(2):238-242.
- Chouinard G. Issues in the clinical use of benzodiazepines: potency, withdrawal, and rebound. J Clin Psychiatry 2004;65 Suppl 5:7-12.
- Malhi GS, Tanious M, Berk M. Mania: diagnosis and treatment recommendations. Curr Psychiatry Rep 2012;14(6):676-86.
- Perlis RH, Ostacher MJ, Miklowitz DJ, et al. Benzodiazepine use and risk of recurrence in bipolar disorder: A STEP-BD report. J Clin Psychiatry 2010;71(2):194-200
- Bobo WV, Reilly-Harrington NA, Ketter TA, et al. Complexity of illness and adjunctive benzodiazepine use in outpatients with bipolar I or II disorder: results from the Bipolar CHOICE study. J Clin Psychopharmacol 2015;35(1):68-74.
- Bobo WV, Reilly-Harrington NA, Ketter TA, et al. Effect of adjunctive benzodiazepines on clinical outcomes in lithium- or quetiapine-treated outpatients with bipolar I or II disorder: results from the Bipolar CHOICE trial. J Affect Disord 2014;161:30-5.
- Pavlova B, Perlis RH, Alda M, et al. Lifetime prevalence of anxiety disorders in people with bipolar disorder: A systematic review and meta-analysis. Lancet Psychiatry 2015;2(8):710-717.
- Goes FS. The importance of anxiety states in bipolar disorder. Curr Psychiatry Rep 2015;17(2):3.
- Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry 2007;64:543-52.
- Goes FS, McCusker MG, Bienvenu OJ, et al. Co-morbid anxiety disorders in bipolar disorder and major depression: familial aggregation and clinical characteristics of co-morbid panic disorder, social phobia, specific phobia and obsessive-compulsive disorder. Psychol Med 2012;42:1449-59
- El-Mallakh RS, Vöhringer PA, Ostacher MM, et al. Antidepressants worsen rapid-cycling course in bipolar depression: A STEP-BD randomized clinical trial. J Affect Disord 2015;184:318-21.
- Mitchell PB. Bipolar disorder and anxiety: A comorbidity needing better treatments. Lancet Psychiatry 2015;2(8):671-672.
- Tohen M, Calabrese J, Vieta E, et al. Effect of comorbid anxiety on treatment response in bipolar depression. J Affect Disord 2007;104:137-46.
- Lydiard RB, Culpepper L, Schioler H, et al. Quetiapine monotherapy as treatment for anxiety symptoms in patients with bipolar depression: a pooled analysis of results from 2 double-blind, randomized, placebo-controlled studies. Primary Care Companion. J Clin Psychiatry 2009;11:215-25.
- Sheehan DV, Harnett-Sheehan K, Hidalgo RB, et al. Randomized placebo-controlled trial of quetiapine XR and divalproex ER monotherapies in the treatment of the anxious bipolar patient. J Affect Disord 2013;145: 83-94.
- Rakofsky JJ, Dunlop BW. Treating nonspecific anxiety and anxiety disorders in patients with bipolar disorder: A review. J Clin Psychiatry 2011;72:81-90.
- Hirschfeld RA, Bowden CL, Gitlin MJ, et al. Practice Guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry 2002;159(suppl 4):1-50.
- Brill S, Penagaluri P, Roberts RJ, et al. Sleep disturbances in euthymic bipolar patients. Ann Clin Psychiatry 2011;23(2):113-6.
- Harvey AG, Schmidt DA, Scarna A, et al. Sleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia, and subjects without sleep problems. American Journal of Psychiatry 2005;162:50-57
- Soreca I. Circadian rhythms and sleep in bipolar disorder: implications for pathophysiology and treatment. Curr Opin Psychiatry 2014;27(6):467-71.
- Harvey AG, Soehner AM, Kaplan KA, et al. Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: A pilot randomized controlled trial. J Consult Clin Psychol 2015;83(3):564-77.
- Soreca I, Frank E, Kupfer DJ. The phenomenology of bipolar disorder: what drives the high rate of medical burden and determines long-term prognosis?. Depress Anxiety 2009;26:73-82.
- Sylvia LG, Dupuy JM, Ostacher MJ, et al. Sleep disturbance in euthymic bipolar patients. J Psychopharmacol 2012;26(8):1108-12.
- Harvey AG, Kaplan KA, Soehner AM. Interventions for sleep disturbance in bipolar disorder. Sleep Med Clin 2015;10(1):101-5.
- Kane JM, Sharif ZA. Atypical antipsychotics: Sedation versus efficacy. J Clin Psychiatry 2008;69 Suppl 1:18-31.
- Yen CF, Cheng CP, Huang CF, et al. Quality of life and its association with insight, adverse effects of medication and use of atypical antipsychotics in patients with bipolar disorder and schizophrenia in remission. Bipolar Disord 2008;10(5):617-24.
- Bally N, Zullino D, Aubry JM. Cannabis use and first manic episode. J Affect Disord 2014;165:103-8.
- Van Rossum I, Boomsma M, Tenback D, et al. Does Cannabis use affect treatment outcome in bipolar disorder? A longitudinal analysis. The Journal of Nervous and Mental Disease 2009;197(1):35-40.
- González-Pinto A, Reed C, Novick D, et al. Assessment of medication adherence in a cohort of patients with bipolar disorder. Pharmacopsychiatry 2010;43(7):263-70.
- Carvalho AF, Dimellis D, Gonda X, et al. Rapid cycling in bipolar disorder: A systematic review. J Clin Psychiatry 2014;75(6):e578-86.
- RachBeisel J, Scott J, Dixon L. Co-occurring severe mental illness and substance use disorders: A review of recent research. Psychiatr Serv 1999;50(11):1427-34.
- Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA 1990;264(19):2511-8.
- Cerullo MA, Strakowski SM. The prevalence and significance of substance use disorders in bipolar type I and II disorder. Subst Abuse Treat Prev Policy 2007;2:29
- Leweke FM, Koethe D. Cannabis and psychiatric disorders: It is not only addiction. Addict Biol 2008;13(2):264-75.
- Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disorders 2001;3(4):181-188.
- Brown ES, Suppes T, Adinoff B, et al. Drug abuse and bipolar disorder: comorbidity or misdiagnosis? Journal of Affective Disorders 2001;65(2):105-115.
- Tyler E, Jones S, Black N, et al. The relationship between bipolar disorder and cannabis use in daily life: An experience sampling study. PLoS One. 2015;10(3):e0118916.
- Linnoila MI. Benzodiazepines and alcohol. J Psychiatr Res. 1990;24 Suppl 2:121-7
- Vorspan F, Mehtelli W, Dupuy G, et al. Anxiety and substance use disorders: co-occurrence and clinical issues. Curr Psychiatry Rep 2015;17(2):4.
- Ogbu UC, Lotfipour S, Chakravarthy B. Polysubstance abuse: alcohol, opioids and benzodiazepines require coordinated engagement by society, patients, and physicians. West J Emerg Med 2015;16(1):76-9.
- Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Research & Health. Vol. 23, No. 1, 1999: 40-51.
- Jones JD, Mogali S, Comer SD. Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug Alcohol Depend 2012;125(1-2):8-18.
- Hollister LE. Interactions between alcohol and benzodiazepines. Recent Dev Alcohol 1990;8:233-9.