Three Unusual Variations of the Testicular Vasculature in a Single Cadaver: Case Report and Short Review of Pathophysiologic Correlations with Varicocele
Received: 03-Jun-2022, Manuscript No. ijav-22-5021; Editor assigned: 06-Jun-2022, Pre QC No. ijav-22-5021 (PQ); Accepted Date: Jun 23, 2022; Reviewed: 20-Jun-2022 QC No. ijav-22-5021; Revised: 23-Jun-2022, Manuscript No. ijav-22-5021 (R); Published: 30-Jun-2022, DOI: 10.37532/1308-4038.15(6).201
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
During the dissection of an 80-year-old male cadaver, the following three unusual variations of testicular vasculature were encountered: 1) bilateral anonymous descending retroperitoneal veins that drained into the testicular veins, 2) bifurcated left testicular vein that drained into the left renal vein and 3) a branch of left testicular artery that entered the hilum of the left kidney. The co-occurrence of multiple variations like this could be potential risks for various medical conditions including varicocele and varicocele associated male subfertility or infertility. These could also affect the interpretation of outcomes of interventional radiological procedures and increase the risk of complications during vascular, renal and urologic surgeries. So, awareness of such variations would play a crucial role in the diagnosis and differential diagnosis of causes of male infertility, urologic diseases, and in the planning and deployment of appropriate radiologic and surgical strategies to reduce the risk of iatrogenic complications.
Keywords
Testicular vein; Retroperitoneal vein; Testicular artery; Renal vein; Varicocele
Introduction
The testicular (internal spermatic) veins are the major drainage routes for venous blood from the testes and epididymides to the inferior vena cava on the right side and to left renal vein on the left side [1]. They present with variable numbers, communications and termination patterns. Particularly, the left testicular vein that drains into the left renal vein can be bifurcated with an oblique communication between its branches [2], can provide a branch that drains into the second lumbar vein [3], can be double [4] and can also have unusual communications with the colonic veins [5]. The testicular veins and the pampiniform plexus that surround the testicular arteries provide a countercurrent heat exchange mechanism that cools the testicular arterial blood as it reaches the testis. This mechanism, together with the cremaster and dartos muscles, therefore, helps to regulate the optimum temperature for spermatogenesis [6]. Varicosis of the testicular veins and the pampiniform plexuses (varicocele), which is more frequent on the left side than the right, is a significant risk factor in the causation of male subfertility or infertility by adversely affecting the heat exchange mechanism. Varicocele particularly causes elevated scrotal temperature (heat stress) with a consequent impairment of spermatogenesis [7], hypogonadism [8] and BPH [9].
The testicular veins are also clinically important for they can be used in different clinical procedures including the lengthening of renal vein during kidney transplantation, laparoscopic varicocelectomy and also serve as entry portal for percutaneous retrograde varicocele embolization [10]. The variability of the testicular veins is also of considerable importance in the rarely performed and controversial testicular transplantation procedure from a male identical twin donor [11].
The testicular arteries are paired branches of the anterolateral aspect of the abdominal aorta. These arteries can also originate from unusual spots on the abdominal aorta or from the renal arteries, accessory renal arteries, suprarenal arteries, lumbar arteries and rarely from the common iliac, internal iliac or inferior epigastric arteries [12]. The testicular arteries can also originate by a common stem with the inferior suprarenal arteries from the abdominal aorta showing a wide range of variabilities, which are found almost exclusively on the left side [12]. For the testicular vessels are closely related to the renal vessels, suprarenal vessels, the kidneys, renal pelvises and the ureters, the knowledge of variations of these vessels is of immense clinical importance during renal transplantation, vascular surgeries and interventional radiological procedures.
Materials and Methods
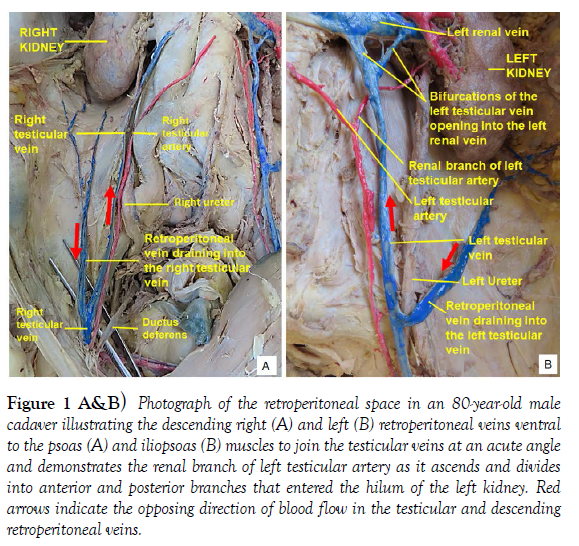
During the dissection study of the retroperitoneal space of an 80-year-old male cadaver, three unusual variations of the testicular vasculature were noted. The vessels were carefully dissected, cleaned and painted red (for arteries) and blue (for veins) and photographs were taken for illustrations.
CASE REPORT
The observed testicular vascular variations consisted of:
1. Bilateral anonymous descending retroperitoneal veins formed by the confluence of multiple small veins of the posterior abdominal wall that descended ventral to the psoas muscle on the right side and the iliopsoas muscle on the left side. These veins joined the testicular veins of the respective side at a caudally directed acute angle, which is more pronounced on the right side (Figure 1 A and B). The right testicular vein is joined by the descending retroperitoneal vein short after it entered the abdomen through the deep inguinal ring, while on the left side it opened into the left testicular vein higher up near the point where the testicular vein crossed from medial to lateral ventral to the left ureter (Figure 1 A and B).
2. Bifurcated left testicular vein into diverging larger medial and smaller lateral divisions that joined the left renal vein independently. The larger medial branch joint the left renal vein short after it crossed over the abdominal aorta and the smaller lateral branch joined it close to the left renal hilum (Figure 1B).
3. A small branch of the left testicular artery ascended dorsal to the left testicular vein and the branches of the left renal artery and vein, and then divided into anterior and posterior branches that ran on the respective sides of the renal pelvis to enter the hilum of the left kidney (Figure 1B).
Figure 1 A&B: Photograph of the retroperitoneal space in an 80-year-old male cadaver illustrating the descending right (A) and left (B) retroperitoneal veins ventral to the psoas (A) and iliopsoas (B) muscles to join the testicular veins at an acute angle and demonstrates the renal branch of left testicular artery as it ascends and divides into anterior and posterior branches that entered the hilum of the left kidney. Red arrows indicate the opposing direction of blood flow in the testicular and descending retroperitoneal veins.
Discussion
As revealed by many studies and reports, variabilities in the termination, number and communication patterns of the testicular veins are very common [1]. A previous case report revealed a bifurcated left testicular vein into right and left branches that terminated in the left renal vein. These branches were interconnected by an oblique communicating branch [2]. The bifurcation or division pattern of the left testicular vein into medial and lateral divisions in the present case report is similar to the above report but there is a significant size difference between the divisions (larger medial and smaller lateral divisions) and no communication between the branches was observed between the divisions. Another case report also described a similar division of the left testicular vein with a different drainage pattern of its divisions, where the medial division ended in the left renal vein and the lateral division drained into the second lumbar vein [3]. The reported lateral division appears to have similarity to the left anonymous descending retroperitoneal vein in the present case report but the author of the current report considers the descending retroperitoneal veins as tributaries draining into the testicular veins rather than divisions from the testicular veins joining other veins. According to the current observation these descending retroperitoneal veins are unusual and bilateral veins draining venous blood from the posterior abdominal wall into the testicular veins at acute angles. The additional blood carried by these veins into the testicular veins could raise the intravenous hydrostatic pressure and could possibly increase the risk of varicocele. In relation to this pattern of drainage, according to the law of physics, I believe that the additional drainage of blood from the almost vertically oriented veins from the posterior abdominal wall into the testicular veins at a caudally directed acute angle of drainage in the direction of gravity or against the stream of blood flow in the testicular veins (counter current flow of fluids), would potentially slow the normal flow of blood in the testicular veins (counter current flow limitation or CCFL) and this at the mean time could increase the volume of blood in the testicular veins consequently leading to increased intravenous hydrostatic pressure. This could also affect the valvular competence in the testicular veins enhancing retrograde flow (reflux) and pooling of blood in the pampiniform plexus increasing the risk of varicocele with its consequent complications. Additionally, if such unusual veins draining into the testicular veins in the abdomen are missed during laparoscopic varicocelectomy through retroperitoneal approach (Palomo’s procedure) they could increase the risk of varicocele recurrence.
Though it can occur bilaterally, left sided varicocele is predominant and is associated with elevated scrotal temperature causing various complications [6]. Such complications can occur in males of any age presenting with primary infertility (35%) or secondary infertility (80%) [6]. The varicocele associated raised intrascrotal temperature causes heat stress that results in oxidative stress and excessive reactive oxygen species formation affecting the rate of spermatogenesis and increased apoptosis/DNA degeneration with consequent male infertility [6]. As it was explained in a review study on varicocele and testicular function; varicocele plays a detrimental impact on Sertoli and Leydig cells of the testis. It is associated with decreased responsiveness of Sertoli cells to FSH and altered androgen binding protein, transferrin and inhibin levels leading to decreased testosterone production. It also causes cytoplasmic vacuolization, atrophy and reduction in the number of Leydig cells associated with decreased level of testosterone [7, 8]. A study done on 901 patients with BPH, demonstrated that there is a straightforward pathophysiologic connection between varicocele and BPH. According to this study, the refluxed venous blood rich in free-testosterone is diverted directly to the prostate via the testicular-prostatic venous communications and accelerates the rate of prostatic cell production and prolongation of cellular life span increasing the prostatic cell population leading to BPH [9].
Testicular arterial variations are also frequently reported. As a previously published research work on 42 cadavers demonstrated almost all the testicular arterial variations occurred on the left side. One of the encountered variations was that the testicular artery provided a suprarenal branch and continued farther as the proper testicular artery [12]. Even though the variant finding in this current report is also on the left side, the branch that is given off of the testicular artery differs in that it did not extend to the suprarenal gland, rather divided into anterior and posterior branches that entered the left kidney running on the respective sides of the renal pelvis. No documentation describing such a branch of testicular artery to the kidney(s) similar to the finding in this case report is found in the review of literature. I, the author of this report, believe that the sharing of the testicular arterial blood through unusual branches like in this case, could possibly reduce the arterial blood flow to the testis increasing the risk of hypoxia, oxidative stress and testicular atrophy which can add up to the complications caused by the varicocele.
Moreover, due to the close relationship with the kidney and its hilar structures including renal vessels and renal pelvis and the ureters; the knowledge of testicular venous and arterial variations is of immense clinical importance during renal transplantation, vascular surgeries and interventional radiological procedures.
Conclusion
The co-occurrence of testicular vascular variations could be potential risk factor for various clinical conditions like varicocele, which is frequently associated with male subfertility or infertility. Multiple variations like these could also affect the interpretations of outcomes of procedures like interventional radiology. So, awareness of such variations would help in the differential diagnosis of causes of male fertility disorders, urologic diseases, and in the planning and deployment of appropriate radiologic and surgical strategies to reduce the risk of complications during and after treatment of varicocele, renal transplantation, endovascular repair of abdominal aortic aneurysm and other nephron-urologic surgeries.
Acknowledgement
I am thankful to the donor and her families for their invaluable donation and consent for education, research and publication. My thanks also go to the department of biomedical sciences for the encouragement and uninterrupted support. I am also grateful to Denelle Kees, Chelsey Swanson and John Opland for their immense assistance during the dissection of this cadaver in the gross anatomy lab.
REFERENCES
- Malar D. A study of variations of testicular vein and its clinical significance. Int J Anat Res. 2016; 4(1): 1985 – 87.
- Nayak SB, Padur AA, Kumar N, Reghunathan D, et al. Terminal bifurcation and unusual communication of left testicular vein with left suprarenal vein. J Vasc Bras. 2017; 16 (2): 174 – 177.
- Oliveira GVd, Nascimento LADd, Souza MV, Vargas R, et al. Uncommon drainage of left testicular vein. Eur.J. Anat. 2018; 22(4): 367 - 369.
- Dey S, Kundu B, Bhakta A. A study on numeric variation of gonadal veins in eastern India: Embryological aspect and its implication. IOSR J Den Med Sci. 2018; 16 (1): 72 – 74.
- Favorito LA, Costa WS, Sampaio FJB. Applied anatomic study of testicular veins in adult cadavers and in human fetuses. Int Braz J Urol. 2007; 33: 176 – 80.
- Islam SR, Islam M, Sarkar SA, Paran S. Outcome of laparoscopic varicocelectomy with mass ligation technique for symptomatic varicocele. Arch Surg Clin Res. 2019; 3: 065 – 069.
- Pastuszak AW, Wang R. Varicocele and testicular function. Asian J Androl. 2015; 17:659 -667.
- Saylam B, Cayan S, Akbay E. Effect of microsurgical varicocele repair on sexual functions and testosterone in hypogonadal men with varicocele. The Aging Male. 2020; 23(5): 1366 – 1373.
- Goren M, Gat Y. Varicocele is the root cause of BPH: Destruction of valves in the spermatic veins produces elevated pressure which diverts undiluted testosterone directly from the testes to the prostate. Andrologia. 2018; 50: e12992.
- Lalwani R, Athavale SA, Chauhan K, Nigam GL, et al. Cadaveric study of mode of termination of gonadal veins: implications for procedures utilizing terminal ends of the gonadal veins as entry portal. J Nat Sci Biol Med. 2017; 8 (2): 210 – 212.
- Donati-Bourne J, Roberts HW, Rajjoub Y, Coleman RA, et al. A review of transplantation practice of urologic organs: Is it only achievable for the kidney? Rev Urol. 2015; 17(2): 69 - 77.
- Kortian SR, Pandey AK, Padmashali S, Jaison J, Kalthur SG. A cadaveric study of testicular artery and its clinical importance. J Vasc Bras. 2016; 15(4): 280 – 286.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref